Purpose
To validate a scale for grading vitreous haze in uveitis using digitized photographs and standardized scoring.
Design
Evaluation of clinical research methodology.
Methods
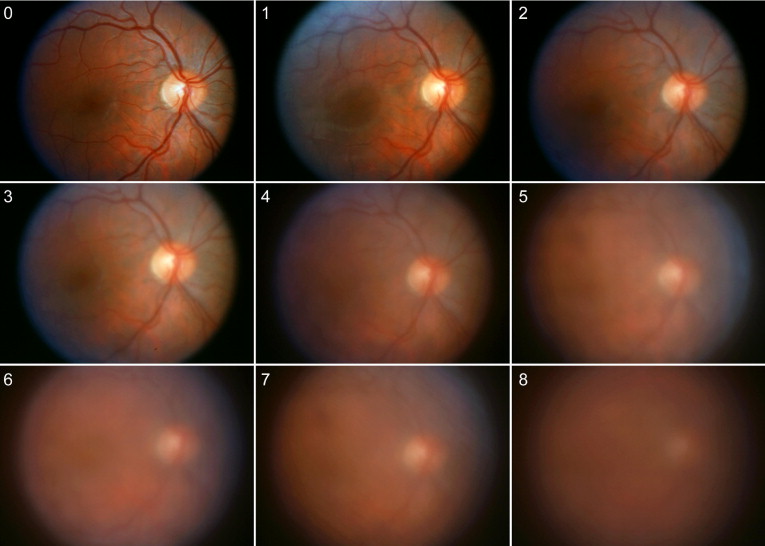
Calibrated Bangerter diffusion filters inducing incremental decrements of spatial contrast were placed in front of the camera lens while photographing a normal eye to simulate vitreous haze. The photographs were digitized and an ordinal scale was created from 0 (none) to 8 (highest level of opacification at which fundus details could be seen). The scale steps correspond approximately to decimal Snellen visual acuities of 1.0, 0.8, 0.4, 0.2, 0.1, 0.04, 0.02, 0.01, and 0.002, with approximately 0.3 log step between each step. For validation, digitized fundus photographs of uveitis patients were displayed on a computer monitor for comparison with the standard photos. Three observers graded the test set twice under standard conditions. Interobserver and intraobserver variability and κ values for agreement greater than chance were calculated.
Results
Variance component analysis determined that 87.7% of the variance in grades was attributable to the test item rather than to grader or session. The intraclass correlation between graders and grading sessions varied from 0.84 to 0.91. Simple agreement within 1 grade between graders and sessions occurred in 90 ± 5.5% of gradings. κ values averaged 0.91, which is considered near perfect.
Conclusions
A 9-step photographic scale was designed to standardize the grading of vitreous haze in uveitis patients using fundus photographs. The scale is potentially adaptable to clinical trials in uveitis.
Grading of intraocular inflammation using cell counts in the aqueous humor and anterior vitreous and a subjective assessment of anterior chamber flare was described first in 1959. These measures recently have been standardized in a consensus document. Vitreous haze is the obscuration of fundus details by vitreous cells and protein exudation. It impacts vision more profoundly than anterior inflammation and therefore is used commonly as an outcome measure for clinical trials involving intermediate, posterior, or panuveitis.
Kimura and associates proposed a 5-level scale of vitreous haze based on the ophthalmoscopic clarity of the ocular fundus in 1959. To improve grading reproducibility for clinical trials, Nussenblatt and associates published clinical photographs illustrating 6 grades of vitreous haze in 1985. Visibility of the optic nerve head, retinal vessels, and nerve fiber layer defined the scale grades. The Nussenblatt scale has been used widely, and the Standardization of Uveitis Nomenclature Working Group consensus document on uveitis nomenclature accepted the scale for grading vitreous haze in 2005, with the exception that the grade of trace was converted to 0.5+ to allow numeric scoring. It is easy to use, reproducible, and currently accepted by the Food and Drug Administration for use in clinical trials.
There are disadvantages of the current scale. Intervals between grades are not quantified. Demonstrating a 2-step change in grade in a clinical trial can be difficult, given the relatively small number of grades of vitreous haze and the relatively poor discrimination of lower levels of haze, which are more common in uveitis than the higher grades of haze. Finally, the scale is not validated as a standard for grading fundus photographs. We propose a method of photographic grading of vitreous haze using a 9-level scale created by photographing a normal fundus through Bangerter occlusion filters to create increasing optical blur, simulating increasing vitreous haze.
Methods
Scale Creation
Bangerter occlusion filters or foils are used in the treatment of amblyopia as an alternative to atropine or patching. They degrade visual acuity and contrast sensitivity stepwise and are calibrated to Snellen visual acuities. The foils are made of plastic and are cut easily for mounting. Bangerter Filters (Haag-Streit, Koeniz, Switzerland) were used singly or in combination to create a 9-point scale separated by approximately 0.3 log units of spatial resolution, equivalent to a doubling of the visual angle. Grade 0 had no superimposed filter. Haze grades 1, 2, 3, and 4 used 0.8, 0.4, 0.2, and 0.1 filters, respectively. Haze grades 5, 6, and 7 were achieved by overlaying the 0.1 filter on the 0.4, 0.2, and 0.1 filters, respectively. Grade 8 was an overlay of two 0.1 filters and the 0.2 filter. The 4 composite filters were estimated to correspond to visual acuities of 20/400, 20/1000, 20/2000, and 20/5000 ( Table 1 ). Visual acuities through the actual filter combinations used were not verified.
| Haze Scale Value | Bangerter Filter | Estimated Snellen Acuity | LogMAR Equivalent |
|---|---|---|---|
| 0 | None | 20/20 | 0 |
| 1 | 0.8 | 20/25 | 0.1 |
| 2 | 0.4 | 20/50 | 0.4 |
| 3 | 0.2 | 20/100 | 0.7 |
| 4 | 0.1 | 20/200 | 1 |
| 5 | 0.1*0.4 | 20/400 | 1.3 |
| 6 | 0.1*0.2 | 20/1000 | 1.7 |
| 7 | 0.1*0.1 | 20/2000 | 2 |
| 8 | 0.1*0.1*0.2 | 20/5000 | 2.7 |
Grade 0 photographs of the normal fundus of a 20-year-old volunteer were obtained without a filter with a 30-degree Zeiss fundus camera model FF4 (Carl Zeiss Meditec, Inc, Pleasanton, California, USA) with a Nikon film camera (Nikon Instruments Inc, Melville, New York, USA) loaded with Fuji-chrome 100 ASA film. Bangerter occlusion filter single and combined filters of increasing density then were suspended before the front aperture of the camera and the best photographs were selected. The film slides subsequently were digitized with a Nikon film scanner at 24-bit color and resolution of 300 dpi. Images were saved as tagged image file format (TIF). A set of 9 standard photographs with incremental optical blur was created ( Figure 1 ). Level 0 corresponds to no haze and level 8 to maximum haze. A theoretical level 9 corresponds to haze greater than 8, creating a 10-point scale.
Scale Validation
Ninety-seven color film fundus photographs of patients with uveitis were selected from the photographic archives. Patients with significant cataracts and prominent fundus pathologic features were excluded. Levels of vitreous haze ranging from clear to total opacification were included in the set. The color slides were digitized as described above.
Preliminary validation was performed with the images projected in an auditorium with 25 graders at different levels of ophthalmologic training who were asked to compare the pictures to a hard copy print of the standards and to record the grade on a grade sheet. The standard photos were projected simultaneously one by one in dual projection adjacent to the test photograph. Each test photograph was scored on a scale from 0 through 8. Grading took approximately 40 minutes.
Subsequently, an interactive graphical user interface using a web browser was designed to allow simultaneous online comparison of the 9 standard photographs with the same set of 97 test photographs and refined as a Windows application (Microsoft, Redmond, Washington, USA). Three retina fellows graded the set twice at a 2-month interval on the same computer monitor under constant lighting conditions after reading a brief paragraph about how to use the grader. The score was recorded online during the grading. Grading took approximately 20 minutes per session.
Statistical Evaluation
Intraclass and interclass correlation coefficients were calculated to assess overall agreement for all graders and then for the 3 graders over 2 grading sessions. Variance component analysis was performed to identify the sources of variability.
Agreement between graders also was evaluated with a distribution of their differences in grading scores, and agreement within graders was evaluated with a distribution of differences between each grader’s first and second grading. κ statistics estimated the excess chance of both exact agreement and agreement within 1 grade. Because the grading scale is ordinal, a weighted κ value was used, which awards credit for exact or nonexact matches according to the formula:
1 − ( ( differences between ratings ) / ( maximum difference between ratings ) ) . 7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


