Purpose
To evaluate the visual performance and rotational stability of the Tecnis Toric 1-piece intraocular lens (IOL) during the first 3 postoperative months.
Design
Prospective, single-center study.
Methods
In this study, patients with age-related cataract and corneal astigmatism of 1.0 to 3.0 diopters measured with the IOLMaster 500 (Carl Zeiss Meditec AG) were included. Before surgery, rotating Scheimpflug scans (Pentacam HR; Oculus) were performed and the cornea was marked in the sitting position at the slit lamp. Patients received a single-piece toric hydrophobic acrylic IOL (Tecnis Toric; AMO). Immediately and 3 months after surgery, retroillumination photographs were obtained to assess the rotational stability of the IOL. Additionally, Autorefraction (Topcon), subjective refraction, uncorrected and distance-corrected visual acuity, keratometry, and Scheimpflug and ocular wavefront (WASCA, Carl Zeiss Meditec AG) measurements were performed at the 3-month follow-up.
Results
Thirty eyes of 30 patients were included in this study. Mean absolute difference between the IOL axis at the 3-month and 1-hour follow-up was 2.7 degrees (standard deviation, 3.0 degrees). The IOL rotation was less than 3 degrees and less than 6 degrees in 62% and 95% of all cases, respectively.
Conclusions
The Tecnis Toric 1-piece IOL is rotationally stable and shows excellent capsule bag performance and refractive outcomes.
Many of the first designs of toric intraocular lenses (IOLs) in the early 1990s showed an IOL rotation of more than 30 degrees in one fifth of the patients. By contrast, modern toric IOLs typically show a mean absolute rotation of 3 to 5 degrees, which would result in a loss of approximately 10% to 15% of the astigmatism-reducing effect of the toric IOL.
The rotational stability of a toric IOL is determined by the interaction between the toric IOL and the capsule bag. The misalignment of the toric IOL, however, depends on several other factors in addition to rotational stability. In the current study, misalignment is defined as the difference between the intended axis of the toric IOL and the actual axis, measured 3 months after surgery.
During surgery, misalignment can occur because of cyclotorsion of the eye (resulting from the supine position of the patient or from peribulbar anaesthesia), imprecision of the surgeon when positioning the IOL relative to the intended meridian, or both. Both of these factors can be controlled more precisely by marking the eye before surgery with the patient in the sitting position and by diligence on the part of the surgeon.
After surgery, the IOL may rotate because it is either undersized for the capsule bag or because of capsule shrinkage during fibrotic contraction of the capsule bag during the postoperative period. Most current IOLs are slightly oversized for the capsule bag; therefore, the former is observed rarely and would be more likely in long eyes, which tend to have a larger capsule bag diameter. However, capsule bag shrinkage is thought to induce rotation in IOLs with open-loop haptics because of the asymmetry of the haptic design. Typical IOL haptic designs that improve rotational stability are either plate haptic IOLs or special Z-haptic–shaped open-loop haptics that are designed to counteract the rotational effect of compression of the shrinking bag. Disadvantages are associated with both of these IOL designs, however. Plate haptic IOLs have an increased risk of posterior capsule opacification because of a less effective lens epithelial barrier effect of the optic edge. Additionally, this design may show more rotation immediately after surgery because of a shorter haptic length. The Z-haptic IOL, however, is cumbersome to implant and is prone to damage during implantation. With the limitations of current IOL haptic designs in mind, the aim of the present study was to evaluate the rotational stability of a novel single-piece hydrophobic acrylic toric IOL with an open-loop haptic design.
Methods
The trial was approved by the Ethics Committee of the City of Vienna and adhered to the tenets of the Declaration of Helsinki. All patients signed an informed consent form prior to taking part in the study. In this prospective study, patients with age-related cataract and corneal astigmatism were included. The inclusion criteria were cataract and corneal astigmatism of between 1.0 and 3.0 diopters (D) on autokeratometry (IOLMaster 500; Carl Zeiss Meditec AG, Jena, Germany). Exclusion criteria included irregular astigmatism such as forme fruste keratoconus, corneal scars, phacodonesis, pseudoexfoliation syndrome, traumatic cataract, and any other ophthalmic pathologic features that may impact postoperative visual function.
The single-piece hydrophobic acrylic toric IOL (Toric Tecnis; AMO, Abbott Park, Illinois, USA) of the current investigation has an optic diameter of 6.0 mm and an overall diameter of 13.0 mm with open-loop haptics. The optic is aspherical and has an ultraviolet filter and a 360-degree sharp optic edge to prevent posterior capsule opacification.
On the day of preoperative assessment, patients underwent a full ophthalmic examination, and optical biometry was performed using the IOLMaster 500. Additionally, corneal topography using a Placido system (Atlas; Carl Zeiss Meditec AG) and corneal tomography using Scheimpflug technology (Galilei; Ziemer, Switzerland) were performed. A toric IOL was implanted only if all 3 methods yielded values that were within 0.5 D and 10 degrees of each other.
Toric power calculation software (Abbott Medical Optics, USA; available at https://www.amoeasy.com/calc ) was used for calculating the toric power and the meridian for IOL alignment. A surgically induced astigmatism value of 0.3 D was entered for calculation, and the steep meridian of the cornea was used for the incision position. This surgically induced astigmatism value was determined by using values collected from a previous study using the Naeser method, wherein the nontoric model of the same IOL and the same incision type and size were used. In cases where the axial eye length was 22.0 mm or more, the spherical IOL power was calculated on the IOLMaster 500 using the SRK-T (Sanders-Retzlaff-Kraff-theoretical) formula. If the axial eye length was shorter, the HofferQ formula was used. The intended postoperative refraction was chosen to be between 0.0 and −0.5 D for the sphere and between −0.1 and −0.5 D for the cylinder power to avoid axis flip of the astigmatism.
Before surgery, the horizontal meridian was marked with the patient in the sitting position at the slit lamp. We ensured that the patient’s head was straight in the chin rest by focusing the horizontally oriented slit of the slit lamp at the first Purkinjemeter reflex of the fellow eye, then moving the slit beam to the study eye without changing the vertical position of the slit lamp. The marking process continued only if the first Purkinjemeter reflex of both eyes was at the same horizontal level; otherwise, the patient’s head was repositioned and the process was begun again. Using an insulin needle, small superficial incisions were made on the limbus at the 3- and 9-o’clock positions. Care was taken to center the slit beam on the center of the pupil for alignment. For better visibility during surgery, the incisions were highlighted with a sterile blue marking pen. Finally, the correct position was verified by the observer at the slit lamp. If one of the markings was slightly off, this was recorded on the case report form to inform the surgeon before positioning the corneal marker during surgery.
Surgery was performed under topical anaesthesia in all cases by 2 experienced surgeons. To ensure uniformity of the incision axis, a temporal self-sealing incision was made in every study eye using a 2.8-mm single-bevelled steel blade. The incision was followed by the injection of an ophthalmic viscoelastic device (OVD), capsulorrhexis, phacoemulsification, irrigation and aspiration of cortical material, and injection of a cohesive OVD (Healon; Abbott Medical Optics) into the capsular bag as standard procedure. After aligning a corneal marking ring (Mendez marker; Duckworth & Kent, Hertfordshire, United Kingdom) with the preoperative markings, the planned meridian was marked with blue pen dots. The IOL was implanted into the capsule bag using the Emerald AR injector (Abbott Medical Optics). After implantation, the toric axis was positioned approximately 20 degrees counter clockwise from the planned meridian by rotating the IOL. The OVD then was aspirated thoroughly using a bimanual irrigation/aspiration set. Special care was taken to remove the OVD completely from behind the IOL by slightly displacing and tilting it while reaching behind the optic with the aspiration cannula. After this, the markings of the toric IOL were aligned to the corneal markings. A last check for accuracy of placement was carried out after filling the anterior chamber and hydrating the incisions, and final alignment was made using the corneal marking ring and a 30-gauge cannula through a paracentesis.
Retroillumination photography was performed at both 1 hour and at 3 months after surgery with a high-resolution digital retroillumination imaging system. The optical system consists of a slit lamp and a fiberoptic cable light source (Carl Zeiss Meditec AG). This system allows coaxial illumination and imaging with a digital color camera (Canon Incorporation, Tokio, Japan, EOS 5D Mark II) connected to the system. The images were transferred directly to a personal computer and were saved to the hard disc as image files (raw format) for later evaluation. As during the preoperative marking process, the examiner (N.H., M.W. and S.M.) assured that both eyes were level and that the patient’s head position was straight before capturing the images. The examiner was masked until the time that photograph was obtained. To ensure that the examiner was masked as long as possible, the retroillumination photograph was always performed at the very end of the follow-up examination.
Several follow-up measurements were obtained at the 3-month postoperative examination. These included autorefraction in IOL mode (Topcon RM 8800; Topcon Corporation, Tokyo, Japan), subjective refraction using the cross-cylinder method, IOLMaster 500 keratometry, unaided and corrected distance visual acuity using a backlit Early Treatment Diabetic Retinopathy chart at 4 m, wavefront measurements using a Hartmann-Shack sensor (WASCA; Zeiss Meditec AG, Jena, Germany), corneal tomography using Scheimpflug imaging (Pentacam HR; Oculus, Wetzlar, Germany), and a full slit-lamp examination. It should be noted that, because of organizational issues, 2 different Scheimpflug cameras were used for the preoperative and the postoperative assessments. Nonetheless, all preoperative images were captured using the first camera and all postoperative images were obtained with the second camera, ensuring minimal variation within the 2 groups of measurements.
Methods of Evaluation
Rotational stability analysis was performed as follows, using Keynote 5.0.2 software (Apple, Inc, Cupertino, California, USA). All retroillumination images were imported into the software system. Images in which the marking on the IOL was not visible were eliminated from the analysis, for example, in the case of small pupils or if one of the Purkinje reflexes was overlapping the toric marking on the IOL. To avoid observer bias, images were imported in random order to ensure that the 2 images from a single patient were not analyzed consecutively. Two thin (0.25 pixels) straight lines were adjusted to the marking on the IOL after magnifying the images. Each line touched the toric marking on the IOL on each side so that the 2 lines were parallel with the marking between the lines. The axes of both lines were entered into an Excel spread sheet (Microsoft, Redmond, Washington, USA), and the average of both lines was used for further statistical analysis. Astigmatism vector analysis was performed using Thibos’ power vector notation.
For statistical analysis, Microsoft Excel 2008 for Mac with a Statplus:mac version 5.8.3.8 plug-in (AnalystSoft, USA) was used, as well as SPSS software version 20.0 for Mac (IBM, USA). Descriptive data are shown as mean, standard deviation (SD), and range. For comparison of repeated measurements of the same eye at different points, the analysis of variance or analysis of covariance was used, unless otherwise noted. For regression analysis, univariate models were used and interactions between the variables were assessed using the type III sum of squares. Correlations are shown as Pearson correlation ( r 2 and P value).
Results
Thirty eyes of 30 patients (17 women and 13 men; 20 right eyes and 10 left eyes) were included in the study. The mean patient age was 67.0 years (range, 36 to 85 years). The cylinder power of the Tecnis Toric IOLs (=ZCT)—ZCT 100, ZCT 150, ZCT 225, and ZCT 300—were used in 5, 9, 10, and 6 cases, respectively. The mean preoperative axial eye length and anterior chamber depth (ACD) were 23.8 mm (SD, 1.9 mm; range, 20.4 to 27.7 mm) and 3.1 mm (SD, 0.4 mm; range, 2.3 to 3.8 mm), respectively.
Mean preoperative astigmatism, measured with autokeratometry, was 1.8 D (SD, 0.5 D; maximum, 2.8 D). No significant differences were observed between the values collected by IOLMaster keratometry and topography ( P < .05, paired heteroscedastic t test). Before surgery, Scheimpflug images showed different readings when compared with topography ( P = .03, paired heteroscedastic t test). The mean absolute difference for the steep and the flat meridian of the cornea was 0.18 mm (SD, 0.1 mm; maximum, 0.4 mm) and 0.26 mm (SD, 0.13 mm; maximum, 0.52 mm), respectively. In 4 of 60 retroillumination photographs, the orientation of the IOL could not be analyzed because of a small pupil with the iris covering the markings of the toric IOL.
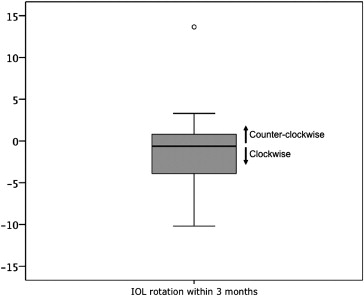
The mean absolute rotation of the IOL from 1 hour to 3 months after surgery was 2.2 degrees (SD, 3.1 degrees; maximum, 13.7 degrees; P = .04, 1-sample t test). A rotation of less than 3 and 6 degrees was observed in 59% and 91% of all patients, respectively. Concerning the direction of rotation, 18.2% were counter clockwise and 36.4% were clockwise, whereas 45.4% had no measurable rotation (± 1.5 degrees; Figure 1 ). The correlation between the magnitude of rotation of the toric IOL within the first 3 months after surgery and the axial eye length and the ACD was r 2 = 0.4 ( P = .06) and r 2 = 0.1 ( P = .58), respectively. The mean absolute misalignment compared with the intended placement 3 months after surgery was 3.6 degrees (SD, 3.2 degrees; maximum, 13.9 degrees; P = .04, 1-sample t test).
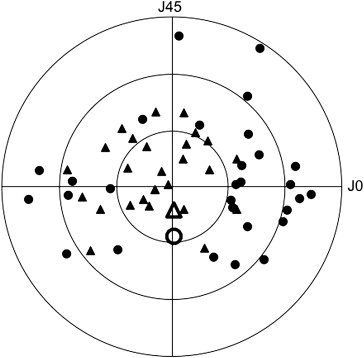
The mean postoperative astigmatism measured with subjective refraction and wavefront analysis was 0.9 D (SD, 0.5 D; range, 0.0 to 1.75 D) and 0.9 D (SD, 0.4 D; range, 0.2 to 1.9 D), respectively. As expected, the difference in astigmatism from before to after surgery was significant ( P < .001, Wilcoxon signed-rank test). Astigmatism was reduced by 44.9% (SD, 32.2%; range, −100% to +13.6%; see Figure 2 ). At the 3-month postoperative follow-up, astigmatism with the rule (75 to 105 degrees), astigmatism against the rule (165 to 15 degrees), and oblique astigmatism were observed in 17.4%, 39.1%, and 43.5%, respectively. In 62.5% of all cases, the astigmatism meridia of the anterior and posterior surfaces were within 15 degrees (mean absolute difference, 16.3 degrees; SD, 19.5 degrees; maximum, 76.7 degrees).
In 8 cases, residual astigmatism of more than 1.0 D was observed at the 3-month follow-up. Four of the 8 cases showed astigmatism of the posterior cornea of 0.6 D or more in the Scheimpflug measurement. In 3 cases, a rotation of more than 5 degrees was observed and in 1 case, and the refractive outcome could not be explained by observed parameters. The mean surgically induced astigmatism was 0.34 D (SD, 0.65 D; maximum, 0.97 D; P = .02, 1-sample t test), compared with the expected value of 0.30 D.
A prediction model for postoperative astigmatism was created with a linear model fitting best. Six different parameters were taken into account; nonetheless, residual astigmatism for the investigated sample was still poorly predictable ( r 2 = 0.05; P = .54). Parameters included in the prediction model included before surgery measured corneal astigmatism (B = 0.20; P = .76), cylinder power of the IOL (B = −0.15; P = .76), misalignment of the IOL (B = 0.01; P = .84), ACD measured before surgery (B = −0.08; P = .85), axial eye length (B = −0.05; P = .64), and surgically induced corneal astigmatism (B = −0.05; P = .84).
Further analysis using partial least squares regression revealed that 2 of the parameters did show significant predictive power for the amount of unexpected residual astigmatism (difference vector between the aimed and the measured astigmatism): the deviation in steep meridian between the anterior and the posterior surface of the cornea (variable importance for protection (VIP), 1.313; SD, 0.78), and orientation of the anterior surface of the cornea (VIP, 1.27; SD, 1.27). The amount of astigmatism on the posterior surface of the cornea (VIP, 0.72; SD, 1.12) or the anterior surface of the cornea (VIP, 0.38; SD, 1.17), however, did not have a significant influence on the amount of unexpected residual astigmatism.
Concerning visual acuity, the 3-month postoperative unaided and distance-corrected visual acuity measured with Early Treatment Diabetic Retinopathy charts was −0.05 logarithm of the minimal angle of resolution (logMAR; SD, 0.22 logMAR; range, 0.5 to −0.30 logMAR) and −0.17 logMAR (SD, 0.16 logMAR; range, 0.12 to −0.34 logMAR), respectively.
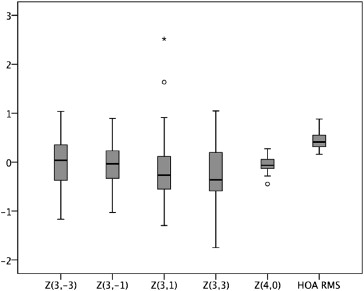
With regard to higher-order aberrations, a mean total root mean square and a higher-order aberration root mean square of 1.8 μm (SD, 1.2 μm; maximum, 5.3 μm) and 0.4 μm (SD, 0.2 μm; maximum, 0.9 μm) were found. The distribution of coma, trefoil, and spherical aberrations is shown in Figure 3 . Spherical aberration was −0.05 μm (SD, 0.17 μm; maximum, 0.28 μm) at 3 months after surgery.