Purpose
To understand the reasons for refusal of fellow eye surgical treatment for glaucoma after first eye trabeculectomy.
Design
Post hoc analysis of data collected in a multicenter, randomized clinical trial.
Methods
Data from participants in the Collaborative Initial Glaucoma Treatment Study (CIGTS) who were randomized to and underwent initial trabeculectomy on their study eye, and whose fellow eye was eligible for surgical treatment, were analyzed. Participant demographic data and characteristics, surgical data from the study eye, and quality-of-life survey results were compared between groups that received or refused trabeculectomy in their fellow eye. The main outcome measure was patient refusal of fellow eye surgery for glaucoma.
Results
Of 159 participants who were randomized to and underwent trabeculectomy on their study eye and had a fellow eye that was eligible for surgery, 30 (19%) refused fellow eye surgery. Eligible patients who refused fellow eye trabeculectomy did not differ significantly in visual function or local eye symptoms from those that underwent fellow eye trabeculectomy (all P > .05). In a multivariable analysis of data, increased fellow eye preoperative intraocular pressure (IOP) was associated with decreased odds (OR = 0.89, P = .0188), study eye hypotony at 3 months postoperatively was associated with increased odds (OR = 7.24, P = .0125), and argon suture lysis procedure was associated with decreased odds (OR = 0.38, P = .0385) of surgery refusal.
Conclusions
Refusal of fellow eye surgery was not uncommonly encountered in the CIGTS. Those who refused fellow eye surgery had lower fellow eye IOP and were more likely to have had hypotony after study eye trabeculectomy.
Glaucoma is a progressive, irreversible optic neuropathy that leads to visual field loss. Intraocular pressure (IOP) remains the only modifiable risk factor for glaucoma development and progression, and can be reduced by topical and oral medications, laser surgery, or incisional surgery.
In the Collaborative Initial Glaucoma Treatment Study (CIGTS), newly diagnosed and untreated patients with open-angle glaucoma were randomized to initial topical medical therapy or trabeculectomy. At the baseline examination a study eye was identified and had to meet eligibility criteria for treatment; the patient’s contralateral or fellow eye was included in the same treatment arm during the study and treated accordingly when eligible or at the discretion of the treating physician. In addition to ophthalmic examination and visual field studies, patients were asked to complete questionnaires regarding their visual activities, symptoms, and quality of life at regular intervals throughout the study. However, some patients refused treatment in the fellow eye. In this study, we examine the factors related to refusal of fellow eye trabeculectomy among CIGTS subjects, to provide insight into the potential reasons for refusal of surgical treatment for glaucoma. Our review of the literature failed to identify any prior studies of patients who refused fellow eye glaucoma surgery.
Methods
This study is a post hoc analysis of CIGTS participants initially randomized to medicine or surgery (trabeculectomy). Ongoing analysis of data collected in the CIGTS is under approval by the University of Michigan Institutional Review Board. The CIGTS is registered as a clinical trial at clinicaltrials.gov , #NCT00000149. Patients with primary open-angle glaucoma, pseudoexfoliative glaucoma, or pigmentary glaucoma with IOP of 20 mm Hg or higher who met visual acuity criteria, as well as visual field and/or optic nerve criteria, were included in the study. Patients were between 25 and 75 years old.
Exclusion criteria included use of eye drops for glaucoma >14 days; ocular disease that may affect IOP or visual function/field; nonproliferative or proliferative diabetic retinopathy or diabetic macular edema; previous ocular laser or intraocular surgery or likely cataract surgery in the next year; and use of corticosteroids.
If at initial assessment both eyes were eligible for treatment, prior to randomization the treating ophthalmologist designated 1 eye to receive initial treatment. This eye was designated the “study eye” and the contralateral eye was designated the “fellow eye.” If the study eye underwent trabeculectomy and the fellow eye was eligible at the time of randomization, then the study protocol specified that surgery of the fellow eye should occur at least 4 weeks after surgery on the study eye and before 6 months after randomization. Fellow eyes could also become eligible for treatment after randomization. Further details on enrollment, randomization, treatment sequences, and examination protocols are published elsewhere.
Descriptive statistics of the sample were summarized with means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Information on participants (both person- and eye-based) who received fellow eye trabeculectomy when eligible was compared to those that refused surgery, in the following categories: clinical measures (mean deviation [MD], IOP), demographics of the participant (age, race, sex), operative characteristics and postoperative complications of the study eye’s surgery, and quality-of-life measures (Visual Activities Questionnaire (VAQ), Center for Epidemiological Studies Depression Scale (CES-D 8), Symptom and Health Problem Chart). The quality-of-life measures used in CIGTS were described elsewhere. Comparisons were made using the t test for continuous variables or χ 2 and Fisher exact tests for categorical variables. The Holm method was used to adjust for multiple comparisons. A multivariable regression model was used to determine preoperative, surgical, and postoperative variables that were independent predictors of fellow eye surgery refusal. Given the low sample size of 30 patients that refused fellow eye surgery, multivariable models were limited to 3 variables. Model selection was performed using the method of best subsets with the score statistic as the selection criteria. All variables that were significant at P < .30 in univariate analyses were included for investigation. SAS version 9.4 was used for all statistical analyses (SAS, Cary, North Carolina, USA).
Results
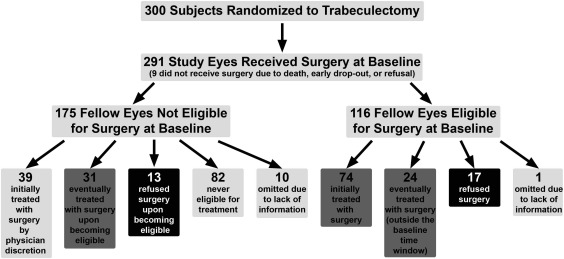
A total of 607 patients were enrolled in CIGTS with 300 randomized to initial surgery and 307 randomized to initial medication to treat their glaucoma. Nine participants who were randomized to trabeculectomy did not receive surgery in the study eye owing to death (n = 1), early dropout (n = 2), and refusal (n = 6). In patients who were randomized to and received trabeculectomy in their study eye (N = 291), 116 fellow eyes (39.7%) were eligible for treatment at baseline. An additional 44 fellow eyes became eligible in follow-up.
One of the 116 participants with a fellow eye eligible for trabeculectomy at baseline was missing follow-up information and was excluded. As displayed in the Figure , 85.2% (98/115) of those with initially eligible eyes underwent trabeculectomy and 14.8% participants (17/115) refused surgery. By comparison, 0.8% (1/122) of participants within the group randomized to receive medicine refused treatment for the baseline eligible fellow eyes ( P < .0001, Fisher exact test). Of the 165 surgery arm participants with a treatment-ineligible fellow eye at baseline and follow-up information, 44 (26.7%) became eligible for treatment during follow-up, of which 13 (29.5%) refused surgery; the rate of surgery refusal was higher among those participants eligible during follow-up compared with that of initially eligible participants ( P = .0333, χ 2 ). In total, of 159 participants whose fellow eye either was initially or subsequently became eligible for surgery and for whom follow-up information was available, 30 (18.9%) refused surgery ( Figure ).
A comparison of participants with fellow eyes eligible for treatment either at baseline or during follow-up that refused (n = 30) vs accepted surgery (n = 129) did not show differences in sex, race, or age ( Table 1 ). Mean deviation at baseline visual field was similar in fellow eyes of participants that were treated or refused surgical treatment. For the 129 fellow eyes that received trabeculectomy, the date of surgery ranged from 18 days to 8.5 years after randomization.
| Continuous Variables | FE Trabeculectomy Refusals (n = 30) | FE Treated With Trabeculectomy (n = 129) | P Value a |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (y) | 59.2 ± 9.9 | 59.1 ± 10.9 | .9488 |
| SE baseline MD (dB) | −6.3 ± 4.9 | −6.4 ± 4.2 | .8958 |
| FE baseline MD (dB) | −3.1 ± 3.2 | −3.7 ± 3.1 | .3760 |
| FE MD prior to treatment/refusal (dB) | −4.2 ± 4.5 | −3.9 ± 3.8 | .7018 |
| SE baseline IOP (mm Hg) | 25.7 ± 4.2 | 28.4 ± 6.0 | .0058 |
| FE baseline IOP (mm Hg) | 23.6 ± 3.3 | 26.2 ± 5.2 | .0010 |
| FE IOP prior to treatment/refusal (mm Hg) | 24.3 ± 4.7 | 27.6 ± 5.6 | .0029 |
| Categorical Variables | Frequency (%) | Frequency (%) | P Value b |
| Sex | |||
| Male | 14 (46.7) | 76 (58.9) | .2228 |
| Female | 16 (53.3) | 53 (41.1) | |
| Race | |||
| White | 19 (63.3) | 64 (49.6) | .2988 |
| Black | 10 (33.3) | 57 (44.2) | |
| Asian | 1 (3.33) | 2 (1.6) | |
| Other | 0 (0.0) | 6 (4.7) |
In participants that underwent trabeculectomy in their fellow eye compared to those who refused surgery, the fellow eye IOP was significantly higher both at baseline (26.2 ± 5.2 mm Hg vs 23.6 ± 3.3 mm Hg, P = .0010) and at the visit prior to treatment or refusal (baseline for fellow eyes initially eligible, or a follow-up visit in those becoming eligible; 27.6 ± 5.6 mm Hg vs 24.3 ± 4.7 mm Hg, P = .0029).
The study eye IOP was similar between patients that refused and accepted fellow eye surgery at the 1 day and 1 week visits after surgery. However, study eye IOP was significantly lower at 1 month in fellow eye trabeculectomy refusers ( P = .0027). Hypotony (IOP <6 mm Hg) in the study eye occurred more frequently in fellow eye surgery refusers at the 1 month and 3 month postoperative visits ( P = .0215 and P = .0059, respectively; Table 2 ). In the fellow eye refuser group, 2 of the 3 subjects who had study eye hypotony at 1 month also had study eye hypotony at 3 months. Among those who accepted fellow eye surgery, the 1 subject whose study eye had hypotony at 1 month did not have hypotony in the study eye at 3 months. By 6 months after surgery, the average study eye IOP and percentages of study eyes with hypotony were similar between the groups.
| Postoperative SE IOP | FE Trabeculectomy Refusals (n = 30) | FE Treated With Trabeculectomy (n = 129) | P Value a |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| 1 day | 14.9 ± 9.6 | 14.6 ± 10.8 | .9142 |
| 1 week | 11.7 ± 7.0 | 11.9 ± 8.1 | .9241 |
| 1 month | 11.6 ± 5.2 | 15.5 ± 6.6 | .0027 |
| 3 months | 12.3 ± 5.8 | 14.6 ± 6. | .0785 |
| 6 months | 13.6 ± 4.8 | 14.1 ± 4.6 | .6370 |
| SE Hypotony (IOP <6 mm Hg) | Frequency (%) | Frequency (%) | P Value b |
| 1 day | 7 (23.3) | 28 (21.7) | .8463 |
| 1 week | 6 (20.0) | 24 (18.9) | .8901 |
| 1 month | 3 (10.0) | 1 (0.8) | .0215 |
| 3 months | 5 (17.9) | 3 (2.4) | .059 |
| 6 months | 1 (3.3) | 4 (3.2) | 1.0000 |
Surgical variables from the study eye surgery (operating room setting, surgeon [community ophthalmologist vs clinical center ophthalmologist], anesthesia type, surgical [scleral flap] site, conjunctival flap site) were similar between participants that refused and received fellow eye trabeculectomy ( Table 3 ). There were no intraoperative choroidal detachments (serous, hemorrhagic, expulsive hemorrhage) in either group ( Supplemental Table , available at AJO.com ). Intraoperative hyphema occurred at similar frequencies in both groups. Postoperative cornea problems occurred more frequently in the study eye of patients that refused fellow eye surgery ( P = .0421, Holm adjusted P = .7999) and laser suture lysis was performed less often in the study eye of patients that refused fellow eye surgery ( P = .0105, Holm adjusted P = .2100).
| FE Trabeculectomy Refusals (n = 30) | FE Treated With Trabeculectomy (n = 129) | P Value a , c | |
|---|---|---|---|
| Frequency, n (%) | Frequency, n (%) | ||
| Intraoperative Variables | |||
| Combined with cataract extraction | 1 (3.3) | 1 (0.8) | .3447 |
| Anesthesia | |||
| Local | 2 (6.7) | 18 (14.0) | .2324 |
| Local/standby | 27 (90.0) | 110 (85.3) | |
| General | 1 (3.3) | 1 (0.8) | |
| Surgical site | |||
| Superior-nasal | 12 (40.0) | 64 (49.6) | .5312 |
| Superior-temporal | 2 (6.7) | 11 (8.5) | |
| Superior | 16 (53.3) | 54 (41.9) | |
| Conjunctiva incision | |||
| Limbus-based | 28 (93.3) | 113 (87.6) | .5291 |
| Fornix-based | 2 (6.7) | 16 (12.4) | |
| Anterior chamber hyphema | |||
| No | 26 (86.7) | 117 (90.7) | .5842 |
| Mild | 4 (13.3) | 11 (8.5) | |
| Moderate | 0 (0) | 1 (0.8) | |
| Postoperative Variables | |||
| Marked inflammation | 2 (6.7) | 1 (0.8) | .0915 |
| Choroidal hemorrhage | 0 (0) | 2 (1.6) | 1.0000 |
| Anterior chamber hyphema | 3 (10.0) | 15 (11.6) | 1.0000 |
| Shallow/flat anterior chamber | 6 (20.0) | 16 (12.4) | .3762 |
| Serous choroidal detachment | 4 (13.3) | 10 (7.8) | .3037 |
| Wound leak | 1 (3.3) | 7 (5.4) | 1.0000 |
| Wound infection | 0 (0) | 0 (0) | 1.0000 |
| Corneal problems | 4 (13.3) | 4 (3.1) | .0421 |
| Ptosis | 4 (13.3) | 17 (13.2) | 1.0000 |
| Progression of/new lens opacities | 2 (6.7) | 2 (1.6) | .1616 |
| Encapsulated bleb | 2 (6.7) | 14 (10.9) | .7384 |
| Endophthalmitis | 0 (0) | 0 (0) | 1.0000 |
| Anterior chamber re-formation | 2 (6.7) | 1 (0.8) | .0926 |
| Argon laser suture lysis | 9 (30.0) | 70 (56.0) | .0105 |
| Mean ± SD | Mean ± SD | P Value b | |
| # Complications (up to 14) | 1.0 ± 1.5 | 0.7 ± 1.0 | .2855 |
a χ 2 test or Fisher exact test (when cell counts <5).
c Upon adjustment for multiple comparisons using the Holm method, no variables were significantly associated with fellow eye surgery refusal (all P > .05; argon suture lysis P = .2100, corneal problems P = .7999).
A multivariable logistic regression model identified 3 independent predictors associated with the probability of fellow eye surgery refusal. Higher fellow eye IOP at the visit prior to treatment/refusal was associated with decreased odds of refusing fellow eye surgery (odds ratio [OR] = 0.89, 95% confidence interval [0.81–0.98]; P = .0188). Study eye hypotony at 3 months post trabeculectomy was associated with increased odds of refusal (OR = 7.24, 95% confidence interval [1.53–34.23]; P = .0125). Lastly, argon laser suture lysis was associated with decreased odds of refusal (OR = 0.38, 95% confidence interval [0.15–0.95]; P = .0385).
The most common study eye surgical complication in follow-up was a shallow or flat anterior chamber (20% of fellow eyes refusing surgery vs 12.4% of fellow eyes treated with surgery, P = .3762). Ptosis in the study eye following surgery was also seen frequently, occurring in 13.3% and 13.2% of participants that refused and received fellow eye surgery, respectively ( P = 1.000). Overall, the number of postoperative complications did not differ between the 2 groups ( P = .2855).
VAQ total score and CES-D 8 score at study baseline, at 3 months, and prior to fellow eye treatment or refusal were similar between the 2 groups ( Table 4 ).



