Purpose
To evaluate differences in mean deviation values in automated perimetry in healthy eyes with multifocal compared to monofocal intraocular lens (IOL) implants.
Design
Prospective, age-matched, comparative analysis.
Methods
setting : Single-center, tertiary referral academic practice. patient population : A total of 37 healthy eyes in 37 patients with bilateral multifocal (n = 22) or monofocal (n = 15) IOL implants were studied. intervention/observation procedure : Humphrey Visual Field 10-2 testing was performed on all patients. main outcome measures : Mean deviation (MD) and pattern standard deviation (PSD) numerical values were evaluated and compared between groups.
Results
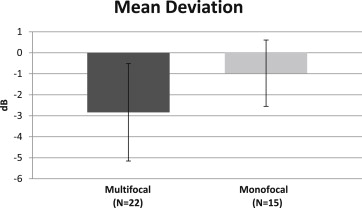
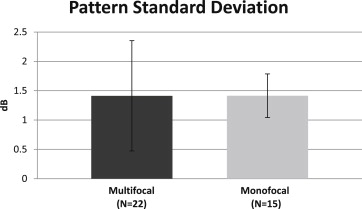
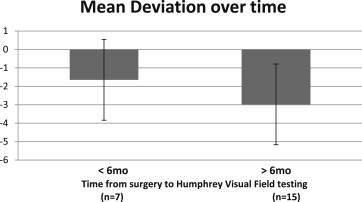
The average MD was −2.84 dB (SD 2.32) for the multifocal IOL group and −0.97 dB (SD 1.58) for the monofocal IOL group ( P = .006). There was no significant difference in PSD between the 2 groups ( P = .99). Eyes that had the visual field 10-2 testing ≥6 months from time of IOL placement showed no improvement in MD when compared to eyes that were tested within 6 months from IOL placement.
Conclusion
Multifocal IOL implants cause significant nonspecific reduction in MD values on Humphrey Visual Field 10-2 testing that does not improve with time or neuroadaptation. Multifocal IOL implants may be inadvisable in patients where central visual field reduction may not be tolerated, such as macular degeneration, retinal pigment epithelium changes, and glaucoma.
Nonpathologic visual field defects from optical anomalies are frequently encountered during automated perimetry in the office setting. Clinical reasons for these relative visual field changes include media opacities, uncorrected refractive errors, lens rim artifacts, miosis, and lid or brow ptosis. With alterations in incident light and contrast on the retina, changes in automated perimetry numerical values of mean deviation (MD) and pattern standard deviation (PSD) can be studied.
Multifocal intraocular lenses (IOLs) produce simultaneous retinal images with different focal planes in order to reduce spectacle dependency for distance and near visual acuities. Along with potential benefits, however, is the reality that the amount of light energy in focus at any given focal distance is reduced, out-of-focus light is superimposed, and approximately 18% of transmitted light in diffractive IOLs, which may vary depending on IOL design, is lost to higher orders of diffraction that are not ever focused on the retina. As a result, patients with multifocal IOLs may experience glare and halos, as well as reduced contrast sensitivity. Mesopic conditions tend to exacerbate these deficiencies. Furthermore, increased chromatic aberrations and light scattering have also been reported. In light of these optical disturbances, we evaluated the effect of diffractive multifocal IOLs on a common clinical test, Humphrey Visual Field Analyzer (Zeiss-Meditec, Dublin, California, USA) 10-2, to determine the impact on performance in patients with bilateral multifocal or monofocal IOL implants.
Several studies have previously reported the effects of intraocular lenses on visual field testing. Mutlu and associates demonstrated that monofocal IOLs may reduce MD in Humphrey Visual Field 24-2 testing compared to healthy phakic patients. Specifically, the effects of multifocal IOLs on perimetry have been evaluated with Octopus 101 autoperimetry, Goldmann manual perimetry, frequency doubling technology matrix perimetry, automated Esterman binocular field test, and Humphrey Visual Field 30-2. With appreciation of the previous contributions, this study is the first to use Humphrey Visual Field 10-2 to compare and quantify the effects of multifocal and monofocal IOL on the central 10 degrees of vision.
Materials and Methods
Institutional Review Board/Ethics Committee approval was obtained from the University of California, Irvine, prior to a prospective comparative analysis. All patients reviewed and signed a detailed informed consent form prior to participating in the study. A total of 37 healthy eyes in 37 patients were enrolled, all with either bilateral multifocal IOLs (n = 22) or monofocal IOLs (n = 15). Cataract surgeries had been previously performed by 1 of 3 surgeons (M.F., R.F.S., S.G.). One eye was selected at random from each patient for the study to ensure independence of the variables. Inclusion criteria were each eye having corrected distance visual acuity (CDVA) ≥20/25 with no other ocular pathology, including retinal disease, glaucoma or optic neuropathy, ocular hypertension, amblyopia, irregular corneal astigmatism, corneal dystrophy, or significant capsular opacity. Dilated examinations of the macula and optic nerve were performed on all eyes to ensure no evidence of pathology prior to testing. All eyes had normal intraocular pressures on multiple visits. Patients with mild dry eye symptoms and signs were not excluded from the study. All cataract surgeries were uncomplicated, with clear corneas and good centration of the IOL in the capsular bag. All multifocal IOLs had aspheric diffractive optics (no refractive multifocal IOLs were included). Any patients with psychological or neurologic disorders, poor concentration, or poor cooperation were excluded from the study. Patients were also excluded if they had a history of prior refractive corneal surgery. Patients with scotopic pupil diameters smaller than 2.5 mm were excluded to avoid diffraction-limited visual field artifacts. All manifest refractions were within 1 diopter of goal in the monofocal IOL group and within 0.5 diopter spherical equivalent in the multifocal IOL group. All eyes had less than 0.5 diopters of refractive astigmatism. No patients with monovision were included. All refractive errors were lens corrected during Humphrey Visual Field 10-2 testing.
All Humphrey Visual Field 10-2 automated perimetry testing was measured with the Swedish Interactive Threshold Algorithm (SITA) standard threshold test algorithm, white stimulus, size III target, and standard Humphrey background luminance of 31.5 apostilb. The earliest visual field testing was measured at postoperative month 1. Near vision refractions were done on every eye prior to testing to ensure that the patient had the minimum refractive add power necessary for comfortable 20/20 vision at the testing distance. Most multifocal IOL eyes required little or no add at this distance. Nevertheless, careful refractive measurements were performed at the testing distance and if an add power was required, it was given by corrective lenses. MD and PSD, as well as reliability indices including fixation losses and false-positive and false-negative numeric values, were recorded. Poor tests with high fixation losses or false-positive/negative values were repeated for reliability. Statistical analysis was performed comparing the multifocal group to the monofocal group using a 2-tailed Student t test under the assumption that the 2 groups had unequal variance ( www.studentsttest.com ).
Results
Thirty-seven patients were included in the study. One eye from each patient was selected randomly for analysis: 22 eyes with multifocal IOLs and 15 eyes with monofocal IOLs. The multifocal IOLs included the 1-piece Tecnis ZMB00 (n = 11) and the 3-piece Tecnis ZMA00 (n = 6) (Abbott Medical Optics, Santa Ana, California, USA), as well as the Acrysof IQ ReSTOR SN6AD1 (n = 5) (Alcon, Fort Worth, Texas, USA). The monofocal IOLs included the 1-piece Tecnis ZCB00 (n = 7) and the 3-piece Tecnis ZA9003 (n = 6) (Abbott Medical Optics) as well as the Acrysof IQ SN60WF (n = 2) (Alcon). There was no significant difference in age or sex between the groups. The average age was 73 years in both groups, with 14 female patients in the multifocal group (14/22; 63.6%) and 10 in the monofocal group (10/15; 66.7%).
The average mean deviation was −2.84 dB (SD 2.32) for the multifocal IOL group and −0.97 dB (SD 1.58) for the monofocal IOL group ( P = .006) ( Figure 1 ). The average pattern standard deviation was 1.41 dB (SD 0.94) and 1.41 dB (SD 0.37) for the multifocal and monofocal groups, respectively ( P = .99) ( Figure 2 ).
Time from cataract surgery to Humphrey Visual Field 10-2 testing was also evaluated to assess if neuroadaptation over time may correlate with less reduction in MD. The time between surgery and visual field testing averaged 12.5 months in the multifocal IOL group (range, 1–34 months) and 4.9 months in the monofocal IOL group (range, 1–26 months). Six months was chosen as a dividing line to assess neuroadaptation based on previous reports. The MD values in multifocal IOL patients with time to visual field testing less than 6 months (n = 7) compared to those with time to visual field testing greater than 6 months (n = 15) were −1.65 dB and −2.98 dB, respectively, with no significant difference between the two ( P = .15) ( Figure 3 ).
Results
Thirty-seven patients were included in the study. One eye from each patient was selected randomly for analysis: 22 eyes with multifocal IOLs and 15 eyes with monofocal IOLs. The multifocal IOLs included the 1-piece Tecnis ZMB00 (n = 11) and the 3-piece Tecnis ZMA00 (n = 6) (Abbott Medical Optics, Santa Ana, California, USA), as well as the Acrysof IQ ReSTOR SN6AD1 (n = 5) (Alcon, Fort Worth, Texas, USA). The monofocal IOLs included the 1-piece Tecnis ZCB00 (n = 7) and the 3-piece Tecnis ZA9003 (n = 6) (Abbott Medical Optics) as well as the Acrysof IQ SN60WF (n = 2) (Alcon). There was no significant difference in age or sex between the groups. The average age was 73 years in both groups, with 14 female patients in the multifocal group (14/22; 63.6%) and 10 in the monofocal group (10/15; 66.7%).
The average mean deviation was −2.84 dB (SD 2.32) for the multifocal IOL group and −0.97 dB (SD 1.58) for the monofocal IOL group ( P = .006) ( Figure 1 ). The average pattern standard deviation was 1.41 dB (SD 0.94) and 1.41 dB (SD 0.37) for the multifocal and monofocal groups, respectively ( P = .99) ( Figure 2 ).




