Procedures
Introduction
Advances in technology over the past several years have enabled those interested in the aerodigestive tract to perform a wide array of procedures in the outpatient environment without sedation. Although techniques involving topical anesthesia have not changed appreciably, the extraordinary optical systems currently available with distal-chip transnasal esophagoscopes allow us to perform a variety of innovative procedures.
The success of office-based procedures is entirely dependent on the adequacy of the topical anesthesia and patient selection. Ideally, the patient selected for transnasal esophagoscopy (TNE) or any related procedures should not be overly anxious and should be confident that he or she can tolerate such a procedure. Virtually all our procedures are done through the nostrils, and therefore appropriate nasal patency is necessary. Anticoagulation is not a contraindication to TNE nor taking biopsies, but anticoagulated patients are observed for 15 minutes following the procedure to ensure that there is no bleeding.
Each procedure presented is performed with standard TNE anesthesia, as discussed earlier. In addition, 2 to 6 cc of lidocaine 2% to 4% is frequently administered through the working channel of the esophagoscope to the area of interest (pharynx, larynx, or trachea). This is usually all that is necessary for any procedure. No topical esophageal anesthesia is required for biopsies taken in the esophagus. Procedures in the trachea usually require additional topical anesthesia.
Other techniques for delivering topical anesthesia include dripping the anesthetic into the larynx and hypopharynx through a curved Abraham cannula passed transorally and the use of nebulized lidocaine. No matter which technique or anesthetic agent selected by the endoscopist, one must always keep in mind the recommended maximal dosages to avoid any adverse reactions to the local anesthetics. Lidocaine 4% has a maximal dose of 7 to 8 cc for a 70-kg patient (1).
Biopsies
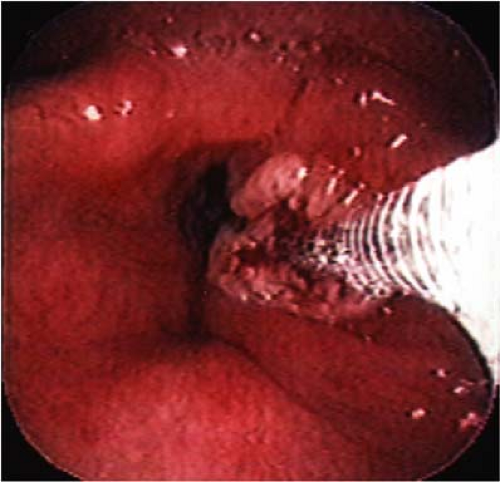
The 2.0-mm working channel allows the passage of a 1.8-mm biopsy cup forceps. With adequate topical anesthesia, nearly any location in the upper aerodigestive tract can be biopsied without difficulty and without patient discomfort. We have biopsied lesions in the nasal cavity, nasopharynx, hypopharynx, larynx, subglottis, and trachea (Figs. 10.1 and 10.2). In addition, we routinely take biopsies throughout the esophagus and gastric cardia. We have obtained hundreds of biopsies without a single complication, and this includes biopsies taken from a number of individuals undergoing systemic anticoagulation with warfarin or clopidogrel bisulfate.
The use of the transnasal esophagoscope as a “panendoscope” for head and neck cancer patients provides the head and neck oncologic surgeon with a significant addition to his or her practice (2). This endoscope allows the biopsy of lesions, close detailed follow-up of head and neck cancer patients, as well as the avoidance of formal panendoscopy under general anesthesia in selected patients. An increasing number of our patients have undergone transnasal panendoscopy with biopsy, followed by definitive treatment without endoscopy and biopsy under general anesthesia (Fig. 10.3). Since TNE is so well tolerated without systemic medications, it is of great value in older individuals and in patients with significant medical comorbidities in whom sedation could be problematic.
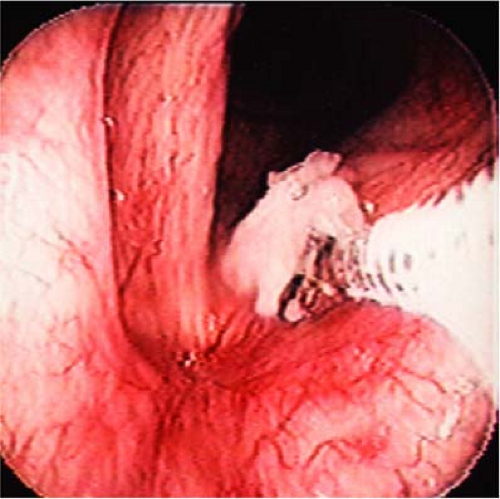 Figure 10.1 Biopsy of a left vocal-fold lesion using 1.8-mm cup forceps. The lesion was determined to be histoplasmosis. |
Posttherapy Dysphagia
TNE can also assist in the evaluation of patients with dysphagia following cancer therapy and reconstruction. We occasionally feed patients with applesauce or water dyed with food coloring, or acetaminophen capsules while the esophagoscope is in place to evaluate the anastomotic sites of regional and free-flap reconstructions (Fig. 10.4) (3). This allows us to determine the precise location and cause of the individual’s dysphagia.
Tracheoesophageal Puncture
Patients who have undergone total laryngectomy have many options for voice rehabilitation. In our practice, the most popular has been the placement of a voice prosthesis in a surgically created tracheoesophageal fistula. This can be performed in the office without sedation in properly selected patients (4). Such secondary tracheoesophageal punctures (TEP) can only be done in individuals with a reasonably sized tracheostoma. This procedure, when performed in the office, provides a significant cost saving. During the entire procedure, the transnasal esophagoscope provides the surgeon and assistant with clear visualization of the surgical site in the neopharynx by gentle insufflation of air. This allows the procedure to be done safely with a minimum of discomfort to the patient. In addition, the insufflation of air in the neopharynx in patients whose voice prosthesis has been lost allows reestablishment of the tracheoesophageal fistula and prosthesis reinsertion when it has partially closed (5).
In addition to the transnasal esophagoscope, a TEP dilator, as well as local anesthetic usually consisting of lidocaine 2% with epinephrine, and a No. 15 scalpel are employed. Patients
undergoing this procedure should have neither neopharyngeal strictures nor a small stoma. Local anesthetic with epinephrine is infiltrated into the posterior tracheal wall at the area of the planned TEP site. After appropriate vasoconstriction has occurred, 2 cc of lidocaine 2% are sprayed into the tracheal stoma, the patient swallows 5 mL of a viscus lidocaine 2% solution, and the transnasal esophagoscope is then passed into the neopharynx. Both endoscopist and surgeon are now able to visualize the neopharynx. An 18- to 20-gauge needle is passed in the midline through the posterior tracheal wall, and the anterior wall of the esophagus is seen on the monitor (Fig. 10.5). The proper position is verified before penetration of the esophageal mucosa. Air insufflation protects the posterior esophageal wall. The needle is then withdrawn, and an incision is created in the same site using the scalpel blade (Fig. 10.6). A hemostat may be used to open this further if desired. The TEP dilators can then be passed under direct vision through the puncture site in the esophagus. We normally enlist the aid of one of our speech-language pathologists who uses the TEP sizing device, and then the appropriate size prosthesis is inserted. This is performed using the Gel-Cap technique. The Gel-Cap holds the inner flanges of the prosthesis together to allow it to be easily inserted. When it dissolves, the flange opens in the pharyngeal lumen. Positioning is verified using the endoscope. Alternatively, the placement of a red rubber catheter through the TEP is slightly easier than the immediate placement of a prosthesis (Fig. 10.7A,B



undergoing this procedure should have neither neopharyngeal strictures nor a small stoma. Local anesthetic with epinephrine is infiltrated into the posterior tracheal wall at the area of the planned TEP site. After appropriate vasoconstriction has occurred, 2 cc of lidocaine 2% are sprayed into the tracheal stoma, the patient swallows 5 mL of a viscus lidocaine 2% solution, and the transnasal esophagoscope is then passed into the neopharynx. Both endoscopist and surgeon are now able to visualize the neopharynx. An 18- to 20-gauge needle is passed in the midline through the posterior tracheal wall, and the anterior wall of the esophagus is seen on the monitor (Fig. 10.5). The proper position is verified before penetration of the esophageal mucosa. Air insufflation protects the posterior esophageal wall. The needle is then withdrawn, and an incision is created in the same site using the scalpel blade (Fig. 10.6). A hemostat may be used to open this further if desired. The TEP dilators can then be passed under direct vision through the puncture site in the esophagus. We normally enlist the aid of one of our speech-language pathologists who uses the TEP sizing device, and then the appropriate size prosthesis is inserted. This is performed using the Gel-Cap technique. The Gel-Cap holds the inner flanges of the prosthesis together to allow it to be easily inserted. When it dissolves, the flange opens in the pharyngeal lumen. Positioning is verified using the endoscope. Alternatively, the placement of a red rubber catheter through the TEP is slightly easier than the immediate placement of a prosthesis (Fig. 10.7A,B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree