Primary Epithelial Neoplasms
This chapter includes a host of epithelial neoplasms of various histologic types, which, with rare exceptions, arise from the functional components of the lacrimal gland. One exception in the Mayo Clinic series of orbital tumors is noted later. The factor common to these intrinsic lesions is a variable degree of proliferation of cellular derivatives of the secretory or ductal epithelium. Nonepithelial tumors that may be primary in the lacrimal gland including non-Hodgkin lymphomas, cavernous hemangioma, hemangiopericytoma, inflammatory tumor with or without vasculitis, Wegener granulomatosis, sarcoid, and sarcoidosis will be mentioned only as one or they may all go into the differential diagnosis from the epithelial group of tumors. The number and histologic type of the primary and secondary epithelial neoplasms in the Mayo Clinic series are listed in Table 15.1.
Before discussing the individual tumor subtypes, consideration should be given to those clinical and radiologic correlates that are either common to the group as a whole or provide preoperative characterization of a particular tumor subtype. A feature common to all the lacrimal gland neoplasms is a firm enlargement of the lacrimal gland that indents the surface of the contiguous eye resulting in a downward and inward displacement of the eye associated with some degree of proptosis. The larger the tumor, which is a factor of its duration, the greater the malpositioning of the eye. This malposition may reach an extreme degree in many cases of long duration, but may also be seen with slowly expanding orbitofrontal hematocele of bone (Fig. 1.1 and Fig. 4.18). None of the nonepithelial lesions of the lacrimal gland listed earlier produce the degree of downward displacement of the eye that is seen with the intrinsic neoplasms. The mass effect of the tumor also causes some mechanical limitation of ocular movement in the direction of the lesion.
If the neoplasm expands anteriorly, medially, or inferiorly, the mass is always palpable. If the tumor expands into the roof of the orbit or posteriorly toward the orbital apex, its palpation may be minimal in degree or absent. However, this dictum is not specific to the intrinsic neoplasms and may also apply to other neoplasms and non-neoplastic lesions in the same location.
All the lacrimal gland tumors may be associated with some degree of pain, discomfort, pressure sensation, or be entirely pain free throughout their progressive course. Although the malignant tumors are more often associated with pain in their clinical course when compared to the benign tumors, this is not a reliable basis for a preoperative differentiation between the benignity or the malignancy of the lesion. The presence of pain, especially when the eyelids are erythematous and swollen, may even be a manifestation of an inflammatory, vasculitic, or granulomatous lesion in the same location.
The literature uniformly implies that the duration of symptoms at the time of presentation plays a key role in predicting a malignant or benign neoplasm. A shorter period of symptoms (<1 year) is said to be representative of a malignant lesion, and a longer period is characteristic of a benign mass. This rule does not take into consideration the highly variable factor of how observant patients are of their ocular disability and how they react to it. One type of patient may present after a 1-month interval of “pressure sensation” over the eye and prove to have a benign mixed tumor. Another patient may be aware of the displacement of one eye but tolerate the problem for some years before presenting with a mass that proves to be malignant. Extreme examples of malignant tumors (adenoid cystic carcinomas) associated with long intervals of symptomatology include reports of 25 years (case 3 of Portis et al., 1985), 30 years (Waller et al., 1973), and 60 years (Shields et al., 1987), 20 years (Byers et al., 1975), 18 years (Wright, 1982), and 18 years (Jakobiec, 1987). These case reports, which are contrary to the general rule, are largely overlooked in discussions of the subject. In our experience, the duration of
symptoms is too variable and subjective to serve as a dependable guide to diagnosis.
symptoms is too variable and subjective to serve as a dependable guide to diagnosis.
Table 15.1 Number and Histologic Type of Primary and Secondary Epithelial Neoplasms of the Lacrimal Gland: Mayo Clinic Series 1948–1997 a | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
The specificity of radiologic features in the preoperative differential diagnosis of malignant versus benign lesions is also overstated (Lemke et al., 1996) and (Mafee et al., 1999). Changes in the bone contiguous to the tumor may occur in both types. Likewise, calcific-like densities in the soft tissue are nonspecific. Although the tumor conforms to all the credos of the preliminary diagnosis, and none of the above exceptions exist, there is a 50:50 chance that a working diagnosis will be wrong when the true identity of the tumor is established. In the realm of changes in the bone contiguous to the tumor, the lytic destruction (as opposed to compression erosion) of bone is the only positive feature that may differentiate a malignant from a benign process. Eleven of 16 nonrecurrent adenoid cystic carcinomas in our Mayo series were initially radiographically negative for changes in bone. Only 3 of 16 cases showed a malignant type of bone destruction. An atypical feature was noted by Rootman and Dolman (1988) in two children aged 11 and 14. The authors believed the invasive features of adenoid cystic carcinoma were not evident in the computed tomography (CT) scans of these patients because of the tendency of the more pliable bone in this age-group to undergo expansion rather than invasion. Nevertheless, the absence of the invasive features of bone in these two cases is compatible with our finding (vide supra) that 68% (11 out of 16) of nonrecurrent adenoid cystic carcinomas were radiographically negative for changes in bone. Also Wharton and O’Donnell (1999) report an atypical case in a 65-year-old woman with a long history of right hypoglobus with sudden exacerbation of symptoms. CT scan showed a round, well-defined lesion in the fossa of the lacrimal gland with a hypotense extension suggestive of malignancy. The lesion was excised revealing a hemorrhage within a pleomorphic adenoma.
Table 15.2 Incidence of Primary Epithelial Neoplasms of Lacrimal Gland: Series of Over 50 Cases | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||
With these preliminary inconsistencies in mind, the surgical and histologic identification of the lacrimal gland mass remain the only means for correct diagnosis. The anterolateral surgical route (Mourier et al., 1994) is useful for this identification process.
Ordinarily, when the surgeon is confronted with an unknown type of tumor, incisional biopsy and frozen tissue study will determine whether the lesion should be removed or allowed to remain in the orbit. However, such an approach to an unknown type of tumor in the lacrimal gland fossa would be a hazard to the patient should the mass prove to be a benign mixed tumor. This lesion is notorious for seeding into the operation site when handled in such a manner. The consequence is a high rate of multiple recurrence throughout the lifetime of the patient with a chance of malignant transformation of the recurrent tumor at some later date. Surgeons who are acquainted with the color and configuration of the benign mixed tumor, therefore, will strive for an “intact,” “complete,” or “total” removal of such a tumor without a preliminary biopsy. For surgeons not well acquainted with the gross appearance of tumors in this area, it would be advisable to completely remove all encapsulated or well-circumscribed masses without incisional biopsy, although the mass proves not to be a benign mixed tumor. An alternative is the “protective” incisional biopsy. Here the lesion is dissected from its bed except for a remaining
pedicle of lacrimal gland, rotated laterally out of the orbital space, stabilized by a narrow gauze-strip wrap around the pedicle, and incised outside the orbital space. Subsequently, the pedicle can be severed and the tumor removed, or the biopsy incision closed and the mass returned to the orbital space depending on the outcome of the frozen tissue examination. Infiltrative and malignant tumors can be safely diagnosed, without fear of seeding, by this method of biopsy.
pedicle of lacrimal gland, rotated laterally out of the orbital space, stabilized by a narrow gauze-strip wrap around the pedicle, and incised outside the orbital space. Subsequently, the pedicle can be severed and the tumor removed, or the biopsy incision closed and the mass returned to the orbital space depending on the outcome of the frozen tissue examination. Infiltrative and malignant tumors can be safely diagnosed, without fear of seeding, by this method of biopsy.
The Mayo series of primary, consecutive, neoplasms are listed in Table 15.2 with a comparison to other reported series of comparable size.
The total patients in the 50-year Mayo series is 1,795. The total of lacrimal gland tumors, of all types, is 118. Of these 118 cases, 70% (83 out of 118) are primary epithelial neoplasms. The remaining 30% are a variety of other tumor types. Ni and Ma (1995) made a retrospective study of 1,921 orbital tumors from the Eye Pathology of Shanghai Medical University. The author found 32% (138 out of 1,921) malignant lacrimal gland tumors and 13% (150 out of 1,921) benign mixed tumors. The total of these two subtypes is 288 cases, a total of 15% of all patients.
Benign Mixed Tumor (Pleomorphic Adenoma)
The term mixed tumor is a carryover from an earlier era when the histogenesis of the neoplasm was considered a mixture of epithelial and mesodermal elements. Later, the World Health Organization proposed the name pleomorphic adenoma, but the older name still persists in many publications.
Incidence
The age range of our 26 patients in the Mayo series is 16 to 81 years, with an average age of 41.8 years. There are 15 males and 11 females. There are two adolescents in the Mayo series, a 16-year-old boy and a 17-year-old girl. The tumor has been reported in children, a 7-year-old boy (McPherson, 1966), a 6-year-old boy (Faktorovich et al., 1996) and an adolescent 16-year-old girl (Tsunoda et al., 1994).
Clinical Features
In 50% of patients, the initial presenting sign is a painless, unilateral, slowly progressive proptosis associated with downward and inward displacement of one eye (see Fig. 15.1). In the other 50% of patients, a drooping of the upper eyelid is a presenting sign. Other symptoms or signs include a change in the refractive error induced by the pressure of the tumor on the eye, diplopia, or an ocular motility disturbance upon the superotemporal movement of the affected eye, an orbital “pressure” sensation, and puffiness of the upper eyelid. A palpable mass in the superotemporal orbital quadrant was present in 88% of our patients on initial examination. In the three patients without a palpable mass, the tumor had extended posteriorly instead of the usual upward, forward, or downward expansion of tumor. The mass is usually not tender. The palpable mass represents only a small part of the total volume of the tumor (the “tip of the iceberg”). Almost all mixed tumors are larger than 2 cm when uncovered surgically. In recurrent tumors, multiple nodules may be palpable in areas of the orbit and adnexa rather than the superior temporal quadrant.
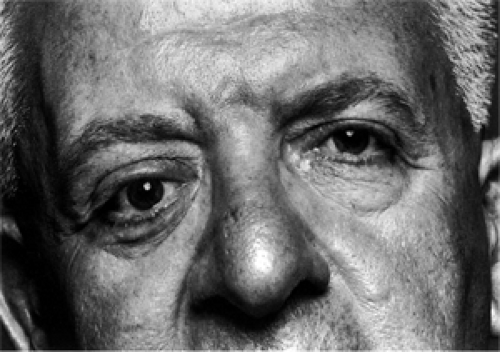 Figure 15.1 Benign mixed tumor: A 65-year-old man with prominence and downward displacement of the right eye of 6 months’ duration. |
Choroidal folds may also be noted at the time of the initial presentation depending on the size of the neoplasm. A rare condition that may also produce an inward and downward displacement of the eye is a hematocele of the lateral portion of the orbitofrontal bone plate.
A less common clinical aspect of this neoplasm is its presentation as a mass in the palpebral lobe of the lacrimal gland (Parks and Glover, 1990: four cases; Murphy and Rodrigues, 1974: two cases; Auran et al., 1988). The age range of these seven cases, 23 to 69 years, parallels the age span of patients with orbital lobe involvement. The palpebral lobe masses were approximately 10 × 10 mm in size when first seen, nontender, freely moveable, and did not present into the superior conjunctival fornix when the upper lid was everted. A tumor of the palpebral lobe does not produce proptosis because it is exterior to the orbital space. Vangveeravong et al. (1996) reported six tumors arising in the palpebral lobe of the lacrimal gland. Three of these were pleomorphic adenomas.
Several unusual manifestations of benign mixed tumors have been reported in the recent literature. Christie et al. (1995) excised a well-circumscribed mass from the lacrimal gland fossa of the right orbit of a 57-year-old woman. The mass proved to be a combination of a small benign mixed tumor and a large ductal cyst, dacryops, of the lacrimal gland. Guerra et al. (2000) described a huge, tender, well-defined
globular mass (8 × 5 × 4.5 cm size) protruding from the superolateral left upper eyelid that concealed a blind eye for 6 years in a 24-year-old man. The mass was completely excised and proved to be a giant pleomorphic adenoma of the lacrimal gland.
globular mass (8 × 5 × 4.5 cm size) protruding from the superolateral left upper eyelid that concealed a blind eye for 6 years in a 24-year-old man. The mass was completely excised and proved to be a giant pleomorphic adenoma of the lacrimal gland.
Imaging Aspects
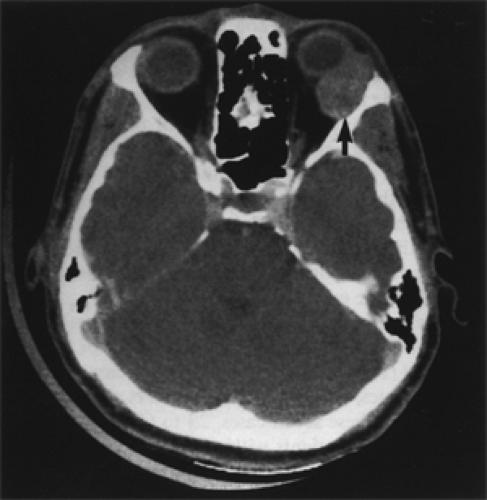
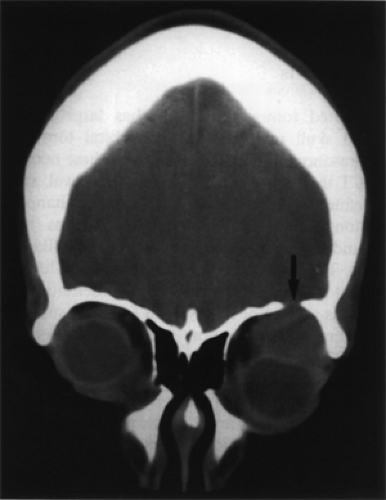
With CT scan and magnetic resonance imaging (MRI), benign mixed tumors are either round or oval, smooth, well-defined, and show mild to moderate enhancement. Some long-standing tumors show lobulations (bosselations) and scattered radiolucent areas (cystic-like degeneration). The presence or absence of calcific-like densities is not of diagnostic significance. Indentation of the contiguous surface of the eye is a frequent supplementary feature in those tumors showing posterior expansion (see Fig. 15.2).
The proximity of the initial focus of tumor to bone, its direction of expansion (superiorly or laterally), and tumor size (its duration) are the factors that determine the presence of radiographic changes in bone. In order of frequency, the bony changes are fossa formation (pressure erosion), increased bone density (reactive sclerosis), and bone destruction. Forty-four percent (11 out of 25) of our patients showed some degree of bony involvement. One of our cases showed a 1 cm defect in the orbital roof (see Fig. 15.3). A similar-sized defect was noted in the orbital roof of a patient reported by Hornblass et al. (1981). MRI shows long T1 and long T2 signal characteristics, but some tumors may be heterogeneous on T2-weighted imaging. The size and position of the orbital mass and the presence or absence of bone defects are the important imaging features the surgeon needs to know when planning his surgical approach.
Pathology
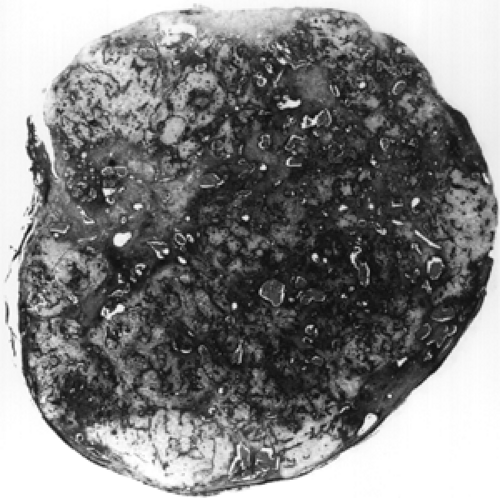
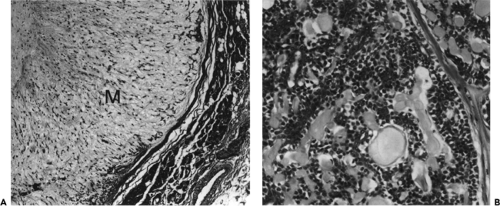
Grossly, the tumor is grayish-white, unilobular, slightly bosselated, and well delineated by a thin pseudocapsule (compression capsule) (see Fig. 15.4). When sectioned, the specimen is less solid than suggested by its surface, consisting of lobules of different density, separated by scanty connective tissue septa and scattered areas of cyst-like degeneration and focal hemorrhage. Under low-power magnification, the tumor consists of alternating areas of myxoid tissue, cellular islands of epithelial cells interspersed with ductal structures, hyaline cartilage, and bands of fibrous tissue (see Figs. 15.5 and 15.6). Small nests of tumor may also be seen outside the pseudocapsule intermingled with normal lacrimal tissue, the latter remaining attached to the tumor during its excision.
 Figure 15.4 Benign mixed tumor. Right: Surface of tumor is circumscribed and slightly bosselated. Left: Cut surface is lobulated and variegated in appearance. |
The epithelial cells consist of anastomosing ducts composed of two layers of cells. The basally located cells show the features of myoepithelial cells and may be cuboidal or spindle shaped. These cells merge into the stroma and undergo metaplasia to form the mesodermal-like elements (see Fig. 15.7). The lining epithelial cells are cuboid or even columnar. The central lumen of the ductal structure is either empty or contains mucous material that is characterized by its high content of neutral glycoprotein. This contrasts with the mucin of the stroma, which is a highly sulfated glycosaminoglycan. On occasion, keratin may be produced by the lining cells (see Fig. 15.8). In long-standing tumors, zones of cyst-like degeneration and hemorrhagic necrosis are also seen. Some pleomorphic adenomas are extremely cellular, and with recurrences, the tumor becomes increasingly cellular (see Fig. 15.9). These tumor cells are either round or spindle shaped, and the extreme cellularity may cause confusion with malignant tumors. The rarity of mitotic figures in the absence of necrosis is helpful in differentiating the tumor from a truly malignant neoplasm.
Immunohistochemistry
Grossniklaus et al. (1990) studied the immunohistochemical features of six benign and six malignant mixed tumors. They found that both types displayed similar ductal and myoepithelial characteristics. This underlies the belief that most malignant mixed tumors arise in a prior benign mixed tumor. The immunohistopathologic features indicated that the ductal epithelium of the normal lacrimal gland develops into the epithelial component of both benign and malignant mixed tumors of the lacrimal gland. Additionally, some of the myoepithelial cells of the normal lacrimal duct complex could be identified in the stromal component of both benign and malignant mixed tumors of the lacrimal gland.
Management and Course
The management of this tumor is complete removal, preferably with an intact capsule. In addition, a rim of the normal lacrimal gland surrounding the lesion should be included in the extirpation. The latter supplement will minimize any tumor seeding from the microscopic extension of the tumor into or through the compression capsule. This capsule, although thin, is, in the main, the most effective barrier to the escape of neoplastic elements into normal gland or orbital soft tissue. Because the capsule of the tumor is frequently fused laterally to the periorbita, we recommend that adjacent periorbita be included in the excision. The anterolateral orbitotomy is the preferred approach to best accomplish these goals.
Sixty percent of our patient cohort was managed in this manner. Follow-up data on all these patients were available with one exception. This exception was a patient
who was living 7 years after an intact removal of tumor, but no information was available concerning the presence or absence of the recurrence of neoplasm. The remaining 15 patients were free of recurrence with a mean follow-up of 9.7 years (range 3 to 21 years).
who was living 7 years after an intact removal of tumor, but no information was available concerning the presence or absence of the recurrence of neoplasm. The remaining 15 patients were free of recurrence with a mean follow-up of 9.7 years (range 3 to 21 years).
One patient with a 3-year follow-up, and two patients each followed for 10 years died from causes unrelated to their previous benign mixed tumor.
Four other patients did not have an intact removal of the tumor upon initial surgery at the Mayo Clinic. In two of these four patients, the capsule of the tumor ruptured near the completion of extirpation with escape of liquid contents into the surgical field. These patients have been followed up for 9 and 10 years, respectively, without local recurrence. In a third patient of this group, the tumor was so necrotic that only a piecemeal, but thorough, excision was accomplished. This patient was without recurrence of tumor for 8 years after surgery. In the fourth patient of this group, a guarded incisional biopsy was performed. When frozen tissue examination revealed a benign mixed tumor, the incisional breach of the capsule of the tumor was closed, followed up by an excision of the tumor without gross spillage of tumoral contents. There was no recurrence of the tumor at the 15-year follow-up.
Tang et al. (1997) reviewed 42 cases of benign mixed tumors which were followed up postoperatively, the follow-up periods ranging from 0.5 to 17 years. Thirty-four cases had no recurrence or malignant change, and eight cases had recurrences. Of the cases with recurrence, seven had several surgeries because of incomplete removal at the time of initial surgery. For successful surgery, they emphasized the need for complete removal of the tumor at the time of initial surgery and to avoid incisional or aspiration biopsy prior to surgery.
In summary, the surgeon who makes the initial surgical approach has the best chance to cure the patient by complete intact removal of the tumor.
Malignant Mixed Tumor
The lesion combines clinical and histologic features of pleomorphic adenoma and carcinoma of the lacrimal
gland. Its size, configuration, and clinical presentation may mimic the benign mixed tumor, but its course is comparable to carcinoma. Historically, the malignant mixed tumor was separated from other neoplasms in the lacrimal gland fossa 50 years ago (Forrest, 1954).
gland. Its size, configuration, and clinical presentation may mimic the benign mixed tumor, but its course is comparable to carcinoma. Historically, the malignant mixed tumor was separated from other neoplasms in the lacrimal gland fossa 50 years ago (Forrest, 1954).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree