Purpose
To investigate the prevalence of and risk factors associated with dry eye syndrome (DES) in South Korea.
Design
Cross-sectional study.
Methods
In 2010 and 2011, 11,666 subjects, ranging in age from 19 to 95, were randomly selected as nationally representative participants in the Korea National Health and Nutrition Examination Survey (KNHANES). Subjects were divided into 2 groups: 1 with clinically diagnosed DES and 1 with symptoms of dry eye. We determined the prevalence of and risk factors for dry eyes in a Korean population. Health-related quality of life (HRQoL), measured by the EuroQoL-5 dimension (EQ-5D), was evaluated in patients with dry eyes.
Results
The mean age was 49.9 years. The overall prevalence of diagnosed DES was 8.0% (95% confidence interval [CI], 7.3% to 8.7%), and of dry eye symptoms the prevalence was 14.4% (95% CI, 13.1 to 15.7). Age (adjusted odds ratio [aOR] = 1.8, 1.6), female (aOR = 2.8, 1.9); history of eye surgery (aOR = 2.6, 2.2); stress (aOR = 1.7, 1.6); thyroid disease (aOR = 1.7, 1.5); and high education level (aOR = 1.6, 1.5) were common risk factors in the groups. Subjects who had undergone ptosis, cataract or refractive surgery were more likely to have dry eye than subjects with no history of eye surgery. Means of pain and anxiety dimensions in the EQ-5D and the Euro Quality of Life Visual Analog Scale (EQ-VAS) were significantly higher in the group with diagnosed DES than in the normal group.
Conclusions
The risk factors were mostly similar in both groups. It is thought there are more patients with DES who have not been diagnosed by doctors. Doctors should identify whether a patient has any risk factors for dry eye. Patients need to be educated about the modifiable factors of DES.
Dry eye syndrome (DES) is the most common disease causing patients to visit ophthalmology clinics. The concept of DES has been understood as a multifactorial disease of the tears and ocular surface that is accompanied by increased osmolality of the tear film and inflammation of the ocular surface. The symptoms of DES are worse than simply discomfort; the condition disrupts activities of daily living and negatively affects quality of life. Thus, dry eye has recently been recognized as an important public health problem. A large-scale study of the prevalence of and risk factors for the disease is essential for planning therapeutic methods and prevention of the disease. The prevalence of DES has been reported in many studies to range from 5.5% to 33.7% and is generally known to be higher in Asians than Westerners. Typical risk factors for dry eye have been reported to include old age, female gender, smoking, and contact lens use. Most studies have reported prevalence of and risk factors for specific ages or within specific regions, but no data are available about the general population.
Thus, this study was conducted to analyze groups with dry eye prevalence and risk factors based on the data collected from a large-scale population study to find methods to prevent dry eye and improve patient quality of life.
Methods
The South Korea Center for Disease Control and Prevention conducted the Korea National Health and Nutrition Examination Survey (KNHANES) studies I, II and III in 1998, 2001 and 2005 to examine the general health and nutrition status of South Koreans. KNHANES V (2010–2012) involved a population-based random sampling of households across 576 national districts (192 per year), selected by a panel to represent the South Korean population using a stratified, multistage, clustered sampling method based on 2009 National Resident demographics. Detailed methodologies of these studies have been reported previously. This survey was reviewed and approved by the Institutional Review Board of the South Korea Centers for Disease Control and Prevention. All participants provided written informed consent. This cross-sectional prevalence study was conducted in accordance with the Declaration of Helsinki.
The KNHANES studies were divided into 3 parts: a health interview survey, a health examination survey and a nutrition survey. For the health interview survey, a trained interviewer asked questions directly of individuals 12 years of age and older.
Because the South Korean Ophthalmological Society participated in the survey, starting in July 2008, ophthalmologic interviews and examinations of the same participants have also been conducted. In 2010, to evaluate risk factors for dry eye specifically, interviews were conducted about dry eye. All members of each selected household were asked to participate in the survey; the rate of participation was, in fact, 82.0%. Participants older than 19 years of age underwent full ocular examinations, including auto refraction, visual acuity testing and slit-lamp examinations. This study included 11,666 adults 19 of age and older who completed a questionnaire regarding independent risk factors and underwent slit-lamp examinations.
Subjects were asked the following question: To date, have you ever before been diagnosed by a physician as having a dry eye (either eye)? The possible responses were yes or no. To make data collection more accurate, subjects were also asked the following question: Until now, have you ever had dry eye symptoms before; for example, dryness of the eye or a sense of irritation? Then the subjects were asked the question above with an emphasis on “by a physician.”
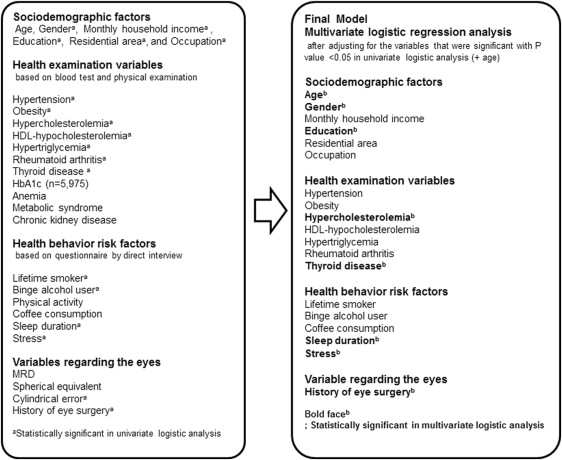
The independent variables were divided into 4 categories: (1) sociodemographic factors; (2) health examination variables; (3) health behavior risk factors; and (4) variables regarding the eye. The income per adult equivalent was calculated using the formula household income/square root of the number of people in the household. Binge alcohol users were defined as males who consumed more than 7 drinks on a single occasion or females who consumed more than 5 drinks on a single occasion at least once per month. Lifetime smokers included respondents who reported that they were current smokers and had smoked at least 100 cigarettes in their lifetimes. Medical histories of diseases, such as hypertension, rheumatoid arthritis, thyroid disease, and surgical history of the eyes, were obtained by health interviewers. Detailed definitions of other diseases were based on previously reported papers and are briefly described in the Figure .
The Euro quality of life-5 dimensions (EQ-5D) was also analyzed for an objective investigation of health status. The EQ-5D questionnaire is a standardized generic instrument for describing and evaluating health; it was designed by the EuroQol group, an international research network established in 1987. The EQ-5D self-reported questionnaire consists of a 5-dimensional descriptive system and a visual analog scale (EQ-VAS) together with brief demographic questions. The descriptive system defines health in term of 5 dimensions: mobility, self-care, usual activities, pain or discomfort, and anxiety or depression. Each dimension is divided into 3 levels, indicating no problem, some or moderate problems, or extreme problems.
Statistical Methods
Descriptive statistics are reported for each response. To determine the prevalence of dry eye in South Korea according to age groups, the prevalence was calculated using the weights defined by the guidelines of KNHANES V. To calculate the weights according to KNHANES V in accordance with the guidelines for the 2010 South Korean population (in accordance with the 2010 census of South Korea), a poststratification adjustment was performed, based on response and extraction rates, to include the distribution of the 2010 South Korean population according to gender and age groups at 5-year intervals. Finally, the sum of the weights according to KNHANES V is equal to the South Korean population of 2010.
Unfortunately, the data for high-density lipoprotein (HDL) cholesterol disclosed to the public were flawed because the test methods were changed in October 2011, and the HDL cholesterol data in 2011 needed additional validation. Regarding HDL cholesterol in this study, only data from 2010 were used for the multivariate logistic regression (number of subjects = 4640). We did not provide the entire multivariate analysis result set from the 2010 data and have simply inserted the result in the table because HDL cholesterol was ultimately not significant and did not affect other odds ratios significantly.
A 2-step, multidimensional approach was used to identify risk factors for dry eye. First, to identify risk factors associated with dry eye, odds ratios and 95% confidence intervals (CIs) were calculated using univariate logistic regression analysis. Second, multivariate logistic regression analysis was used to determine risk factors with each variable after adjusting for the variables that were significant (with P values of <0.05) in the univariate analyses. Some variables could be confounded by age, so multivariate analysis was performed to adjust for age. Ultimately, the final model included age, gender, monthly household income, education, residential area, occupation, hypertension, obesity, hypercholesterolemia, HDL-hypocholesterolemia, hypertriglyceridemia, rheumatoid arthritis, thyroid disease, lifetime smoker, binge alcohol user, sleep duration, stress, and history of eye surgery.
To evaluate which kinds of eye surgery were associated with dry eye, as diagnosed by a physician, or dry eye symptoms, adjusted proportions were calculated based on multivariable linear regression after adjusting for age, gender, education, thyroid disease, hypercholesterolemia, sleep duration, and stress, which were significant variables in the final model. The relationship between dry eye and EQ-5D was identified using unadjusted and adjusted means, based on linear regression analysis. All statistical tests were 2-sided at the 95% CI level and were performed using the Stata/SE 12.1 software (StataCorp, College Station, Texas, USA).
Results
The mean age of the 11,666 participants 19 years of age or older was 49.9 (SD, 16.7) years. Of the participants, 42.8% were males, and 78.5% were living in urban areas. Supplemental Table 1 provides the characteristics of the study population in greater detail.
The overall prevalence of patients with dry eye—with real diagnoses or with symptoms—was 16.0% (95% CI = 14.6% to 17.3%). The overall prevalence of dry eye diagnosed by a physician and dry eye symptoms was 8.0% (95% CI, 7.3% to 8.7%) and 14.4% (95% CI, 13.1% to 15.7%), respectively. The prevalence of patients with dry eye symptoms or with a diagnosis at the age of 40 or older was 10.7% for males (95% CI = 9.1 to 12.2) and 20.6% (95% CI = 18.5 to 22.7) for females. Table 1 shows the prevalence of dry eye by age and gender.
| Diagnosed DES | Symptoms of DES | Diagnosed DES or Symptoms of DES | ||||
|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | |
| All | ||||||
| 19–29 | 8.3 | (6.8–10.1) | 15.1 | (12.9–17.6) | 16.8 | (14.5–19.4) |
| 30–39 | 7.8 | (6.4–9.4) | 13.8 | (11.9–15.9) | 15.5 | (13.5–17.8) |
| 40–49 | 7.1 | (6.0–8.4) | 12.9 | (10.9–15.1) | 14.6 | (12.5–17.0) |
| 50–59 | 8.9 | (7.5–10.5) | 15.2 | (13.2–17.5) | 17.1 | (14.9–19.5) |
| 60–69 | 9.1 | (7.6–10.9) | 16.2 | (13.9–18.8) | 17.0 | (14.6–19.7) |
| 70– | 6.7 | (5.4–8.2) | 14.1 | (11.7–16.7) | 15.0 | (12.7–17.8) |
| Men | ||||||
| 19–29 | 3.6 | (2.3–5.8) | 9.9 | (7.6–12.8) | 10.1 | (7.4–12.8) |
| 30–39 | 3.7 | (2.5–5.3) | 9.5 | (7.4–12.1) | 10.3 | (7.9–12.7) |
| 40–49 | 3.5 | (2.5–5.0) | 8.8 | (6.7–11.5) | 9.8 | (7.3–12.2) |
| 50–59 | 3.2 | (2.2–4.7) | 8.6 | (6.6–11.2) | 9.5 | (9.3–13.2) |
| 60–69 | 5.9 | (4.1–8.2) | 11.4 | (8.8–14.7) | 12.3 | (9.6–15.7) |
| 70– | 4.9 | (3.5–6.7) | 13.1 | (10.1–16.7) | 13.9 | (10.9–17.6) |
| Women | ||||||
| 19–29 | 13.3 | (10.8–16.3) | 20.7 | (17.4–24.4) | 23.8 | (20.1–27.6) |
| 30–39 | 12.0 | (9.8–14.7) | 18.1 | (15.4–21.2) | 20.8 | (17.7–23.9) |
| 40–49 | 10.8 | (8.9–13.0) | 17.0 | (14.3–20.2) | 19.7 | (16.5–22.8) |
| 50–59 | 14.5 | (12.2–17.2) | 21.7 | (18.7–25.1) | 21.1 | (18.7–23.5) |
| 60–69 | 12.1 | (9.8–14.7) | 20.3 | (17.1–24.0) | 21.2 | (17.9–24.9) |
| 70– | 7.8 | (6.0–10.0) | 14.7 | (11.8–18.1) | 15.7 | (12.7–19.3) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


