Some women with Meniere disease demonstrate exacerbation of symptoms during the premenstrual period. It is believed that the hormonal stress of the premenstrual period acts on the volatile inner ear with Meniere disease to result in dysfunction. Migraine, Meniere disease, and the premenstrual period may be a complex interaction leading to exacerbation of symptoms. Having patients maintain a daily calendar of symptoms, diet, and menses can be helpful in understanding the disease as well as instigating treatment monitoring. Most patients can be effectively managed with dietary sodium restriction and a loop diuretic.
A goal of identifying and studying a subpopulation of patients within a disease entity is to better understand the etiology and pathophysiology of the condition so that this information can be applied to the disease in general. Such is the case in Meniere’s disease where the subpopulation is identified as those women who have typical symptoms, including ear congestion, fluctuating heaing loss, tinnitus, and crises of vertigo exacerbated during the late luteal phase of the menstrual cycle (premenstrual period).
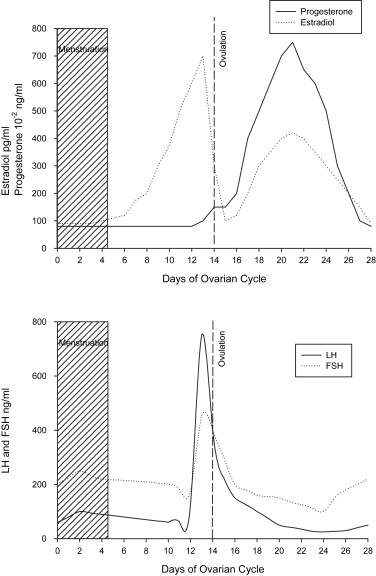
Menses occurs to prepare the uterus for ovulation. The entire cycle ( Fig. 1 ) is dependent on gonadotropic hormones from the anterior pituitary, follicle-stimulating hormone, and luteinizing hormone. The follicular phase of the ovarian cycle occurs with follicle-stimulating hormone acting on the ovum to enlarge and produce various layers, including the theca and granulosa cells, which are primarily responsible for secreting the estrogens and, to a lesser degree, progesterone. Approximately 2 days before ovulation, there is an increase in production of luteinizing hormone, eventually reaching 6 to 10 times its base concentration approximately 18 hours before ovulation. An increase in follicle-stimulating hormone also occurs over this same time period but only increases in 2-fold concentration. The luteinizing hormone causes the theca and granulosa cells to become lutein cells, which secrete progesterone and much less estrogen. There is follicle swelling, degeneration, and rupture that results in release of the ovum. The luteal phase of the ovarian cycle then begins. The remaining theca cells enlarge and undergo luteinization to become the corpus luteum. Once formed, the corpus luteum undergoes a sequential program of proliferation, enlargement, secretion, and degeneration. During its secretory phase, the corpus luteum is producing large amounts of progesterone and estrogen. This increase in progesterone and estrogen acts on the anterior pituitary in a feedback mechanism to suppress production of luteinizing and follicle-stimulating hormone. With degeneration of the corpus luteum, there is a drop in progesterone and estrogen levels, which allows for a surge in luteinizing and follicle-stimulating hormone. A new ovarian cycle begins.
Report of a case
A 34-year-old woman presented to the authors’ clinic with a 7-year history of previously diagnosed Meniere’s disease, noting repeated bouts of left-sided hearing loss with documented low-frequency audiometric threshold shifts, low-frequency tinnitus, ear congestion, and sometimes vertigo. The vertigo bouts were severe and could last several hours and usually were associated with nausea and sometimes vomiting. She noted a long history of being treated for migraine headaches with typical aura at their onset, which at times could be associated with her otologic symptoms. She found some relief in lying down in a dark room until they subsided, which required some hours. Approximately 2 years previously she had a period of freedom from symptoms for approximately 15 months from both Meniere’s and migraine during and after the pregnancy of her first child, whom she subsequently nursed. At the time of her presentation she was on Loestrin 24 (ethinyl estradiol and norethindrone acetate) for birth control and using Diamox (acetazolamide) in attempt to control her Meniere’s and migraine symptoms. After trial of various medical regiments, she eventually found success in using a combination of verapamil and Dyazide (triamterene and hydrocholorothiazide) with a low salt diet (<1500 mg sodium per day). She decided to have another child and discontinued her medication although continued with the low salt diet. By having the patient maintain a daily calendar by logging her symptoms and menses, it became notable that her symptoms of unilateral tinnitus and ear congestion were present most of the time but would become more intense during the premenstrual period as would fluctuations in hearing ( Fig. 2 ). Some of the premenstrual periods were associated with pronounced episodes of vertigo lasting hours to days. Again, she became pregnant. The tinnitus and congestion continued into the first trimester but hearing fluctuations, vertigo, and headaches improved. The events in this patient are consistent with the putative role of the menstrual cycle in triggering the symptoms of Meniere’s disease.
Literature review
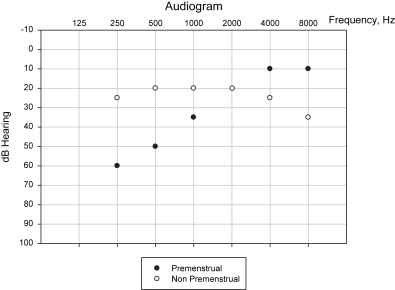
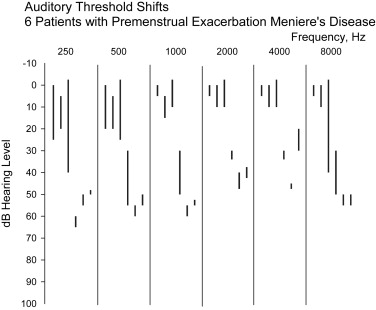
In 1992, the authors reviewed 109 women with Meniere’s disease; 6 were identified with exacerbation of symptoms during the premenstrual period. This was noted by having the patients maintain a calendar and documenting the days of menstrual bleeding as well as symptoms of dizziness, unilateral hearing loss, aural pressure, and tinnitus throughout the month. Although primarily the correlation of the patients’ symptoms with the premenstrual period was used to make this diagnosis, serial audiograms were performed showing typical auditory threshold shifts to support this correlation. Within this study, two subgroups of patients could be identified: first, those with early-onset Meniere’s disease whose auditory dysfunction was considered reversible, and second, those with long-standing Meniere’s disease whose auditory dysfunction was considered irreversible. The patients with reversible disease did not always demonstrate the full spectrum of Meniere’s disease initially. Their auditory threshold shifts were considerably more marked and involved all frequencies ( Figs. 2 and 3 ). Those with irreversible or long-standing Meniere’s disease demonstrated the full spectrum of symptoms all along during the premenstrual period. Their initial auditory thresholds were worse and showed more limited fluctuation.
All patients were managed with a low salt diet and the loop diuretic is triamterene and hydrochlorothiazide (Dyazide). All patients demonstrated control of their vestibular crises symptoms. Those with reversible auditory dysfunction were able to maintain normal hearing. Those with irreversible auditory dysfunction showed stabilization of their hearing but no further improvement. This study again implicates the premenstrual period as an exacerbating factor in the manifestation of symptoms in some women with Meniere’s disease.
In another reported study of 5 women with Meniere’s disease who could correlate symptoms with their menstrual cycle, two noted their symptoms some days before the menses and three noted their symptoms concomitantly occurred with the menses or immediately thereafter. During pregnancy, vertigo symptoms markedly improved. After the pregnancy, some patients noted the return of Meniere’s symptoms with their menstrual cycle. With interruption of the menstrual cycles by pregnancy, there was improvement in the Meniere’s symptoms, only to have them return after childbirth. This report provides further evidence of the premenstrual period as the aggravating factor in this group of Meniere’s patients.
In an Internet-based research study, subjects with Meniere’s disease were recruited from a website. In the first phase of the study, 42 women with purported Meniere’s disease were identified that could correlate the symptoms of their condition with the menstrual cycle. In the second phase of the study, 20 women were invited to participate by maintaining calendars and filling out questionnaires to assess their condition on a daily basis. They were compared with 17 men with Meniere’s disease as a control. In the third phase of the study, the female subjects were asked to use over-the-counter urinary ovulation kits, which were then returned by mail to the investigators to analyze more specifically the timing of ovulation to compare with their reported symptoms. Eleven women were able to complete the study. Vertigo was noted as the significant symptom that would diminish post menses in those women with premenstrual exacerbation of Meniere’s disease.
There are several additional case reports regarding premenstrual symptoms of fluctuating hearing loss, tinnitus, and vertigo. In some of these reports, symptoms develop bilaterally. In others, symptoms are unilateral and exacerbated during the premenstrual period.
Price and colleagues describe a patient with Meniere’s disease exacerbated during the luteal phase of the menstrual cycle. The patient’s symptoms were completely controlled using leuprolide acetate (a gonadotropin-releasing hormone) but returned on cessation of treatment. Andreyko and Jaffe described a patient with a 40-dB auditory threshold fluctuation, which always occurred in the luteal phase of her menstrual cycle. Similarly, her symptoms were completely controlled with nafarelin (a gonadotropin-releasing hormonal agonist) only to return after the cessation of this medication. The use of gonadotropin-releasing hormones is to bind to the pituitary gonadotropin-releasing hormone receptors and suppress gonadotropin secretion, resulting in the cessation of ovulation. With complete interruption of the menstrual cycle, these patients’ disease was controlled. Together, all these reports corroborate that the fundamental pathology of the inner ear symptoms were associated with the premenstrual period.
Literature review
In 1992, the authors reviewed 109 women with Meniere’s disease; 6 were identified with exacerbation of symptoms during the premenstrual period. This was noted by having the patients maintain a calendar and documenting the days of menstrual bleeding as well as symptoms of dizziness, unilateral hearing loss, aural pressure, and tinnitus throughout the month. Although primarily the correlation of the patients’ symptoms with the premenstrual period was used to make this diagnosis, serial audiograms were performed showing typical auditory threshold shifts to support this correlation. Within this study, two subgroups of patients could be identified: first, those with early-onset Meniere’s disease whose auditory dysfunction was considered reversible, and second, those with long-standing Meniere’s disease whose auditory dysfunction was considered irreversible. The patients with reversible disease did not always demonstrate the full spectrum of Meniere’s disease initially. Their auditory threshold shifts were considerably more marked and involved all frequencies ( Figs. 2 and 3 ). Those with irreversible or long-standing Meniere’s disease demonstrated the full spectrum of symptoms all along during the premenstrual period. Their initial auditory thresholds were worse and showed more limited fluctuation.
All patients were managed with a low salt diet and the loop diuretic is triamterene and hydrochlorothiazide (Dyazide). All patients demonstrated control of their vestibular crises symptoms. Those with reversible auditory dysfunction were able to maintain normal hearing. Those with irreversible auditory dysfunction showed stabilization of their hearing but no further improvement. This study again implicates the premenstrual period as an exacerbating factor in the manifestation of symptoms in some women with Meniere’s disease.
In another reported study of 5 women with Meniere’s disease who could correlate symptoms with their menstrual cycle, two noted their symptoms some days before the menses and three noted their symptoms concomitantly occurred with the menses or immediately thereafter. During pregnancy, vertigo symptoms markedly improved. After the pregnancy, some patients noted the return of Meniere’s symptoms with their menstrual cycle. With interruption of the menstrual cycles by pregnancy, there was improvement in the Meniere’s symptoms, only to have them return after childbirth. This report provides further evidence of the premenstrual period as the aggravating factor in this group of Meniere’s patients.
In an Internet-based research study, subjects with Meniere’s disease were recruited from a website. In the first phase of the study, 42 women with purported Meniere’s disease were identified that could correlate the symptoms of their condition with the menstrual cycle. In the second phase of the study, 20 women were invited to participate by maintaining calendars and filling out questionnaires to assess their condition on a daily basis. They were compared with 17 men with Meniere’s disease as a control. In the third phase of the study, the female subjects were asked to use over-the-counter urinary ovulation kits, which were then returned by mail to the investigators to analyze more specifically the timing of ovulation to compare with their reported symptoms. Eleven women were able to complete the study. Vertigo was noted as the significant symptom that would diminish post menses in those women with premenstrual exacerbation of Meniere’s disease.
There are several additional case reports regarding premenstrual symptoms of fluctuating hearing loss, tinnitus, and vertigo. In some of these reports, symptoms develop bilaterally. In others, symptoms are unilateral and exacerbated during the premenstrual period.
Price and colleagues describe a patient with Meniere’s disease exacerbated during the luteal phase of the menstrual cycle. The patient’s symptoms were completely controlled using leuprolide acetate (a gonadotropin-releasing hormone) but returned on cessation of treatment. Andreyko and Jaffe described a patient with a 40-dB auditory threshold fluctuation, which always occurred in the luteal phase of her menstrual cycle. Similarly, her symptoms were completely controlled with nafarelin (a gonadotropin-releasing hormonal agonist) only to return after the cessation of this medication. The use of gonadotropin-releasing hormones is to bind to the pituitary gonadotropin-releasing hormone receptors and suppress gonadotropin secretion, resulting in the cessation of ovulation. With complete interruption of the menstrual cycle, these patients’ disease was controlled. Together, all these reports corroborate that the fundamental pathology of the inner ear symptoms were associated with the premenstrual period.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


