Purpose
To evaluate the effectiveness of pre-seasonal treatment with topical olopatadine on the reduction of clinical symptoms of seasonal allergic conjunctivitis (SAC).
Design
Prospective interventional case series.
Methods
Eleven patients with SAC received topical olopatadine in one eye at least two weeks before the onset of allergy symptoms, and the other eye served as the control. After the onset of allergic conjunctivitis, both eyes were treated with topical olopatadine. Visual analogue scale (VAS), which evaluated the subjective symptoms of ocular allergy, and the tear levels of histamine and substance P were measured up to six weeks.
Results
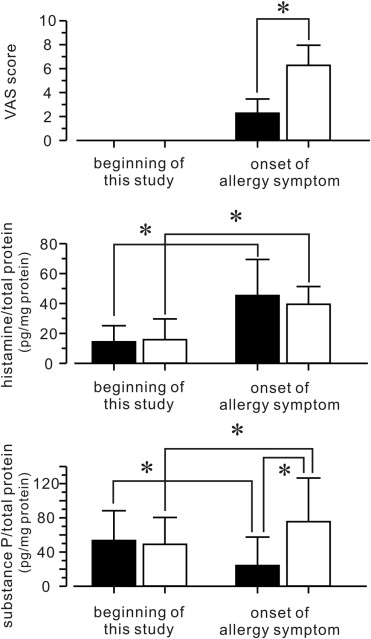
At the onset of allergy symptoms, the VAS score in the pretreatment eyes was statistically significantly lower than that in the control eyes. The VAS score in the control eyes decreased with time but did not decrease to the level seen in the pretreatment eyes until four weeks later. The tear level of substance P at the onset of allergy symptoms was significantly suppressed in the pretreatment eyes, while the level of histamine was not suppressed. Alteration of the VAS scores in the pretreatment eyes significantly correlated with the level of substance P, but not of histamine.
Conculsions
To suppress clinical symptoms in patients with SAC, pre-seasonal treatment with topical olopatadine is effective. The effectiveness of treatment correlates with the tear level of substance P.
Seasonal allergic conjunctivitis (SAC) is the most prevalent ocular allergy, affecting approximately 25% of the US population. SAC is usually an acute or subacute condition characterized by self-limited signs and symptoms that become persistent with repeated allergen exposure during pollen season. The hallmark signs and symptoms are itching, redness, and lid swelling, along with tearing, mucous discharge, and burning.
The allergic response in conjunctivitis is typically elicited by ocular exposure to allergens that causes cross-linkage of membrane-bound IgE, which triggers mast cell degranulation, releasing a cascade of allergic and inflammatory mediators. Histamine is the major mediator contributing to the development of the early-phase signs and symptoms of seasonal allergic conjunctivitis. Two types of histamine receptors, H 1 and H 2 , have been identified in the human conjunctiva. The activation of H 1 receptors induces itching, whereas activation of vascular endothelial cells through the actions of both H 1 and H 2 receptors induces hyperemia attributable to vasodilation and eyelid swelling and chemosis attributable to the transduction of fluid. Several different drugs target mast cells and histamine receptors in order to reduce this allergic response in patients with SAC.
A bidirectional regulation of neuronal stimulation and allergic response has been theorized to occur during allergic inflammation. Neuromediators represent the key factor in this process, working on either immune or structural cells and exerting neuroimmunomodulatory functions in maintaining homeostasis and an inflammatory tissue remodeling system. Substance P is the representative neuromediator involved in allergic inflammation and contributes to the severity of ocular allergy symptoms. However, little is known about the regulation of substance P secretion by anti-allergic ophthalmic drugs in patients with SAC.
Although pre-seasonal administration of multiple-action drugs, which combine antihistamine effects, mast cell stabilization, and anti-inflammatory actions, is believed to suppress the ocular allergy signs and symptoms of itching, redness, chemosis, tearing, and lid swelling, the efficacy of this treatment option has not been investigated. Olopatadine hydrochloride 0.1% ophthalmic solution is one of these multiple-action drugs and has recently become the primary medication choice for prevention and treatment of allergic conjunctivitis.
In this prospective study, we investigated whether pre-seasonal administration of the multiple-action drug olopatadine suppressed ocular allergy symptoms at the onset of SAC; and the concentrations of the chemical mediator “histamine” and the neuromediator “substance P” in tears, with and without pre-seasonal treatment, were measured to assess their correlation with the severity of disease.
Methods
Patient Eligibility
Patients who had a history of seasonal allergic conjunctivitis to cedar pollen in both eyes, with a serum level of IgE specific to cedar pollen of greater than 4 IU/mL (class 3), and had itching and signs of ocular allergy every year during cedar pollen season were recruited for this study. The following patients were excluded from the study: those who 1) had any ocular disease other than allergic conjunctivitis; 2) used systemic or topical concomitant medications including corticosteroids, nosteroidal anti-inflammatory drugs, anticholinergics, and immunosuppressives; 3) suffered from severe ocular allergic diseases such as those associated with giant papilla formation; or 4) needed to wear contact lenses during the treatment period. Written informed consent was obtained from all patients.
Outcome Measures
To evaluate the severity of subjective symptoms including conjunctival itching, injection, discharge, lacrimation, and foreign body sensation, a visual analogue scale (VAS; 0 = none to 10 = most severe) was adopted. Tears were collected from both eyes of each patient using a glass capillary with a filament (GDC-1, Narishige Scientific Instrument Lab, Tokyo, Japan) placed at the inferior tear meniscus for 30 to 60 seconds. A total volume of 20 to 50 μL was easily collected with this unique technique ( video available at AJO.com ). After the collection of samples, both sides of the glass capillary were sealed with clay and immediately transferred on ice to the laboratory. The specimens were stored at −80°C.
The levels of histamine and substance P in the tears were determined using commercially available competitive enzyme-linked immunosorbent assay kits from Oxford Biomedical Research, Inc (Oxford, Michigan, USA) and Assay Designs, Inc (Ann Arbor, Michigan, USA), respectively. Total protein was quantified with the BCA Protein Assay Reagent from PIERCE Biotechnology, Inc (Rockford, Illinois, USA). Tear samples were prepared by appropriate dilutions for measurement of substance P, histamine, and total protein. Each assay was performed according to the manufacturer’s direction.
Study Design
This study was conducted from January 2009 to April 2009. Initial examination of each eligible patient was completed by the middle of February 2009 because the beginning of cedar pollen season in this area of Sendai city in Japan, is usually at the end of February every year. At the beginning of the study, it was confirmed that the patients did not have symptoms of allergic conjunctivitis in either eye (VAS = 0 in both eyes). Subsequently one eye received topical administration of olopatadine hydrochloride 0.1% ophthalmic solution (Patanol; Alcon Laboratories, Fort Worth, Texas, USA) four times per day, and the other eye served as the control. To perform precise case-control study, the other eye should received Patanol without olopatadine hydrochloride; however, such an ophthalmic solution is not commercially available. Also, Patanol contains benzalkonium chloride (BAC) as preservative and administration of only BAC to preclinical SAC patients was not permitted by the Institutional Review Board (IRB), NTT East Japan Tohoku Hospital. Also in clinical phase, patients with SAC either receive or do not receive pre-seasonal administration of anti-allergic eye drugs; thus the IRB had recommended the other control eye without any eye drops until the onset of allergy symptoms.
At the onset of allergy symptoms, olopatadine was administered to both eyes. Ocular examination including VAS scoring and tear collection from both eyes was performed at the initial examination, at the onset of allergy symptoms, and at two, four, and six weeks after the onset of allergy symptoms. Alterations in the levels of the chemical mediators were assessed using the ratio of chemical mediators to total protein.
Statistics
Obtained data do not always follow a metric scale, so statistical analyses were done with the Wilcoxon signed rank test (pretreatment and posttreatment data in the same eye) and with the Mann-Whitney U test (data for treated and control groups) as appropriate using a statistical program (SPSS Science, Chicago, Illinois, USA). To investigate the correlation between levels of chemical mediators and VAS, the Pearson correlation coefficient ( r ) and a P value were calculated. Since the number of samples was 11, an r 2 value of more than 0.3 (| r | > 0.6) was considered statistically significant and defined as a strong correlation. All of the data are presented as means ± standard deviations.
Results
Eleven patients (mean age 40.3 ± 12.6 years) with seasonal allergic conjunctivitis in both eyes participated in this study. Seven patients were male and four were female. The average level of serum IgE specific for cedar pollen was 23.8 ± 26.8 IU/mL.
No ocular or systemic side effects of the study drug were observed in any participants.
Initial Examination Prior to the Onset of Cedar Pollen Season
At the beginning of this study, the VAS score of both eyes in all patients was confirmed to be 0. The total protein (TP) level in tears from the treated eyes was 7.83 ± 5.09 mg/mL, which was not significantly different from the level in the control eyes of 8.57 ± 6.47 mg/mL. The histamine level in tears from the treated eyes was 1.04 ± 1.09 ng/mL, and the level in the control eyes was 1.23 ± 1.40 ng/mL. The substance P level in tears from the treated eyes was 3.60 ± 2.33 ng/mL, and the level from the control eyes was 3.79 ± 2.53 ng/mL.
The level of TP varied according to the day of tear collection even in the same patient. The ratios of histamine/TP and substance P/TP were calculated and adopted for this comparative study. The histamine/TP level in tears was not significantly different between the treated eyes (14.4 ± 10.6 pg/mg protein) and the control eyes (15.8 ± 13.9 pg/mg protein). The substance P/TP level in tears was also not significantly different between the treated eyes (53.5 ± 34.8 pg/mg protein) and the control eyes (49.0 ± 31.4 pg/mg protein).
Effectiveness of Pre-seasonal Therapy at the Onset of Allergy Symptoms
Although cedar pollen season began on February 26, clinical allergy symptoms were not seen in any of the patients until after March 7. The average duration of pre-seasonal therapy was 27.9 ± 13.5 days.
At the onset of allergy symptoms (week 0), the VAS score in the treated eyes averaged 2.27 ± 1.19, which is significantly lower than the VAS score in the control eyes of 6.27 ± 1.68 ( P = .0001) ( Figure 1 , Top) The histamine/TP level in tears was significantly elevated to 45.31 ± 24.11 pg/mg protein in the treated eyes ( P = .0067) and to 39.46 ± 11.87 pg/mg protein in the control eyes ( P = .0076). However, there was no significant difference in the histamine/TP level in tears from the treated eyes and the control eyes ( P = .5767) ( Figure 1 , Middle). While substance P/TP level in tears was significantly decreased to 24.16 ± 33.32 pg/mg protein in the treated eyes ( P = .0469), it was significantly increased to 75.49 ± 51.26 pg/mg protein in the control eyes ( P = .0367). There was also a significant difference in the substance P/TP level in tears from the treated eyes and the control eyes ( P = .0138) ( Figure 1 , Bottom).
Contribution of Chemical Mediators to Allergy Symptoms
The relationship between the VAS score at the onset of allergy symptoms and the alteration of histamine/TP, which is defined as subtraction of the ratio at the onset of symptoms from the ratio at the beginning of this study, is depicted in Figure 2 (Top). Although there is no significant correlation ( r 2 = 0.081, P = .409) in the treated eyes, there is a significant correlation ( r 2 = 0.711, P = .001) in the control eyes. The relationship between the VAS score and the alteration of substance P/TP is depicted in Figure 2 (Bottom). In contrast, although there is a significant correlation in the treated eyes ( r 2 = 0.379, P = .039), there is no significant correlation in the control eyes ( r 2 = 0.094, P = .371).




