Purpose
To present a new complication of persistent corneal edema after collagen cross-linking (CXL) in keratoconus patients.
Design
Retrospective case series of postoperative corneal edema after CXL.
Methods
study population: All patients who underwent CXL treatment with subsequent corneal edema. Patients with stromal haze were excluded. intervention: The CXL treatments used the Dresden protocol with corneal thickness of more than 400 μm after epithelium was removed. main outcome measure: The resolution of corneal edema after surgery.
Results
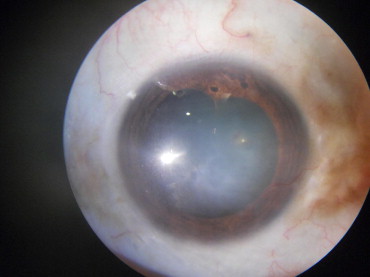
Postoperative corneal edema was identified in 10 (2.9%) of 350 patients who were followed up for a mean of 14 ± 4 months. The edema started on postoperative day 1 (10/10) and increased for 3 weeks. Additional findings included: deep vascularization (2 eyes; 20%), iris atrophy (6 eyes; 60%), pigment dispersion (5 eyes; 50%), persistent epithelial defect (3 eyes; 30%), and infectious keratitis (1 eye; 10%). Specular microscopy was unsuccessful, but the fellow untreated eyes had normal endothelial counts. Intraocular pressure and lenticular evaluations were normal. Corneal edema improved in 4 patients and resolved in 1 patient. In these 5 patients, the logarithm of the minimal angle of resolution best-corrected visual acuity was 0.5 ± 0.18. Penetrating keratoplasty was offered to 5 patients when improvement plateaued at 3 months, but only 2 patients underwent penetrating keratoplasty.
Conclusions
CXL is a safe and effective procedure with few known side effects. This case series reports the possibility of corneal endothelial damage with visually significant corneal edema after CXL treatment. Based on the extent of endothelial damage, patients may require penetrating keratoplasty.
Keratoconus is a bilateral, asymmetric, noninflammatory, progressive ectatic degeneration resulting in stromal thinning and distortion of the cornea. Depending on the severity and progression of the disease, it can be treated with spectacles, rigid gas permeable contact lenses, intracorneal ring segments, deep anterior lamellar keratoplasty, or penetrating keratoplasty. Recently, collagen cross-linking (CXL) with riboflavin drops has been reported to be effective in increasing the biomechanical strength and stability of the cornea. CXL, if preformed according to standard protocols, has been found to be a safe procedure. Despite the high safety profile reported, there are a few reports of adverse events after CXL. Persistent corneal haze is one of the more frequently reported complications of CXL. In addition, a few cases of infectious keratitis after CXL have been reported. Furthermore, Gokhale recently reported a single case of CXL-induced corneal endothelial cell damage resulting in corneal edema. We observed several cases of persistent corneal edema after CXL for treatment of progressive keratoconus and have evaluated this case series of 10 patients.
Methods
After approval from the Cornea Centre Institutional Review Board, a retrospective chart review of all patients treated with CXL for progressive keratoconus from July 1, 2008, through June 30, 2011, was conducted. These charts were reviewed for any complications of the treatment. Patients who were treated for persistent stromal haze were excluded from the study. Patients in whom corneal edema developed that persisted for more than 3 weeks were included in the study.
Data acquisition included preoperative and postoperative best-corrected visual acuity, refraction, keratometry, pachymetry, and corneal topography. Pachymetry readings were obtained from a Pentacam (Pentacam Oculyzer; Oculus Optikgerate GmbH, Heidelberg, Germany) to eliminate the chance of missing the thinnest point in the cornea that could be missed by ultrasonic pachymeter. The details of the surgical procedure, including frequency of riboflavin drops, total energy delivered, and any deviation from the Dresden protocol, were recorded. The postoperative anterior segment findings and duration of symptoms also were evaluated.
Collagen Cross-Linking Procedure
The CXL treatment was preformed as an outpatient procedure following the Dresden protocol by an experienced ophthalmologist (K.Mi.). The treatment was performed under sterile conditions in an operating theater. After obtaining informed consent, the ocular surface was anesthetized with topical proparacaine hydrochloride 0.5% solution. An eyelid speculum was inserted, and the corneal epithelium was removed using a hockey stick blade (Grieshaber; Alcon, Schaffhausen, Switzerland). The epithelium was debrided to expose 80% to 90% of the central cornea. The corneal thickness was measured after the epithelium was removed to confirm a thickness of more than 400 μm in all cases. Next, isotonic riboflavin 0.1% drops (Medio-Cross; Medizinprodukte GmbH, Neudorf, Germany) were instilled every 2 minutes for 30 minutes, concurrent with instillation of topical proparacaine. The corneas then were exposed to ultraviolet A light (UV-X System; Peschke Meditrade GmbH, Huenenberg, Switzerland) for 30 minutes. Administration of additional isotonic riboflavin drops occurred every 3 minutes during the ultraviolet A exposure. The parameters of emitted ultraviolet light included: wavelength, 370 nm; irradiance, 3 mW/cm 2 ; and diameter, 7.5 mm. A calibrated ultraviolet meter was used to confirm the irradiance (3.0 mW/cm 2 ) before each treatment session; however, the corneal thickness was not remeasured during the ultraviolet exposure. After completion of ultraviolet A exposure, the eyelid speculum was removed and a drop of moxifloxacin hydrochloride ophthalmic solution 0.5% (Cipla Ltd, Roorkee, India) was instilled. An eye pad and shield then were applied. The standard postoperative treatment included both moxifloxacin hydrochloride ophthalmic solution 0.5% and carboxymethyl cellulose (Allergan, Karnataka, India) 4 times daily. For pain control, the patient also was prescribed Combiflam (combination pill of ibuprofen and acetaminophen; Aventis, Akhleshwar, India) as needed for 2 to 3 days. After the corneal epithelium healed, fluorometholone drops were added twice daily for 2 weeks followed by a taper to once daily for 2 weeks. If the patient had a nonhealing epithelial defect, then a bandage contact lens was placed.
Those patients in whom corneal edema developed were prescribed prednisolone acetate 1.0% drops (Allergan) 3 times daily, carboxymethylcellulose 1% (Allergan) 4 times daily, and homatropine 1% (Bell Pharma, Mumbai, India) twice daily. Topical steroids were stopped after 6 weeks of treatment.
Results
Of the 520 charts of patients with progressive keratoconus that were reviewed, 350 consecutive patients received CXL from a referring ophthalmologist. Of these, postoperative corneal edema developed in 10 (10/350; 2.9%). Three patients (3/350; 0.9%) were excluded: 1 because of stromal haze, 1 because of infectious keratitis without corneal edema, and 1 because of corneal melt. No intraoperative complications were noted at the time of CXL treatment. The average age was 22 ± 5 years (range, 16 to 32 years). Patients were followed up for mean of 14 ± 4 months (range, 8 to 22 months). Before surgery, the median logarithm of the minimal angle of resolution (logMAR) best-corrected visual acuity was 0.00 ± 0.08, the median maximum keratometry was 57.4 ± 2.90 diopters, and the mean pachymetry was 472.6 ± 17.5 μm. Preoperative specular microscopy was not performed ( Table ).
| Patient No. | Age (y) | Sex | VA | Max K | CCT | Follow-up (mos) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | 3 Weeks after Surgery | 3 Months after Surgery | 6 Months after Surgery | 12 Months after Surgery | ||||
| 1 | 17 | M | 0.00 | 0.20 | 53.8 | 48.0 | 493 | 621 | 596 | 586 | 565 | 22 |
| 2 a | 21 | F | 0.00 | 0.80 | 51.2 | 50.0 | 482 | 698 | 693 | 682 | 664 | 12 |
| 3 a | 24 | M | 0.00 | 0.20 | 59.8 | 49.3 | 484 | 656 | 645 | 594 | 585∼ | 18 |
| 4 b | 20 | M | 0.20 | 1.00 | 59.4 | 56.8 | 480 | 695 | 685 | 663 | 657 | 8 |
| 5 | 29 | F | 0.00 | 0.50 | 57.9 | 55.4 | 496 | 598 | 587 | 585 | 572 | 10 |
| 6 b | 16 | M | 0.00 | 1.00 | 53.8 | 54.2 | 474 | 687 | 659 | 633 | 585 | 15 |
| 7 | 32 | F | 0.00 | 0.30 | 58.3 | 55.6 | 463 | 620 | 582 | 571 | 569 | 16 |
| 8 | 26 | M | 0.00 | 0.60 | 56.9 | 54.8 | 447 | 678 | 674 | 628 | 590 | 14 |
| 9 | 16 | M | 0.00 | 0.60 | 59.5 | 57.9 | 449 | 634 | 626 | 597 | 575 | 16 |
| 10 b | 22 | M | 0.20 | 0.80 | 56.9 | 54.6 | 458 | 658 | 632 | 609 | 584 | 12 |
a Patients who underwent penetrating keratoplasty after cross-linking.
b Patients offered penetrating keratoplasty after cross-linking, but declined.
In all cases, the onset of corneal edema occurred within the first 24 hours after the procedure, and both the corneal edema and anterior chamber inflammation increased for 2 to 3 weeks. Descemet membrane was not ruptured, nor was intraocular pressure elevated after surgery in any cases. All patients were phakic, and there were no lens opacities after CXL. Additional anterior segment findings in the 10 patients included: marked deep corneal vascularization (2 eyes; 22%), iris atrophy (6 eyes; 67%), pigment dispersion (5 eyes; 56%), corneal epithelial defect present for more than 6 days (3 eyes; 33%), and infectious keratitis (1 eye; 11%; Figures 1 and 2 ). The infectious keratitis occurred in a patient with a persistent corneal epithelial defect.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


