Purpose
To compare the long-term outcomes of peripheral retinal cryoablation to conventional treatment for active pars planitis.
Design
Retrospective, interventional, comparative case series.
Methods
Review at a single institution was conducted to compare the effect of cryotherapy to eyes with pars planitis to those receiving conventional therapy (topical, regionally injected, or oral corticosteroid therapy). Best-corrected visual acuity (VA), complications, resolution of cystoid macular edema (CME), and anterior chamber and vitreous inflammation were assessed.
Results
One hundred thirty-six eyes were treated conventionally, 50 eyes were treated with cryotherapy. Median follow-up was 60.8 months (range 8.1–223.1 months) in the cryotherapy group and 45.0 months (range 3.1–339.0 months) in the controls. There were no significant differences in baseline VA, anterior chamber and vitreous inflammation, presence of CME, and prior use of regional corticosteroid injections. VA improved over time in the cryotherapy group (slope of −0.0018 logMAR units per month; P = .023) but declined in the controls (slope of +0.0011 logMAR units per month; P = .023). Kaplan-Meier survival estimates demonstrated faster times to resolution of anterior chamber cell, vitreous cell, and CME in the cryotherapy-treated eyes. Hazard ratios of remission (adjusted for confounding factors) for vitreous cell and CME for those treated with cryotherapy compared to controls were 4.73 (95% confidence interval 1.63, 13.63; P = .004) and 6.85 (95% confidence interval 1.06, 44.78; P = .044), respectively. No ocular complications were identified in the cryotherapy group.
Conclusions
These data suggest that peripheral retinal cryoablation therapy is an effective treatment for active pars planitis and may be better than conventional regional corticosteroid injections and oral corticosteroid therapy for induction of remission.
Pars planitis is a subset of intermediate uveitis characterized by chronic vitreous inflammation and the accumulation of fibroinflammatory debris over the pars plana, occurring in the absence of any associated infection or systemic disease. Clinically, these collections of inflammatory material resemble yellow-gray or white aggregates visible in the mid- and posterior vitreous and collections of inflammatory debris on the pars plana (particularly inferiorly), known as “snowballs” and “snowbanks,” respectively. The most frequent structural complication of pars planitis is macular edema, and most treatment regimens are directed at controlling macular edema. Other, less common structural complications include traction retinal detachments and vitreous hemorrhage from neovascularization of the snowbank.
Although a subset of patients with pars planitis do not have macular edema or visual impairment and may be observed, the majority of patients need treatment. Conventional treatment regimens typically have used a stepped approach starting with regional corticosteroid injections (either periocular or intravitreal), followed by oral corticosteroids, supplemented with immunosuppression as needed for more difficult or bilateral cases. Regional corticosteroid injections have the potential for elevated intraocular pressure and cataract formation/progression and typically have a duration of effect of 3 months, thereby requiring repetitive injections. Although when used properly, oral corticosteroids and immunosuppression can be administered with minimal to no increase in side effects in adults, in children long-term use of oral corticosteroids is avoided owing to the risk of growth retardation. Furthermore, the chronic nature of the disease often requires long-term therapy; there is a low sustained, drug-free remission rate; and some patients’ uveitis will not be controlled by this approach. Although some clinicians have advocated therapeutic vitrectomy for pars planitis, a review concluded that methodological problems and study confounders resulted in insufficient evidence to support or refute its use. In 1973, Aaberg and associates reported in 23 eyes in 14 patients affected by pars planitis that peripheral retinal ablation directed at the inflammatory exudates overlying the pars plana with transconjunctival cryopexy (cryotherapy) was effective at decreasing vitritis and improving visual acuity. These observations subsequently were supported by data from other small case series; however, these studies evaluated the effect of cryotherapy on relatively few eyes and were limited by a relatively short duration of follow-up.
There are limited data on the long-term effectiveness of peripheral retinal cryoablation therapy in controlling intraocular inflammation, improving visual acuity outcomes, and reducing structural complications of pars planitis. Our retrospective study compared the long-term clinical outcomes of eyes receiving cryotherapy to those receiving conventional therapy for active pars planitis. We sought to determine if cryotherapy resulted in better visual outcomes and faster time to resolution of cystoid macular edema, vitreous, and anterior chamber cell compared to conventional therapy.
Methods
A retrospective, interventional, comparative study of all known patients with active pars planitis treated in the Department of Ophthalmology and Visual Sciences at the University of Iowa from January 1, 1983 (near the time cryotherapy for pars planitis was first used at the University of Iowa) to January 1, 2013 was conducted. The records of patients with ICD-9 diagnosis code 363.21 corresponding to a diagnosis of pars planitis were reviewed for inclusion in this study. Included patients met the following criteria: (1) presence of intraocular inflammation in the vitreous in at least 1 eye; (2) presence of inflammatory vitreous debris with snowbanks on the pars plana of the inflamed eye; and (3) a follow-up ophthalmic evaluation performed at least 3 months after the diagnosis of pars planitis. Exclusion criteria included (1) serologic evidence of an infectious etiology for the ocular inflammation or a known associated systemic disease (eg, sarcoidosis or multiple sclerosis); (2) clinical history or physical examination finding(s) to suggest a diagnosis other than pars planitis (eg, oral lesions in patients with Behçet disease); (3) intermediate uveitis without evidence of snowbanks; (4) isolated anterior or posterior uveitis; and (5) significant diabetic retinopathy, macula-off retinal detachment, uncontrolled glaucoma, or a disease other than pars planitis that could account for a loss of visual acuity. Only de-identified data were used in the analyses. Institutional Review Board approval at the University of Iowa was obtained for this project, which adhered to the principles of the Declaration of Helsinki.
Data were extracted from review of patient charts at the time of pars planitis diagnosis (the “baseline” visit) and at consecutive follow-up visits. Follow-up visits were grouped as sequential 3-month “contiguous visit windows” extending until the last follow-up visit (eg, the 3-month follow-up window extended from 1.5 to 4.5 months post-baseline, the 6-month follow-up visit window from 4.5 to 7.5 months post-baseline, etc). Data collected at presentation, baseline, and follow-up visits included (1) best-corrected Snellen visual acuity; (2) presence or absence of cystoid macular edema identified by stereoscopic funduscopic examination and/or fluorescein angiography, which was confirmed by optical coherence tomography imaging when this modality became available (2004); (3) grading of anterior chamber cell; (4) grading of vitreous chamber cell; (5) lenticular status (phakic, aphakic, pseudophakic); (6) use of topical corticosteroid medications; (7) use of oral corticosteroid medications; (8) use of periocular corticosteroid injections within the previous 120 days; (9) treatment of glaucoma with topical medication; (10) interval glaucoma surgery; (11) interval cataract surgery; and (12) presence of retinal detachment. Also noted in treated eyes was the date of the first cryotherapy and the total number of cryotherapy treatments per eye.
Visual acuity data were converted to logMAR (logarithm of the minimal angle of resolution) values (logMAR = log [1/Snellen visual acuity]) to allow for statistical analysis. The following logMAR values were assigned: for hand motion, 3.3 logMAR; light perception, 4.3 logMAR; and no light perception, 5.3 logMAR. Each difference of +0.3 logMAR between the baseline and follow-up visual acuity corresponds to a loss of 3 lines on an Early Treatment Diabetic Retinopathy Study (ETDRS) eye chart and a doubling of the visual angle.
Much of the grading of anterior chamber cell and vitreous chamber cell was performed prior to publication of the Standardization of Uveitis Nomenclature’s (SUN) publication of their standardized grading schema. However, the grading used appears to correspond reasonably well with the SUN schema. The early grading used a 1 × 1 mm beam on the brightest illumination on slit-lamp biomicroscopy and had the following grades: 0 for no cells, 0.5+ for 1–2 cells, 1+ for 5–10 cells, 2+ for 10–20 cells, 3+ for 20–30 cells, and 4+ for over 30 cells. Anterior chamber and vitreous inflammatory activity outcomes were dichotomized based on a threshold of anterior chamber cell or vitreous chamber cell ranking less than or equal to 0.5+, corresponding to “trace” inflammatory activity or less. The proportion of patients with anterior chamber cell or vitreous cell ranking less than or equal to 0.5+ at baseline and the rate at which patients’ anterior chamber and vitreous inflammation fell below this threshold was compared between eyes treated with cryotherapy and eyes treated with conventional therapy alone.
Cryoablation Procedure and Conventional Therapy
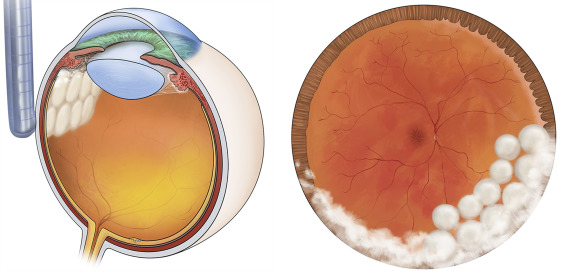
With visualization using the indirect ophthalmoscope and condensing lens, single freeze-thaw, confluent, but not overlapping applications of cryotherapy were applied to all areas of snowbanking along involved areas of the pars plana ( Figure 1 , Left). Procedures were performed by 1 of 2 surgeons (E.H.S. or J.C.F.). A single row of cryotherapy was also applied just posterior to the most posterior aspect of snowbanking ( Figure 1 , Right). Depending on the amount of snowbanking, the average eye may receive between 10 and 20 spots of cryotherapy. If the snowbanking involved more than 6 clock hours of the periphery, treatment was planned in 2 sessions because of the concern that more extensive cryopexy at a single session could cause exacerbation of the inflammation and/or peripheral retinal traction. A second session of cryotherapy was also performed if the inflammation remained active. All patients received preprocedure topical anesthesia with proparacaine eye drops and, if the cryotherapy was performed in the clinic, subconjunctival 2% lidocaine without epinephrine; those intolerant of this approach were given a peribulbar block with 2% lidocaine without epinephrine. Children under the age of 16 years or those with substantial anxiety or discomfort were brought to the operating room for monitored anesthesia care or laryngeal mask anesthesia for the procedure. No postoperative antibiotic drops were given to patients. To blunt any inflammatory response and the potential for retinal detachment from cryotherapy, some patients not already on oral prednisone received either (1) a posterior superior sub-Tenon injection of 20 mg triamcinolone acetonide or intravitreal 2 mg triamcinolone acetonide injection at the time of cryotherapy (n = 21) or (2) oral prednisone at a dose of 20–60 mg daily for 3 days prior to treatment, then a rapid taper and discontinuation over 9 days after cryotherapy (n = 6).
Patients receiving conventional therapy (ie, controls) received either topical prednisolone acetate 1% eye drops or a posterior superior sub-Tenon or an intravitreal triamcinolone acetonide injection for unilateral active pars planitis. Oral prednisone was used for recalcitrant unilateral cases, eyes with a history of a corticosteroid-related intraocular pressure rise, or bilateral active disease; patients who could not tolerate prednisone or had recalcitrant disease despite prednisone 80 mg daily were started on corticosteroid-sparing immunomodulatory therapy. Relatively few eyes were treated with pars plana vitrectomy with or without adjunctive cryotherapy; any eyes receiving cryotherapy were placed in the cryotherapy group. Some eyes with bilateral active disease received cryotherapy in only 1 eye; in these instances the eye with more severe disease was always selected for cryotherapy.
Statistical Analysis
Kaplan-Meier curves and random-effects Cox proportional hazards models were fit for time-to-event data, such as resolution of macular edema, vitreous cell, and anterior chamber cell. Visual acuity (logMAR after conversion from Snellen) trajectories were obtained using linear model with random effects (ie, mixed model). Resolution was defined as going from a vitreous (or anterior) chamber cell rating greater than 0.5+ at baseline (ie, time of cryotherapy or time or presentation in the control group) to the first occurrence of vitreous (or anterior) cell rating less than 0.5+ at least 3 months after baseline, with additional qualifiers of having no periocular or intravitreal corticosteroid injections within the previous 120 days and no oral corticosteroids or immunosuppressive agents. The 120-day time lag was used to account for the duration of the effect of regional corticosteroid injections in both groups. Baseline for the controls was defined as the time of presentation; for the cryotherapy group it was the date the treatment was performed or most recent visit before cryotherapy. Time-varying covariate analysis was performed to account for confounding factors found between the groups at baseline and during follow-up, including bilaterality, vitrectomy, and regional corticosteroid injections given after baseline.
Results
Of the charts reviewed for inclusion in this study, 58 patients were excluded because they did not meet the diagnostic criteria for pars planitis and 3 patients were excluded owing to follow-up of less than 3 months. The study population consists of 186 eyes (136 control eyes; 50 cryotherapy eyes) from 95 patients (69 control patients, 6 cryotherapy patients with unilateral pars planitis, and 20 patients with bilateral uveitis where 1 eye was treated with cryotherapy and the second eye was in the control group). Characteristics of the study population are shown in the Table . Cryotherapy-treated patients were followed for a median of 60.8 months (range 8.1–223.1 months) and controls were followed for a median of 45.0 months (range 3.1–339.0 months). Ten eyes in the cryotherapy group sustained more than 1 treatment. The 2 groups were relatively well balanced at baseline with no significant differences between the groups in baseline visual acuity, anterior chamber and vitreous inflammation, presence of macular edema, and prior use of regional corticosteroid injections. There were significant differences in the ages of the 2 groups, with the cryotherapy group being somewhat younger (median 17.4 years vs 23.0 years) and in the higher use of oral corticosteroids in the cryotherapy group at baseline (28.2% vs 2.9%, P = .001).
| Characteristic | Cryotherapy Group | Control Group | P Value |
|---|---|---|---|
| Number of patients a | 40 | 86 | |
| Number of eyes | 50 | 136 | |
| Median age (y) | 17.4 | 23.0 | <.001 |
| Age range | 12–70 | 12–74 | |
| Sex (%) | |||
| Men | 55 | 46 | .37 |
| Women | 45 | 54 | |
| Race/ethnicity (%) | |||
| White, non-Hispanic | 95.0 | 98.8 | .19 |
| African-American | 2.5 | 1.2 | .59 |
| Asian | 2.5 | 0 | .14 |
| Bilateral uveitis (%) | 92.5 | 76.7 | .03 |
| Treatment at baseline | |||
| % who received regional corticosteroids within 3 months of baseline | 0 | 1.5 | .44 |
| Current prednisone use (%) | 28.2 | 2.9 | .001 |
| Immunosuppression (%) | 0 | 0 | |
| Ocular characteristics | |||
| Presenting visual acuity | |||
| Median logMAR | 0.4 | 0.3 | .23 |
| Range, logMAR | −0.12 to 3.3 | −0.12 to 3.3 | |
| Snellen equivalent | 20/50 | 20/40 | |
| Anterior chamber median grade cell | 0.5 | 0.5 | .68 |
| Range | 0–3 | 0–3 | |
| Vitreous cell median grade | 2 | 2 | .20 |
| Range | 0–3 | 0–3 | |
| Lens status (%) | |||
| Phakic | 100.0 | 99.3 | .54 |
| Pseudophakic | 0 | 0.07 | .56 |
| Macular edema (%) | 47.9 | 45.2 | .71 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


