Purpose
To compare the performance of individuals with deficient stereoacuity with that of individuals with normal stereoacuity on a microsurgical task using the VRMagic EYESi Ophthalmosurgical Simulator (VRmagic Holding AG).
Design
Prospective, experimental study at a single institution.
Methods
Subjects with abnormal stereoacuity and controls with normal stereoacuity completed a total of 4 attempts on 2 standardized microsurgical tasks on the EYESi Simulator. Performance was quantified using a 60-point scale, and scores were compared using the Wilcoxon rank-sum test with a significance level of .05 assumed for all tests.
Results
Twenty-one subjects with deficient or absent stereoacuity and 21 control subjects with normal stereoacuity were included. The mean age of both groups was 31.5 years (range, 10 to 64 years). Twenty-nine (69%) participants were male. The 2 groups did not differ in age or gender. For each of the 4 module attempts, the Wilcoxon rank-sum test showed significantly better performance of individuals in the control group compared with the study group ( P < .001). Additional attempts did not result in improved performance by the study group compared with the control group. No significant associations were observed between performance scores and age or gender.
Conclusions
This study compared the performance of patients with deficient stereoacuity with that of those with normal stereoacuity in microsurgical tasks. Individuals with normal stereoacuity performed better than those with deficient stereoacuity in a simulated microsurgical task. A larger and more complex study may be necessary to validate the findings of the present investigations.
Depth perception is the visual ability to perceive the world in 3 dimensions. It relies on cues from both monocular and binocular stimulation of the retina and visual cortex. Stereopsis is a particularly refined form of binocular fusion resulting from neural processing of the relative horizontal binocular disparities between monocular retinal projections. Stereopsis can be lost as a result of a deficit in binocular vision. Examples include individuals who have lost the use of one eye secondary to trauma or disease, as well as those individuals with monofixation syndrome, a form of sensory adaptation secondary to subnormal binocular vision. Monofixation syndrome can be the result of small-angle strabismus, anisometropia, or occlusion amblyopia, or it may occur as a primary defect in central binocular vision. Patients with monofixation syndrome have a unilateral central suppression scotoma and maintain peripheral fusion under binocular viewing conditions, with a resultant deficit in stereopsis. The prevalence of monofixation syndrome in the general population in the United States is approximately 1%.
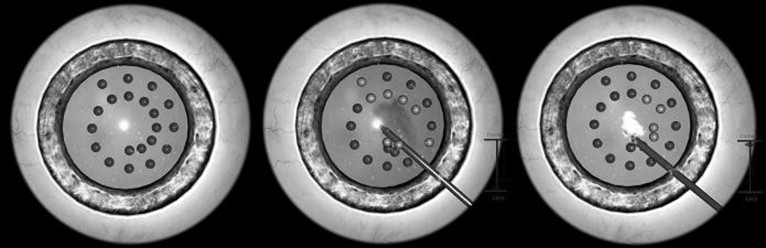
The VRMagic EYESi Ophthalmosurgical Simulator (VRmagic Holding AG, Mannheim, Germany) is a device that was designed for intraocular microsurgical training ( Figure 1 ). The premise for its development was based on flight simulators used to train pilots for civil aviation. During simulated surgery, the participant manipulates handheld instruments that are inserted into an artificial eye. The motion and orientation of the instruments are interpreted by sensors and are transmitted to a computer, which then renders the virtual operation scenario into the EYESi microscope. Although the simulator software adapts to individual actions of each participant, each module is highly reproducible, providing identical tasks and objective measures of performance.

It is unclear if individuals with deficient stereopsis perform similar to, or worse than, individuals with normal stereopsis on manual tasks that theoretically necessitate refined binocular function. Assuming that certain, if not all, modules require good depth perception and stereoacuity to perform a given surgical task, we hypothesized that individuals with normal stereopsis would perform better than those with either deficient or absent stereoacuity. We set out to test this hypothesis using the VRMagic EYESi Ophthalmosurgical Simulator.
Methods
A prospective experimental study was conducted at the Cole Eye Institute in Cleveland, Ohio. Inclusion criteria for the study group included deficient stereoacuity (80 seconds of arc or less on the Titmus stereotest; Stereo Optical Company, Chicago, Illinois, USA) and binocular best-corrected Snellen visual acuity of 20/40 or better. Inclusion criteria for the control group included normal stereoacuity (60 seconds of arc or more on the Titmus stereotest), best-corrected Snellen visual acuity of 20/40 or better in each eye, and otherwise normal eye examinations. Additional inclusion criteria for both groups included the ability to sit at the simulator device and age between 10 and 75 years. Exclusion criteria for both groups included ongoing therapy for amblyopia, recent intraocular or periocular surgery (within the preceding 60 days), prior microsurgical experience, and the presence of mental deficiency or other physical or mental reason for impaired performance.
Subjects completed two standardized, highly reproducible anterior segment modules on the VRMagic EYESi Ophthalmosurgical Simulator. During these tasks, subjects manipulated a handheld probe (controlled by the subject’s dominant hand) with its tip inserted into the anterior segment of the artificial eye. The goals of the assigned tasks were: (1) to touch the probe tip to several target spheres dispersed at various depths in the anterior chamber, (2) to maintain efficient control of the eye and probe, and (3) to avoid touching the probe tip to the iris, lens, and cornea ( Figure 2 ). Subjects performed 3 consecutive attempts on the first difficulty level module, followed by 1 attempt on the third difficulty level module. This final module was graded as a higher difficulty level because of variation in target size and depth of location within the anterior chamber. Subjects were given up to 4 minutes to attempt the completion of each module.
Each subject’s performance was quantified using a predetermined scale totaling 60 points. Scores were based on the subject’s ability to touch each target site in the allotted time; ability to avoid the lens, iris, and cornea; speed and efficiency of movements; ability to maintain zonular stability; and ability to maintain the probe tip and target sites in focus.
Scores were compared between the study and control groups using the Wilcoxon rank-sum test. Scores were compared additionally between age groups and genders using Wilcoxon rank-sum tests, Pearson chi-square tests, and Spearman correlations. For the first module, which was repeated for a total of 3 attempts, the interval improvement of the performance scores between consecutive attempts was compared, also using Wilcoxon rank-sum tests, to evaluate each group’s ability to improve performance with practice. All statistical analyses were conducted using SAS software version 9.2 (SAS Institute, Cary, North Carolina, USA). A significance level of .05 was assumed for all comparisons.
Results
A total of 42 patients were recruited into the study: 21 patients with deficient or absent stereoacuity and 21 control patients with normal stereoacuity. Results are given in Table 1 . The mean age of the 42 subjects was 31.5 years (range, 10 to 64 years). The median and mean ages were 30 and 32 years, respectively, in the study group, and 29 and 31 years, respectively, in the control group. Of the 42 subjects, 29 (69%) were male, 15 within the study group and 14 within the control group. Based on these demographics, there was no difference between the study and control groups in age and gender ( P = .92, Wilcoxon rank-sum tests for age; P = .74, Pearson chi-square tests for gender).
| Patient No. | Age (yrs) | Sex | Binocular BCVA | Stereoacuity a (Seconds of Arc) | Cause of Deficient Stereoacuity, If Present | EYESi Simulator Scores | |||
|---|---|---|---|---|---|---|---|---|---|
| Level 1 | Level 3 | ||||||||
| First Attempt | Second Attempt | Third Attempt | |||||||
| Study group | |||||||||
| 1 | 10 | M | 20/20 | 200 | Accommodative Esotropia | 0 | 0 | 0 | 0 |
| 2 | 12 | F | 20/30 | 3000 | Esotropia | 0 | 0 | 0 | 0 |
| 3 | 49 | F | 20/20 | absent | Duane syndrome with esotropia | 0 | 0 | 0 | 0 |
| 4 | 64 | M | 20/20 | 100 | Exotropia | 0 | 33 | 33 | 0 |
| 5 | 15 | M | 20/15 | 400 | Congenital SO palsy with hypertropia | 0 | 0 | 0 | 0 |
| 6 | 37 | F | 20/30 | absent | Anisometropic amblyopia | 0 | 24 | 2 | 0 |
| 7 | 17 | M | 20/20 | absent | Exotropia with DVD | 0 | 0 | 0 | 0 |
| 8 | 55 | M | 20/25 | 3000 | Exotropia | 0 | 0 | 6 | 0 |
| 9 | 30 | M | 20/15 | absent | Esotropia | 0 | 0 | 0 | 0 |
| 10 | 12 | M | 20/20 | absent | Anisometropic amblyopia | 0 | 37 | 31 | 0 |
| 11 | 15 | M | 20/25 | absent | Esotropia | 0 | 0 | 8 | 0 |
| 12 | 21 | M | 20/40 | 3000 | Nystagmus | 9 | 34 | 34 | 0 |
| 13 | 14 | F | 20/20 | absent | Esotropia | 31 | 11 | 8 | 0 |
| 14 | 39 | M | 20/20 | 200 | Anisometropic amblyopia | 12 | 33 | 36 | 0 |
| 15 | 40 | M | 20/20 | absent | Exotropia | 27 | 0 | 28 | 0 |
| 16 | 14 | M | 20/20 | absent | NLP vision in 1 eye secondary to total RD | 29 | 39 | 46 | 0 |
| 17 | 30 | M | 20/20 | absent | Exotropia | 0 | 0 | 0 | 0 |
| 18 | 59 | M | 20/20 | absent | Anisometropic amblyopia | 0 | 0 | 0 | 0 |
| 19 | 61 | F | 20/20 | absent | Anisometropic amblyopia | 0 | 17 | 38 | 0 |
| 20 | 57 | F | 20/30 | absent | Anisometropic amblyopia | 31 | 36 | 35 | 8 |
| 21 | 20 | M | 20/25 | 3000 | Esotropia | 0 | 0 | 4 | 2 |
| Control group | |||||||||
| 22 | 29 | M | 20/20 | 40 | 33 | 32 | 33 | 8 | |
| 23 | 32 | M | 20/20 | 60 | 58 | 57 | 55 | 28 | |
| 24 | 10 | M | 20/20 | 40 | 16 | 23 | 22 | 0 | |
| 25 | 14 | M | 20/20 | 40 | 0 | 0 | 0 | 19 | |
| 26 | 12 | M | 20/20 | 40 | 0 | 0 | 0 | 0 | |
| 27 | 55 | F | 20/20 | 40 | 29 | 23 | 35 | 8 | |
| 28 | 28 | M | 20/30 | 40 | 57 | 60 | 60 | 57 | |
| 29 | 20 | M | 20/20 | 40 | 36 | 33 | 47 | 52 | |
| 30 | 22 | F | 20/15 | 40 | 56 | 54 | 32 | 8 | |
| 31 | 30 | F | 20/20 | 40 | 32 | 59 | 55 | 35 | |
| 32 | 30 | F | 20/20 | 40 | 39 | 39 | 59 | 31 | |
| 33 | 62 | M | 20/20 | 40 | 0 | 0 | 0 | 0 | |
| 34 | 30 | M | 20/25 | 40 | 31 | 36 | 37 | 0 | |
| 35 | 21 | F | 20/20 | 60 | 19 | 58 | 53 | 47 | |
| 36 | 31 | F | 20/20 | 40 | 35 | 59 | 53 | 54 | |
| 37 | 29 | M | 20/25 | 40 | 58 | 59 | 60 | 59 | |
| 38 | 23 | F | 20/20 | 60 | 33 | 34 | 38 | 32 | |
| 39 | 27 | M | 20/20 | 40 | 35 | 49 | 59 | 39 | |
| 40 | 45 | M | 20/20 | 50 | 51 | 39 | 59 | 57 | |
| 41 | 56 | M | 20/20 | 40 | 37 | 60 | 59 | 32 | |
| 42 | 47 | M | 20/20 | 40 | 36 | 49 | 51 | 0 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


