This article reviews current knowledge of the science of pediatric tonsillectomy—developmental anatomy of the tonsil, physiology of the operation, and wound healing after surgery. It outlines indication for surgery and best practices for intraoperative and postoperative care as described in the American Academy of Otolaryngology—Head and Neck Surgery Foundation clinical practice guideline: Tonsillectomy in Children. Finally, it discusses areas of uncertainty in the field and opportunity for future improvement.
Key points
- •
Tonsillectomy decreases the frequency of severe recurrent sore throats in children who meet the “Paradise criteria.”
- •
Adenotonsillectomy improves symptoms of sleep disordered breathing in children with adenotonsillar hypertrophy.
- •
Polysomnography is a useful adjunct in selecting children for surgery, especially when the diagnosis is in doubt or risks of surgery are increased because of young age or comorbid conditions.
- •
Obese children with sleep disordered breathing may not be cured by surgery.
- •
Ibuprofen is safe after tonsillectomy and provides good pain relief with fewer side effects than narcotics.
| AAO-HSN | American Academy of Otolaryngology – Head and Neck Surgery Foundation |
| IL | Interleukin |
| PANDAS | Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections |
Introduction
The tonsillectomy operation has changed in recent years. More children are operated on for sleep disordered breathing and fewer for recurrent pharyngitis. New instruments now permit less invasive surgery. Systematic reviews by the Cochrane Collaboration and others have helped to define best practices for preoperative assessment and postoperative care.
Approximate 100 million tonsillectomies have been performed worldwide in the century since the procedure was popularized. Pediatric tonsillectomy with or without adenoidectomy is an effective operation for obstructive sleep apnea and sleep disorder breathing. It can decrease the incidence of sore throat in children who have frequent throat infections and may be effective for children who suffer from peritonsillar cellulitis or abscess, pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS), “chronic” tonsillitis, febrile seizures, halitosis, dental malocclusion, cryptic tonsils, or hemorrhagic tonsillitis. It has a role in the prevention of recurrences of rheumatic fever, and in controlling chronic pharyngeal carriage of group A beta-hemolytic streptococci. Yet despite a century of experience with this operation, tonsillectomy remains a traumatic experience for children and their families. In the best of hands, tonsillectomy has a 1% to 5% risk of immediate or delayed hemorrhage and a 1:35,000 death rate. The surgery produces separation anxiety, postoperative edema, dysphagia, weight loss, and night terrors. Nausea and vomiting remain common despite pharmacologic advances and everyone suffers from pain. Even when well-treated with opioid and nonopioid analgesics, most children still rate their pain as moderate to severe.
This article reviews current knowledge of the science of pediatric tonsillectomy—developmental anatomy of the tonsil, physiology of the operation, and wound healing after surgery. It outlines indications for surgery and best practices for intraoperative and postoperative care as described in the American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HSN) clinical practice guideline: Tonsillectomy in Children. Finally, it discusses areas of uncertainty in the field and opportunity for future improvement.
Introduction
The tonsillectomy operation has changed in recent years. More children are operated on for sleep disordered breathing and fewer for recurrent pharyngitis. New instruments now permit less invasive surgery. Systematic reviews by the Cochrane Collaboration and others have helped to define best practices for preoperative assessment and postoperative care.
Approximate 100 million tonsillectomies have been performed worldwide in the century since the procedure was popularized. Pediatric tonsillectomy with or without adenoidectomy is an effective operation for obstructive sleep apnea and sleep disorder breathing. It can decrease the incidence of sore throat in children who have frequent throat infections and may be effective for children who suffer from peritonsillar cellulitis or abscess, pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS), “chronic” tonsillitis, febrile seizures, halitosis, dental malocclusion, cryptic tonsils, or hemorrhagic tonsillitis. It has a role in the prevention of recurrences of rheumatic fever, and in controlling chronic pharyngeal carriage of group A beta-hemolytic streptococci. Yet despite a century of experience with this operation, tonsillectomy remains a traumatic experience for children and their families. In the best of hands, tonsillectomy has a 1% to 5% risk of immediate or delayed hemorrhage and a 1:35,000 death rate. The surgery produces separation anxiety, postoperative edema, dysphagia, weight loss, and night terrors. Nausea and vomiting remain common despite pharmacologic advances and everyone suffers from pain. Even when well-treated with opioid and nonopioid analgesics, most children still rate their pain as moderate to severe.
This article reviews current knowledge of the science of pediatric tonsillectomy—developmental anatomy of the tonsil, physiology of the operation, and wound healing after surgery. It outlines indications for surgery and best practices for intraoperative and postoperative care as described in the American Academy of Otolaryngology–Head and Neck Surgery Foundation (AAO-HSN) clinical practice guideline: Tonsillectomy in Children. Finally, it discusses areas of uncertainty in the field and opportunity for future improvement.
Developmental anatomy
Developmental anatomy describes when the tonsil becomes immunologically active, how its structure changes, when it enlarges, and when it involutes. An appreciation of the fetal development of the tonsil and the changes it undergoes in the first decade of life can aid in surgical decision making ( Table 1 ).
| Observation | Implications for Intracapsular Tonsillectomy |
|---|---|
| The tonsil epithelium arises before the lymphoid component. Lymphoid cells infiltrate the lamina propria then proliferate. | The crypt epithelium runs full thickness through the tonsil; thus, superficial treatment of the crypts is unlikely to be effective. |
| The tonsil is arranged in lymphoepithelial fronds. Lymphoid elements are arranged around a fibrovascular core in each frond. The fronds are surrounded by crypt epithelium. | Crypt epithelium and lymphoid elements are intimately associated and cannot be treated independently. |
| Germinal center activation occurs after birth when the immune system is exposed to stimulating antigens. | The tonsil is an immunologically active structure. It is insignificant in mass in most infants. |
| Rapid germinal center proliferation is the most conspicuous event of the first decade of tonsil development and accounts for most of tonsillar enlargement. | Surgery that leaves significant amounts of residual lymphoid tissue may lead to recurrent hyperplasia. |
| The tonsil has no core. | It is not possible to perform a tonsil “core” biopsy without contamination by epithelial elements. |
| The concept of bacterial sequestration in the tonsil “core” is not valid. | |
| The tonsil capsule is contiguous with the trabeculae and frond fibrovascular cores. | There is no natural surgical plane between the tonsil parenchyma and the capsule. |
| The tonsil capsule surrounds the tonsil except on the medial crypt surface. | Powered intracapsular tonsillectomy, proceeding outward from the crypt area, can remove all of the lymphoid and epithelial elements. The appearance of thick trabeculae signals the approach of the capsule. |
| Marginal incisions around the crypt area are made in intracapsular tonsillectomy with bipolar electrosurgical scissors or plasma excision. Such incisions will encompass all tonsil epithelial elements. | |
| The tonsil expands, rather than invades, surrounding structures as it grows. | Removal of the parenchyma of the tonsil allows collapse of expanded normal tissues, minimize wound surface area. |
| The tonsillar pillars and plicae do not contain bulky lymphoid elements or crypt epithelium. | The tonsil pillars and all plica mucosa can be preserved for healing without compromising surgical goals. |
| Involution of lymphoid elements is characteristic of the second decade of life. | More conservative tonsil resection (or avoidance of surgery) may be preferable in older children. |
| Prominent fibrosis of the capsule and trabeculae is typical of the third decade and beyond. | Techniques applicable to young children may work less well in the fibrotic tonsils of adults. |
Intrauterine Development
The epithelium that covers the tonsil’s medial surface and lines the tonsillar crypts arises from the second branchial (pharyngeal) pouch. The outer edges of this outpouching go on to form the faucial arches and mucosa plicae. In the embryo, solid epithelial cores form in the lateral walls of each pouch and grow outward into the surrounding mesenchymal tissue. These epithelial cores branch and subsequently canalize. The branches ultimately become the primary and secondary tonsillar crypts ( Fig. 1 A). Transmission electron microscopy has demonstrated that the mature crypt epithelium is porous and allows the protrusion of lymphocytes that mediate the immune response.
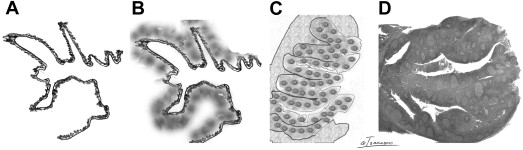
The mucosa of the tonsillar fossa is similar in microscopic structure to the lining of the oropharynx. Its surface is nonkeratinizing squamous epithelium with an underlying lamina propria. The pharyngeal tonsils are a part of the mucosa-associated lymphatic tissue system and develop their monocellular populations in a fashion much like the Peyer’s patches in the gut. Around the 16th week postconception, the lamina propria is invaded by wandering lymphocytes and lymphoid stem cells of bone marrow origin (see Fig. 1 B). The lymphatic tissue surrounding the crypts becomes organized into a cellular architecture resembling that of lymph nodes and includes B-cell follicles, primary germinal centers, and extrafollicular T-cell areas (see Fig. 1 C). Unlike lymph nodes, tonsils lack afferent lymphatics. Instead, the epithelium that lines the crypts contains dendritic cells that can transport exogenous antigens to extrafollicular T-cell areas and to B-cell follicles. The intimate relationship between the crypt epithelium and lymphoid component continues through life.
Immune stimulation begins shortly after birth in response to exogenous antigens. Terminal differentiation of effector B-cells to extrafollicular plasma cells can be seen first at approximately 2 weeks postnatally. This results in the development of secondary follicles with active germinal centers. The proliferation of these germinal centers is the outstanding event of the first decade of life and accounts for the rapid growth of the tonsil in the young child (see Fig. 1 D). This hyperplasia expands the tonsil at the expense of the surrounding soft tissues and the oropharyngeal space. The tonsils behave like other benign mass lesions, expanding rather than invading the surrounding tissues.
The tonsillar capsule arises from deep layers of the lamina propria. The deepest layers are pushed aside by the enlarging lymphoid component of the tonsil and condense to form a thin, compact membrane or capsule. The capsule surrounds the tonsil mass on all sides, except on its medal, cryptic surface. The more superficial fibers coalesce into trabeculae between the branching crypts. The tonsillar capsule is continuous with these trabeculae. Thus, there is no natural surgical plane between the tonsil’s parenchyma and its capsule.
Unlike a lymph node, the tonsil is not a mass of lymphoid tissue with a central core and surrounding capsule. Rather, the tonsil parenchyma is a series of densely packed fingerlike fronds. Each frond is based on a fibrovascular core, surrounded by a layer of lymphoid tissue and covered by crypt epithelium. These fronds extend from the capsule to the medial cryptic surface ( Fig. 2 A). The crypt epithelium runs full thickness through the tonsil and lymphoid tissue and is present throughout the tonsil parenchyma.
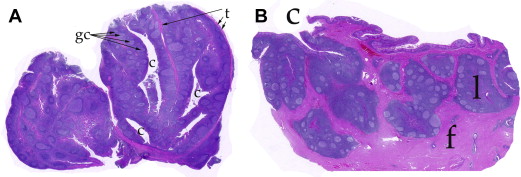
In the second decade of life, the B-cell component of the tonsil begins to involute. Germinal centers become smaller and there is a proliferation of fibrous tissue in the trabeculae and capsule. The tonsil decreases in mass and regresses, disappearing behind the anterior tonsillar pillar, much as it appeared at birth. By the seventh decade, fibrous connective tissue surrounds the lymphoid fronds making the outline of the tonsil less distinct (see Fig. 2 B). Fatty degeneration begins at about 25 years of age and progresses with age.
Tonsillectomy healing
Most of the complications and all of the misery associated with pediatric tonsillectomy come from the injury of surgery and the inflammatory process of second intention healing resulting from an open pharyngeal wound. Although there is progressive improvement from the first day after surgery, pain does not resolve and the risk of bleeding remains until the tonsillar fossae are fully healed at about 2 weeks after surgery. There has been much research into the mechanism of cutaneous wound healing. Healing in the oral cavity is less well studied. Oral mucosal wounds proceed through the same healing stages as seen in the skin, including hemostasis, inflammation, proliferation, and remodeling of the collagen matrix. Oral mucosal healing is more rapid than skin repair and less likely to produce scar.
Several animal studies have focused on the effects of different cutting instruments (lasers, ultrasound, electrosurgical devices, etc) on oral wound healing. Most show that cold steel incision produces the lowest level of collateral tissue damage and leads to the most rapid healing and ultimate tensile strength. Ultrasound, bipolar and monopolar electrosurgery, and carbon dioxide laser (in that order) cause greater injury to surrounding tissues. Such injury results in delayed epithelialization. In a dog tonsil model, microdebrider tonsillectomy resulted in less inflammation and more rapid healing than monopolar electrosurgery.
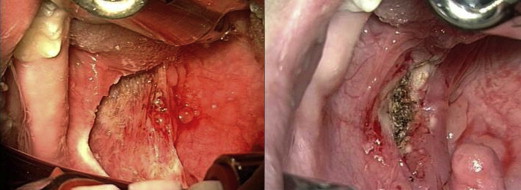
Serial photography of the healing human tonsillar fossa suggests that mucosal injury and healing follows the pattern described in animal experiments ( Fig. 3 ). In human oral wounds, as in the porcine model, polymorphonuclear infiltrates appear quickly. Inflammation is greatest on days 3 through 7, resolving by day 14. Granulation tissue (stroma) forms in the pig cheek defect and is gradually covered by advancing epithelium, as demonstrated in serial human photographs.

Studies of pharyngeal wounding and healing help to explain posttonsillectomy complications, including edema, pain, and hemorrhage. Thermal spread to the tonsillar fossa prevents bleeding by thrombosing blood vessels, but also damages lymphatics at the base of the uvula, producing annoying edema and occasional airway obstruction.
The same inflammatory mediators responsible for stimulating the monocellular influx that clears necrotic wound debris cause injury-associated pain. In a mouse incisional model, increasing postoperative pain was strongly correlated with neutrophil infiltration. Skin samples harvested from these mice show enhanced levels of 5 cytokines: interleukin (IL)-1β, IL-6, tumor necrosis factor alpha, granulocyte colony stimulating factor, and keratinocyte-derived cytokine. After tonsillectomy, analog pain scores decrease linearly from postoperative days 1 through 10. This progression is often interrupted by a ‘bump’ in pain on days 3 through 5, coincident with maximum inflammation and fibrin clot accumulation.
Capillary development in the stoma is greatest at the end of the first postoperative week. This stomal development precedes epithelial ingrowth. With separation of the fibrin clot, capillaries in the vascular stoma are exposed and vulnerable to minor trauma and bleeding. Involution of the vascular stoma (presumably from decreasing levels of vascular endothelial growth factor and cellular apoptosis) coincides with the decreasing risk of secondary hemorrhage in the second week after surgery.
Clinical decision making
Indications
Tonsillectomy, when performed for the right reasons, can:
- •
Decrease upper airway resistance;
- •
Ameliorate or cure obstructive sleep apnea and sleep disordered breathing;
- •
Decrease the incidence of recurrent pharyngitis; and
- •
Improve child health status and quality of life.
Debate rages about what constitutes the “right reasons.” For each child, the potential benefits of tonsillectomy (usually in combination with adenoidectomy) must be weighed against its substantial discomforts and occasional, but real risks.
Adenotonsillar hypertrophy is most pronounced between ages of 3 and 6 years. Tonsils involute in most children after age 8. This sequence accounts for the appearance and natural resolution of snoring and sleep disordered breathing in many children.
Obstructive sleep apnea
There is little doubt that, for children with true obstructive sleep apnea secondary to adenotonsillar enlargement, the negative aspects of surgery are far outweighed by its benefits to health and function. As the severity of the sleep disorder breathing spectrum decreases, the risk–benefit balance shifts. Most pediatric otolaryngologists would not recommend an adenotonsillectomy for a well child troubled only by snoring. By the same token, the child with suspected sleep disordered breathing who also suffers from growth retardation, poor school performance, enuresis, or certain behavioral problems may derive greater benefit from surgery. When uncertainty exists, formal polysomnography can help to quantitate the severity of disease and correlate sleep disruption with symptoms.
Recurrent severe sore throat
Similarly, one must weigh the pros and cons of tonsillectomy versus continued medical management for recurrent sore throats. It is clear that a child undergoing tonsillectomy for frequent severe sore throats will experience fewer sore throats in years to come. It is less clear that the tonsillectomy is the reason for the improvement. For most children, recurrent severe sore throats (characterized by temperature >38.3°C, cervical adenopathy, tonsillar exudate, or positive test for group A beta-hemolytic streptococci) resolve spontaneously within a few years. In a prospective, randomized trial of adenotonsillectomy for severe recurrent sore throats (7 episodes in a year, or 5 in 2 consecutive years, or 3 in 3 consecutive years—also known as “the Paradise criteria”) children derived benefit from surgery for at least 2 years compared with nonoperative controls. In a second, similar trial of moderately affected children (number of episodes, severity or documentation relaxed), surgery slightly decreased the frequency of sore throats compared with controls. The subsequent number of sore throats was so low in both arms as to mute the clinical impact of tonsillectomy. There is likely a subgroup of children with recurrent sore throats who do not improve over time and who might receive greater benefit from surgery. Unfortunately, there is no way to distinguish such patients in advance.
Other relative indications for tonsillectomy include:
- •
Peritonsillar cellulitis or abscess;
- •
PANDAS;
- •
“Chronic” tonsillitis;
- •
Febrile seizures;
- •
Halitosis;
- •
Dental malocclusion;
- •
Cryptic tonsils;
- •
Hemorrhagic tonsillitis;
- •
Prevention of recurrences of rheumatic fever; and
- •
Chronic pharyngeal carriage of group A beta-hemolytic streptococci.
The role of tonsillectomy in the management of these disorders has not undergone rigorous scientific study.
Procedure
It is likely many more tonsillectomies would be performed were it not such a morbid procedure. To reach the oropharynx and overcome strong protective reflexes requires deep general anesthesia in nearly all children. Such anesthetics often lead to transient postoperative disorientation, nausea, and vomiting. Even in the best of hands, classic tonsillectomy is complicated by immediate (0.2%–2%) and delayed (1%–5%) hemorrhage. Incomplete ligation or coagulation of peritonsillar arteries or veins can lead to bleeding immediately after surgery. Delayed bleeding occurs during the inflammatory phase of healing, usually 7 to 10 days after surgery. Bleeding can be controlled safely in most cases but usually requires a second, potentially more dangerous general anesthetic. If bleeding is severe or the child is far from a medical facility, exsanguination may occur requiring transfusion or leading to death. Other less common tonsillectomy sequelae include facial burns, airway fires, airway edema, postobstructive pulmonary edema, sepsis, disorders of taste, velopharyngeal insufficiency, and nasopharyngeal stenosis.
Which Tonsillectomy to Do
Extracapsular tonsillectomy
Standard extracapsular tonsillectomy consists of the en bloc excision of the palatine tonsil and its enveloping capsule, usually including a portion of the anterior tonsillar pillar for exposure. It removes the tonsil quickly and completely, leaving little chance of tonsillar regrowth or future peritonsillar abscess. Extracapsular tonsillectomy produces a relatively large oropharyngeal wound that exposes the superior and middle constrictor muscles, bridging tonsillar arteries, and the tonsillar venous plexus. The glossopharyngeal nerve, peritonsillar fat, and tongue base muscles are nearby structures that are occasionally exposed during excision ( Fig. 4 A). This complete extracapsular procedure has been the gold standard operation since the early 20th century, employed in all major studies of the effectiveness of tonsillectomy.