Pediatric stridor is an important symptom of upper airway obstruction, and must be recognized early by evaluating physicians. Proper evaluation and management, both acutely and chronically, can provide improved outcomes and better quality of life for patients. This article discusses the physiology of stridor and its intimate relation to airway anatomy, the work-up of the stridorous child, and recent advances in treatment, and provides illustrative examples of common lesions.
Key points
- •
Stridor is a symptom of upper airway obstruction, and can not only be heard but also visualized.
- •
Complete and efficient evaluation and diagnosis of the stridorous child is critical for safe and timely management and intervention.
- •
A wealth of ancillary diagnostic studies are available for airway evaluation, which can tailor further intervention, but operative endoscopy remains the mainstay of diagnosis and intervention.
- •
A thorough understanding of airway anatomy and associated obstructive lesions equips the surgeon for intervention with decreased risk of further injury.
- •
Creation of simulation scenarios and a multidisciplinary approach to the child with stridor may improve the physician and the team approach and subsequently the outcome.
| BVCP | Bilateral vocal cord paralysis |
| CT | Computed tomography |
| DISE | Drug-induced sleep endoscopy |
| ED | Emergency department |
| EoE | Eosinophilic esophagitis |
| GERD | Gastroesophageal reflux disease |
| HIB | Haemophilus influenzae B |
| HPV | Human papillomavirus |
| LPR | Laryngopharyngeal reflux |
| MRI | Magnetic resonance imaging |
| OSA | Obstructive sleep apnea |
| RRP | Recurrent respiratory papillomatosis |
| SGH | Subglottic hemangioma |
| SGS | Subglottic stenosis |
| UVCP | Unilateral vocal cord paralysis |
Introduction
Stridor is a symptom and not a diagnosis ( Table 1 ). It is defined by a partial obstruction of the airway caused by abnormal apposition of 2 tissue surfaces in close proximity, with resultant turbulent airflow. This condition produces a high-pitched sound known as stridor. The degree of obstruction can range from minimal to life threatening, and stridor may be inconsequential or a sign of impending airway collapse. Those untrained in the evaluation and management of a stridorous child are uncomfortable with the symptom and fearful of the potential implications. In some circumstances, without adequate airway protection or intervention, respiratory collapse may ensue, particularly in young children.
| Level of Obstruction | Cause | Diagnostic Studies | Management/Treatment Options |
|---|---|---|---|
| Pharynx | Vallecular cyst | Laryngoscopy, CT | Surgical excision |
| Glossoptosis | Laryngoscopy, sleep-state endoscopy, polysomnogram | CPAP, posterior glossectomy, suture tongue base advancement, tracheotomy if severe | |
| Supraglottis | Laryngomalacia | Laryngoscopy, feeding evaluation | Acid suppression treatment Supraglottoplasty if severe |
| Laryngocele | Laryngoscopy, CT | Surgical excision | |
| Epiglottitis | Flexible laryngoscopy | Steroids, antibiotics Secure airway if indicated | |
| Glottis | Bilateral vocal fold paralysis | Fiber optic laryngoscopy CT Chest if indicated MRI head if indicated | Tracheotomy, Cordotomy/cordectomy laryngotracheoplasty |
| Glottic web | Laryngoscopy, genetic testing | Open or endoscopic web lysis with keel | |
| Recurrent respiratory papilloma | Flexible laryngoscopy, operative endoscopy, biopsy | Endoscopic excision, cidofovir | |
| Subglottis | Inflammatory croup | Laryngoscopy, airway films | Corticosteroids, nebulized saline |
| Reflux or EoE related | Gastroenterology consult pH/impedance probe Empiric suppression therapy | Acid suppression treatment | |
| Subglottic stenosis | Airway films, airway endoscopy | Endoscopic or open airway expansion surgery (LTR/CTR) | |
| Hemangioma | Airway endoscopy | Propranolol, corticosteroids, open excision, laser excision | |
| Trachea | Primary tracheomalacia | Airway fluoroscopy, airway endoscopy | Observation, and medical management of inflammation Tracheotomy if severe |
| Secondary tracheomalacia from extrinsic compression | Airway fluoroscopy, airway endoscopy, CTA chest, 3D reconstruction MRI | Surgical management of vascular ring | |
| Complete tracheal rings | CTA chest, 3D reconstruction, airway endoscopy, cardiac w/u | Slide tracheoplasty | |
| Airway foreign body | Airway films and chest radiographs | Airway endoscopy with removal |
The evaluation and airway management of infants and children with stridor continues to evolve, with technological advancements and improved understanding of the impact of inflammatory triggers and trauma in the causation of airway obstruction and stridor. Preventive measures have been used to curtail pediatric stridor. The widespread use of Haemophilus influenzae B (HIB) vaccine has essentially eliminated HIB-induced epiglottitis. The incidence of stridor caused by acquired subglottic stenosis (SGS) in neonates has declined dramatically over several decades because of improved airway management of the intubated infant; however, those surviving may have multiple medical comorbidities that influence evaluation, management, and outcome. The advancements in technology for optical visualization of the airway and expanded surgical armamentarium have allowed surgeons to push the limits of endoscopic surgery for airway management in children with stridor. Serendipitous discovery of the application of propranolol for management of airway hemangiomas has revolutionized treatment. Adoption of slide tracheoplasty for complete tracheal rings has greatly reduced the morbidity and mortality traditionally associated with these lesions. This article reviews the pathophysiology of stridor, and discusses key concepts and advances in diagnosis and management of common causes of stridor.
Introduction
Stridor is a symptom and not a diagnosis ( Table 1 ). It is defined by a partial obstruction of the airway caused by abnormal apposition of 2 tissue surfaces in close proximity, with resultant turbulent airflow. This condition produces a high-pitched sound known as stridor. The degree of obstruction can range from minimal to life threatening, and stridor may be inconsequential or a sign of impending airway collapse. Those untrained in the evaluation and management of a stridorous child are uncomfortable with the symptom and fearful of the potential implications. In some circumstances, without adequate airway protection or intervention, respiratory collapse may ensue, particularly in young children.
| Level of Obstruction | Cause | Diagnostic Studies | Management/Treatment Options |
|---|---|---|---|
| Pharynx | Vallecular cyst | Laryngoscopy, CT | Surgical excision |
| Glossoptosis | Laryngoscopy, sleep-state endoscopy, polysomnogram | CPAP, posterior glossectomy, suture tongue base advancement, tracheotomy if severe | |
| Supraglottis | Laryngomalacia | Laryngoscopy, feeding evaluation | Acid suppression treatment Supraglottoplasty if severe |
| Laryngocele | Laryngoscopy, CT | Surgical excision | |
| Epiglottitis | Flexible laryngoscopy | Steroids, antibiotics Secure airway if indicated | |
| Glottis | Bilateral vocal fold paralysis | Fiber optic laryngoscopy CT Chest if indicated MRI head if indicated | Tracheotomy, Cordotomy/cordectomy laryngotracheoplasty |
| Glottic web | Laryngoscopy, genetic testing | Open or endoscopic web lysis with keel | |
| Recurrent respiratory papilloma | Flexible laryngoscopy, operative endoscopy, biopsy | Endoscopic excision, cidofovir | |
| Subglottis | Inflammatory croup | Laryngoscopy, airway films | Corticosteroids, nebulized saline |
| Reflux or EoE related | Gastroenterology consult pH/impedance probe Empiric suppression therapy | Acid suppression treatment | |
| Subglottic stenosis | Airway films, airway endoscopy | Endoscopic or open airway expansion surgery (LTR/CTR) | |
| Hemangioma | Airway endoscopy | Propranolol, corticosteroids, open excision, laser excision | |
| Trachea | Primary tracheomalacia | Airway fluoroscopy, airway endoscopy | Observation, and medical management of inflammation Tracheotomy if severe |
| Secondary tracheomalacia from extrinsic compression | Airway fluoroscopy, airway endoscopy, CTA chest, 3D reconstruction MRI | Surgical management of vascular ring | |
| Complete tracheal rings | CTA chest, 3D reconstruction, airway endoscopy, cardiac w/u | Slide tracheoplasty | |
| Airway foreign body | Airway films and chest radiographs | Airway endoscopy with removal |
The evaluation and airway management of infants and children with stridor continues to evolve, with technological advancements and improved understanding of the impact of inflammatory triggers and trauma in the causation of airway obstruction and stridor. Preventive measures have been used to curtail pediatric stridor. The widespread use of Haemophilus influenzae B (HIB) vaccine has essentially eliminated HIB-induced epiglottitis. The incidence of stridor caused by acquired subglottic stenosis (SGS) in neonates has declined dramatically over several decades because of improved airway management of the intubated infant; however, those surviving may have multiple medical comorbidities that influence evaluation, management, and outcome. The advancements in technology for optical visualization of the airway and expanded surgical armamentarium have allowed surgeons to push the limits of endoscopic surgery for airway management in children with stridor. Serendipitous discovery of the application of propranolol for management of airway hemangiomas has revolutionized treatment. Adoption of slide tracheoplasty for complete tracheal rings has greatly reduced the morbidity and mortality traditionally associated with these lesions. This article reviews the pathophysiology of stridor, and discusses key concepts and advances in diagnosis and management of common causes of stridor.
Anatomy and pathophysiology of stridor
Physics of Stridor
The phenomenon of stridor is mediated by 2 basic principles of physics: Poiseuille’s law and the Bernoulli principle. Poiseuille’s law of fluid dynamics describes the relationships among the variables involved in the rate of laminar flow of a fluid through a tube. This equation can be directly extrapolated to airflow through a tube:
The outstanding relationship in this equation is the proportion of flow rate (Q) to the radius of the tube to the fourth power, resulting in an exponential effect on flow rate related to any change in radius. When applied to the 4-mm diameter of a neonatal airway, 1 mm of edema reduces the cross-sectional area leading to a 75% reduction in airflow. Because of decreased cross-sectional area, airflow velocity increases and induces the effect of the Bernoulli principle. This principle states that as the velocity of airflow increases, the pressure exerted by airflow decreases. The application of the Bernoulli principle in a narrowed pediatric airway predicts that increased airflow velocity exerts negative pressure on the walls of the lumen, precipitating airway collapse ( Fig. 1 ). It is the resultant alteration of laminar flow and turbulence of the airflow that creates a vibratory resonant effect on tissues that are closely approximated, which then creates the sound described as stridor. Stridor can be heard during inspiration, expiration, or both phases of respiration. The phase of respiration in which stridor is heard usually correlates with a specific anatomic site and whether or not the site of obstruction is fixed or dynamic, as described later.

Anatomy of Stridor
Stridor can originate from a narrowing at any level of the airway. There are occasions when there are multiple levels of the airway involved. The site of obstruction and the nature of its structural support combined with increased airflow and the patient’s respiratory effort influence the observed characteristics of stridor ( Fig. 2 ).

Supraglottis and pharynx
Stridor related to supraglottic disease or narrowing is typically inspiratory. The supraglottis in an infant is funnel shaped, and although large in diameter relative to other parts of the larynx it contains multiple moving parts connected by soft tissue attachments. This anatomy results in a high level of structural mobility, which is an inherent requirement of the supraglottic functions of respiration, deglutition, and airway protection. In the infant, supraglottic stridor is the result of collapse of these mobile structures into the airway on inspiration. Because of the funnel shape of the supraglottis, expiration tends to separate the supraglottic structures, relieving the obstruction temporarily. The most common cause of infantile supraglottic stridor is laryngomalacia. In this condition a structurally small, tubular supraglottis and redundant supra-arytenoid tissue narrow the airway, resulting in pathologically increased airflow rate, and collapse based on the principles of airflow previously described ( Fig. 3 ). With supraglottic growth and neuromuscular maturation the child is less prone to symptoms of stridor caused by collapse. As children age, supraglottic conditions causing stridor tend to be less dynamic and more likely inflammatory, infectious, or acquired from complications of surgery or intubation. Only a fixed obstruction, such as severe supraglottic stenosis, could cause an expiratory component of stridor at this site.

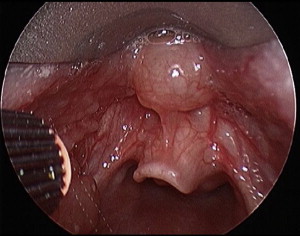
Dynamic pharyngeal collapse presents with noisy breathing called stertor (snoring) and must be differentiated from stridor. Stertor can be heard on inspiration, expiration, or both and is caused by the reverberation of soft structures from the level of the nasopharynx and pharynx. Stertor can occur in conjunction with stridor. Recognition and differentiation of this overlap are critical for appropriate treatment of upper airway obstruction. Stertor and stridor concurrently occur when there is extrinsic compression of the larynx or supraglottis by the tongue base as exemplified by a vallecular cyst ( Fig. 4 ) or glossoptosis. Stertor and stridor are also heard when adenotonsillar hypertrophy and laryngomalacia coexist.
Glottis
Stridor related to glottic disease or narrowing can be inspiratory or biphasic. The glottis includes the arytenoid cartilages and adductor and abductor muscles of the larynx. Because of the supporting muscular and cartilaginous structures, the glottis is more limited in its capacity for expansion or collapse. Stridor at this site is usually from a fixed, rather than a dynamic, obstruction. The degree of obstruction and phase of respiration in which the subsequent turbulent airflow is heard depends on how much of the diameter of the airway at this level is compromised. For example, a unilateral vocal fold paralysis (UVCD) may present with inspiratory stridor caused by partial obstruction, particularly in the neonate or in the setting of another airway lesion, and a bilateral paralysis or glottic stenosis presents with biphasic stridor caused by rapid airflow occurring in both directions without relief from the obstruction.
Subglottis
Stridor related to subglottic disease or narrowing is typically heard during both phases of respiration (ie, biphasic). The subglottis, the most inferior aspect of the larynx, comprises the cricoid cartilage, the only complete cartilage ring of the airway and the smallest portion of the infant larynx. The rigid and fixed nature of the cricoid cartilage and its noncompliant diameter, combined with sensitive respiratory mucosa in this region, make it uniquely prone to complications of inflammation or trauma. Stridor emanating from this site generally results from clinically significant airway obstruction that is difficult to manage ( Figs. 5 and 6 ).

Trachea
Stridor related to tracheal conditions or narrowing is typically expiratory but can be biphasic with fixed obstructive lesions. The trachea is divided into intrathoracic and extrathoracic components. Respiratory effort modulates intrathoracic pressures leading to dynamic changes in the diameter of the airway and subsequent turbulent airflow. The intrathoracic trachea is more susceptible to such pressure gradient changes, and more likely to collapse with triggers of increased pressure such as the act of coughing. The intrathoracic trachea expands during inspiration, when intrathoracic pressure is negative, and collapses with the positive intrathoracic pressure of expiration. The physics of this pressure gradient change explain why the trachea is the primary site of the airway implicated in pure expiratory stridor. As seen in Fig. 7 , congenital tracheomalacia is a classic example of expiratory stridor caused by dynamic collapse of the airway. Structures in close proximity but extrinsic to the airway, such as a vascular ring ( Fig. 8 ), can also cause tracheal compression and expiratory stridor. Similar to a fixed subglottic lesion, a fixed tracheal obstruction, as exemplified by complete tracheal rings ( Fig. 9 ), produce biphasic stridor.

A list of common or notable causes of pediatric stridor is shown in Box 1 .
Pharynx/hypopharynx
- •
Glossoptosis
- •
Laryngopharyngeal reflux
- •
Vascular malformation
- •
Vallecular cyst
- •
Supraglottis
- •
Laryngomalacia
- •
Laryngocele
- •
Stenosis
- •
Vascular malformation
- •
Neck mass
- •
Glottis
- •
Vocal cord paralysis (bilateral>unilateral)
- •
Intubation injury
- •
Laryngeal cleft
- •
Glottic web
- •
Stenosis
- •
Laryngeal trauma/fracture
- •
Subglottis
- •
Croup
- •
Intubation granulation/edema
- •
Acquired stenosis
- •
Hemangioma
- •
Cysts
- •
Congenital cricoid malformation
- •
Foreign body
- •
Tracheobronchus
- •
Tracheobronchomalacia
- •
Foreign body
- •
Complete tracheal rings
- •
Vascular compression
- •
Stenosis
- •
Bacterial tracheitis
- •
Neck/chest mass
- •
Evaluation of the stridorous patient
History
The evaluation of a stridorous patient requires an initial observation of the patient’s respiratory pattern, assessment of the severity of airway obstruction, and determination of the potential need for urgent or emergent airway intervention. The phase of respiration in which stridor occurs can help the clinician determine the level at which the obstruction is located. Patients who present with acute onset of stridor are most likely to have infection, inflammation, or foreign object aspiration as the cause. The initial point of evaluation is most often the emergency department (ED), where the goal of the ED physician is to assess risk for impending respiratory collapse. In this setting, vital signs, respiratory rate and effort, and oxygenation are assessed. Airway and chest radiographs are performed. A rapid evaluation for impending airway collapse and the need for intubation are conducted. The need for otolaryngology and anesthesia consultations for airway control is determined.
The otolaryngologist can provide additional diagnostic information using fiberoptic nasopharyngoscopy and laryngoscopy in the cooperative and clinically stable patient. The otolaryngologist has the expertise to assess the need for diagnostic or therapeutic intervention in the operating room or for establishing a surgical airway. Some institutions have created a critical airway assessment team with supporting bronchoscopic equipment in the ED to facilitate management in cases of critical airway obstruction. With the advancement of simulation as an educational tool, institutions are encouraged to develop simulation programs for the assessment of acute stridor requiring urgent intervention.
Most children present with chronic or gradual onset stridor in which the airway is restricted but stable and allows the physician to conduct a methodical evaluation. A carefully taken history helps to narrow the differential diagnosis and direct the diagnostic evaluation. Chronology of the event is important, because many causes can be predicted by symptom onset. For example, stridor associated with laryngomalacia is generally present within the first 2 weeks of life, whereas stridor associated with subglottic hemangiomas (SGH) begins around 2 months of life and is likely to be progressive. Other causes have a latency between lesion occurrence and onset of symptoms. For example, bilateral vocal cord paralysis (BVCP) may take several months to become symptomatic, whereas congenital SGS may only become clinically significant in early childhood as recurrent croup. Accompanying complaints or symptom triggers can guide the diagnosis and management of stridor. Hoarseness could signify a glottic mass (papilloma) or neurologic cause affecting the vagal nerve and vocal fold function. Feeding difficulty could indicate acid reflux or an anatomic anomaly such as a laryngeal cleft or tracheoesophageal fistula.
A query of the past medical history can also provide diagnostic clues to stridor. Stridor in the context of an intubation history is characteristic of acquired laryngotracheal stenosis. A history of neck, chest, or neurologic trauma or surgical procedures may indicate obstruction from a vocal cord weakness. Because children with chronic stridor are often misdiagnosed with other conditions such as asthma, a lack of response to typical therapies may indicate a structural cause in the tracheobronchial tree.
In patients with episodic stridor, an attempt should be made to identify the potential triggers and evaluate the severity of the paroxysms, to identify patients at risk for critical airway compromise and emergent respiratory events. Such patients require a diagnostic evaluation in an inpatient setting with appropriate monitoring during the evaluation ( Box 2 ).



