Auditory brainstem implants (ABIs) provide auditory perception in patients with profound hearing loss who are not candidates for the cochlear implant (CI) because of anatomic constraints or failed CI surgery. Herein, the authors discuss (1) preoperative evaluation of pediatric ABI candidates, (2) surgical approaches, and (3) contemporary ABI devices and their use in the pediatric population. The authors also review the surgical and audiologic outcomes following pediatric ABI surgery. The authors’ institutional experience and the nearly 200 cases performed in Europe and the United States indicate that ABI surgery in children can be safe and effective.
Key points
- •
Evaluation for pediatric auditory brainstem implant (ABI) candidacy includes a thorough neurotologic and neurosurgical consultation, audiologic evaluation including both behavioral and electrophysiologic testing, speech and language consultation, high-resolution temporal bone computed tomography and MRI imaging, and neuropsychological assessment of developmental milestones.
- •
Indications for an ABI in infants and children include bilateral cochlea aplasia/hypoplasia, cochlear nerve hypoplasia/aplasia, cochlear ossification, cochlear nerve fracture or cochlear nerve injury from bilateral temporal bone fractures, failed cochlear implantation caused by anatomic constraints or auditory neuropathy. Older children and teenagers with neurofibromatosis type 2 (NF2) are also candidates for the ABI.
- •
The retrosigmoid craniotomy approach is recommended for pediatric ABI because of the relative small size of the temporal bone in young children that would make a translabyrinthine craniotomy more difficult.
- •
Most complications following ABI surgery are minor in the hands of an experienced neurotology/neurosurgery team. The most common complication is a cerebrospinal fluid leak after surgery.
- •
Outcomes are generally modest among most pediatric ABI users, with most achieving sound awareness that enhances lip reading, but some realize closed-set or open-set speech recognition. Patients who do not have NF2 as the cause of deafness have better audiologic outcomes than those with NF2.
- •
Standardized outcome reporting across a growing number of pediatric ABI centers worldwide will be important in order to identify the factors that predict safe and effective ABI surgery in children.
| ABI | Auditory brainstem implant |
| CAP | Category of auditory performance |
| ChR | Channel rhodopsin |
| CI | Cochlear implant |
| CN | Cochlear nucleus |
| CNS | Central nervous system |
| CSF | Cerebrospinal fluid |
| DCN | Dorsal cochlear nucleus |
| EMG | Electromyographic |
| FDA | Food and Drug Administration |
| IAC | Internal auditory canal |
| IC | Inferior colliculus |
| NF2 | Neurofibromatosis type II |
| PABI | Penetrating auditory brainstem implant |
| VCN | Ventral cochlear nucleus |
Introduction
Providing meaningful sound perception to pediatric and adult patients with profound hearing loss has been the subject of intense research efforts for decades. Beginning with Djourno and Eyriès more than 50 years ago, the idea of an auditory prosthesis has undergone a dramatic evolution. These pioneers provided a detailed description for artificially transducing sound with an implantable induction coil that created auditory sensations via transcutaneous electric stimulation. Since then, technological advancements have facilitated the development of both cochlear implants (CIs) and auditory brainstem implants (ABIs). In parallel with improved microphone and battery technology, more advanced algorithms for speech processing as well as postoperative auditory rehabilitation and training on device use has further advanced the audiologic gains with implantable prostheses, offering the possibility of open-set speech recognition in most patients with severe to profound sensorineural deafness.
Although the CI implant has gained widespread acceptance and use, this technology has limitations. In cases whereby the cochlea and cochlear nerve are fully developed or are only mildly malformed (eg, Mondini or incomplete partition type 2 deformity), the CI is a reasonable option for hearing habilitation (in congenitally deaf children) or rehabilitation (in patients with postlingual deafness). The CI bypasses the inner hair cells of the cochlea to directly stimulate spiral ganglion cells, the first-order neurons of the auditory pathway. However, there is a subset of patients who are not candidates for a CI because of abnormal anatomy, such as an absent, scarred, or small cochlea or cochlear nerve. A CI is likely to provide modest benefits in these patients, with some exceptions. The ABI is an alternative approach to the CI and bypasses the cochlea, cochlear nerve, and any associated peripheral disease to electrically stimulate the second-order auditory neurons found in the cochlear nucleus (CN). The ABI is a modified CI whose surface electrode array is placed on or near the brainstem CN via the lateral recess of the fourth ventricle. The CN is the primary brainstem hub for type 1 auditory afferents originating in the cochlea and is the first center of auditory processing in the brain. Electrical stimulation of the electrode array crudely approximates the input that normally arises from the cochlear nerve by leveraging the tonotopic distribution of second-order auditory neurons within the CN. Most ABI users have neurofibromatosis type II (NF2) and receive sound detection that aids in lip reading.
In 1979, William Hitselberger and William House performed the first successful ABI surgery for an adult woman with NF2 following removal of her second vestibular schwannoma via a translabyrinthine craniotomy. This prototype implant had a single glass ball electrode that was placed via the lateral recess of the fourth ventricle in proximity to the dorsal CN (DCN) to provide auditory sensations. Eventually, technology developed to include a multiple electrode array and receiver stimulator that is forward compatible with modern receiver stimulators used with the CI. In 2000, Cochlear Corporation (Engelwood, CO) received approval from the Food and Drug Administration (FDA) for the 21 electrode Nucleus 24 ABI system for patients with NF2 aged 12 years and older. There are no audiologic candidacy criteria for the ABI in patients with NF2. Today, more than 1000 patients have received ABI surgery worldwide.
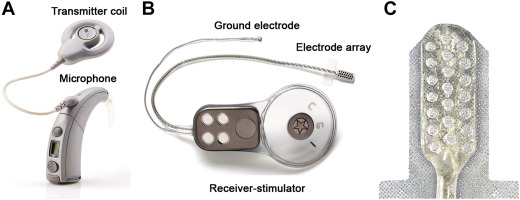
As of May 2015, the Nucleus 24 ABI system ( Fig. 1 ) was phased out; Cochlear Corporation will be introducing a new ABI system pending regulatory approval in the United States that until then may be used under FDA compassionate use exemption. The MED-EL (Durham, NC) also manufactures an ABI device ( Fig. 2 ) that has been used internationally for pediatric ABI surgery. Although it has not been submitted for formal FDA approval in the United States, it has been used under the FDA compassionate use exemption.

Patients with NF2 are the most common cohort of ABI candidates with deficits of the cochlear nerve related to tumor growth and compression that are not typically amenable to CI. Patients with NF2 have an autosomal dominant mutation that triggers the formation of vestibular schwannomas bilaterally along with a myriad of synchronous central nervous system (CNS) tumors. Growth of these vestibular schwannomas as well as resection with surgery and/or treatment with radiation often damages the cochlear nerve, resulting in bilateral retrocochlear hearing loss not helped with hearing aids or CIs.
Over the past decade, there has been growing interest in the ABI to provide hearing sensations to non-NF2 patients with cochlear or cochlear nerve pathology. Professor Vittorio Colletti’s work at the University of Verona and more recently in Milan has propelled enthusiasm for ABI surgery in non-NF2–related deafness. Colletti and colleagues demonstrated that open-set sentence recognition is possible with the ABI in adult non-NF2 users compared with NF2 users. Since those initial studies in adult patients, Colletti’s group expanded the indications for ABI surgery to children and infants who are not CI candidates. Colletti performed the first pediatric ABI surgery for auditory nerve aplasia in 2001 and has performed approximately 100 non-NF2 pediatric ABI surgeries since that time, including surgery on an 8 month old, the youngest infant to date. Much like Colletti, Professor Levent Sennaroglu from the University of Hacettepe, Turkey has driven international experience in Ankara with more than 70 non-NF2 pediatric ABIs. Remarkably, the combined experience of these two groups has been associated with relatively low morbidity. There have been a small number of transient facial nerve palsies and cerebrospinal fluid (CSF) leaks, which have been managed conservatively. More strikingly, a significant number of these children who were implanted at a young age and had no significant developmental issues have subsequently achieved either closed or open-set speech recognition following ABI surgery. Pediatric ABI surgery in non-NF2 children in the United States began initially in 2012, with the first child implanted in 2012 at New York University. There are now 4 investigational device exemption clinical trials in the United States: University of North Carolina-Chapel Hill, Massachusetts Eye and Ear Infirmary-Harvard Medical School, the Los Angeles Pediatric ABI team, and New York University.
In this article, we summarize the preoperative assessment of pediatric ABI candidates, the surgical approach, postoperative management issues, complications, and review published outcomes in this unique cohort. Based on findings from Italy and Turkey and our early experience in the U.S., we believe that ABI surgery is a safe and effective option for auditory habilitation in deaf children who are not candidates for the CI.
Introduction
Providing meaningful sound perception to pediatric and adult patients with profound hearing loss has been the subject of intense research efforts for decades. Beginning with Djourno and Eyriès more than 50 years ago, the idea of an auditory prosthesis has undergone a dramatic evolution. These pioneers provided a detailed description for artificially transducing sound with an implantable induction coil that created auditory sensations via transcutaneous electric stimulation. Since then, technological advancements have facilitated the development of both cochlear implants (CIs) and auditory brainstem implants (ABIs). In parallel with improved microphone and battery technology, more advanced algorithms for speech processing as well as postoperative auditory rehabilitation and training on device use has further advanced the audiologic gains with implantable prostheses, offering the possibility of open-set speech recognition in most patients with severe to profound sensorineural deafness.
Although the CI implant has gained widespread acceptance and use, this technology has limitations. In cases whereby the cochlea and cochlear nerve are fully developed or are only mildly malformed (eg, Mondini or incomplete partition type 2 deformity), the CI is a reasonable option for hearing habilitation (in congenitally deaf children) or rehabilitation (in patients with postlingual deafness). The CI bypasses the inner hair cells of the cochlea to directly stimulate spiral ganglion cells, the first-order neurons of the auditory pathway. However, there is a subset of patients who are not candidates for a CI because of abnormal anatomy, such as an absent, scarred, or small cochlea or cochlear nerve. A CI is likely to provide modest benefits in these patients, with some exceptions. The ABI is an alternative approach to the CI and bypasses the cochlea, cochlear nerve, and any associated peripheral disease to electrically stimulate the second-order auditory neurons found in the cochlear nucleus (CN). The ABI is a modified CI whose surface electrode array is placed on or near the brainstem CN via the lateral recess of the fourth ventricle. The CN is the primary brainstem hub for type 1 auditory afferents originating in the cochlea and is the first center of auditory processing in the brain. Electrical stimulation of the electrode array crudely approximates the input that normally arises from the cochlear nerve by leveraging the tonotopic distribution of second-order auditory neurons within the CN. Most ABI users have neurofibromatosis type II (NF2) and receive sound detection that aids in lip reading.
In 1979, William Hitselberger and William House performed the first successful ABI surgery for an adult woman with NF2 following removal of her second vestibular schwannoma via a translabyrinthine craniotomy. This prototype implant had a single glass ball electrode that was placed via the lateral recess of the fourth ventricle in proximity to the dorsal CN (DCN) to provide auditory sensations. Eventually, technology developed to include a multiple electrode array and receiver stimulator that is forward compatible with modern receiver stimulators used with the CI. In 2000, Cochlear Corporation (Engelwood, CO) received approval from the Food and Drug Administration (FDA) for the 21 electrode Nucleus 24 ABI system for patients with NF2 aged 12 years and older. There are no audiologic candidacy criteria for the ABI in patients with NF2. Today, more than 1000 patients have received ABI surgery worldwide.
As of May 2015, the Nucleus 24 ABI system ( Fig. 1 ) was phased out; Cochlear Corporation will be introducing a new ABI system pending regulatory approval in the United States that until then may be used under FDA compassionate use exemption. The MED-EL (Durham, NC) also manufactures an ABI device ( Fig. 2 ) that has been used internationally for pediatric ABI surgery. Although it has not been submitted for formal FDA approval in the United States, it has been used under the FDA compassionate use exemption.
Patients with NF2 are the most common cohort of ABI candidates with deficits of the cochlear nerve related to tumor growth and compression that are not typically amenable to CI. Patients with NF2 have an autosomal dominant mutation that triggers the formation of vestibular schwannomas bilaterally along with a myriad of synchronous central nervous system (CNS) tumors. Growth of these vestibular schwannomas as well as resection with surgery and/or treatment with radiation often damages the cochlear nerve, resulting in bilateral retrocochlear hearing loss not helped with hearing aids or CIs.
Over the past decade, there has been growing interest in the ABI to provide hearing sensations to non-NF2 patients with cochlear or cochlear nerve pathology. Professor Vittorio Colletti’s work at the University of Verona and more recently in Milan has propelled enthusiasm for ABI surgery in non-NF2–related deafness. Colletti and colleagues demonstrated that open-set sentence recognition is possible with the ABI in adult non-NF2 users compared with NF2 users. Since those initial studies in adult patients, Colletti’s group expanded the indications for ABI surgery to children and infants who are not CI candidates. Colletti performed the first pediatric ABI surgery for auditory nerve aplasia in 2001 and has performed approximately 100 non-NF2 pediatric ABI surgeries since that time, including surgery on an 8 month old, the youngest infant to date. Much like Colletti, Professor Levent Sennaroglu from the University of Hacettepe, Turkey has driven international experience in Ankara with more than 70 non-NF2 pediatric ABIs. Remarkably, the combined experience of these two groups has been associated with relatively low morbidity. There have been a small number of transient facial nerve palsies and cerebrospinal fluid (CSF) leaks, which have been managed conservatively. More strikingly, a significant number of these children who were implanted at a young age and had no significant developmental issues have subsequently achieved either closed or open-set speech recognition following ABI surgery. Pediatric ABI surgery in non-NF2 children in the United States began initially in 2012, with the first child implanted in 2012 at New York University. There are now 4 investigational device exemption clinical trials in the United States: University of North Carolina-Chapel Hill, Massachusetts Eye and Ear Infirmary-Harvard Medical School, the Los Angeles Pediatric ABI team, and New York University.
In this article, we summarize the preoperative assessment of pediatric ABI candidates, the surgical approach, postoperative management issues, complications, and review published outcomes in this unique cohort. Based on findings from Italy and Turkey and our early experience in the U.S., we believe that ABI surgery is a safe and effective option for auditory habilitation in deaf children who are not candidates for the CI.
Treatment goals and outcomes
The treatment goals for pediatric ABI surgery are (1) safe and successful placement of ABI electrode array through the foramen of Luschka (to bring electrode in close proximity to cochlear nucleus), (2) measurable electrically-evoked auditory brainstem responses (EABR) seen intraoperatively, (3) minimizing surgical complications such as CSF leak and facial nerve injury, (4) habilitation/rehabilitation of deafness with meaningful sound detection on behavioral testing, and (5) avoidance of side effects caused by stimulation of non-auditory pathways (e.g. facial nerve, glossopharyngeal nerve). As the range of clinical outcomes varies widely (see Outcomes), the stated goals should include a substantial conversation with families and patients regarding both the risks of craniotomy surgery in a young child as well as the reasonable expectation of audiologic outcomes. A team based tertiary care setting is the ideal environment where pediatric ABI candidates and their families can be carefully evaluated for possible surgery. At the Wilson ABI Program at Massachusetts Eye and Ear Infirmary and Massachusetts General Hospital, all candidates participate in a formal consultation with pediatric neurotology, neurosurgery, audiology, speech therapy, and neuropsychology to ensure adequate communication regarding the treatment goals, frank discussion of surgical risks, and review of outcomes.
Preoperative planning and preparation
Implant Systems
The ABI system is modular, with both external and internal components that capture, transduce, process, and propagate auditory stimuli into electrical signals to the electrode array, similar to that of the CI. The external components include a microphone, battery, speech processor, and transmitter coil. Acoustic stimuli are processed and transmitted as electronic signals to a receiver-stimulator via an induction coil. The surgically implanted receiver-stimulator then carries these signals to the CN via a rigid surface multi-electrode array that consists of 12 (MED-EL) to 21 (Cochlear) electrode contacts (see Figs. 1 and 2 ). These platinum alloy electrode contacts trigger neuronal signaling in the CN, thereby stimulating upstream auditory pathways and providing sound perception.
The ABI continues to leverage sound-processing algorithms originally developed for CIs. However, because the tonotopic arrangement of the DCN is orthogonal to the surface of the brainstem, capturing a specific spectral frequency with each electrode is more challenging. This organization is in contrast to the CI electrode whose position in the scala tympani follows the tonotopic organization of the cochlea. Indeed, some studies suggest that there is limited benefit to an ABI electrode array beyond 7 leads, providing a rationale for exploring penetrating electrodes that can better stimulate multiple tonotopic layers of the DCN. However, the initial experience using a novel penetrating ABI (PABI) array developed in Los Angeles in adult patients with NF2 was not associated with improved outcomes. This PABI system also includes surface contacts, and overall auditory performance was not enhanced in the PABI-only condition. Side effects were also seen in patients even with the ABI turned off. Finally, stimulation one level higher at the inferior colliculus (IC) has been proposed, with the hypothesis that patients with NF2 may have damage to the CN that limits the utility of an ABI. However, outcomes in a small cohort of patients with IC electrode placement (either penetrating or surface) have not demonstrated improved outcomes compared with traditional electrode placement near the CN.
In the United States, Cochlear Corporation previously offered the multichannel Nucleus 24 ABI system, which was approved by the FDA in 2000 for patients with NF2 aged 12 years and older (see Fig. 1 ). The Nucleus 24 ABI consists of 21 electrode contacts measuring 0.7 mm in diameter arranged along a polymeric silicon (Silastic) paddle with polyethylene terephthalate (Dacron) mesh backing. This ABI has been used for the approximately 20 pediatric ABI surgeries performed in the United States. The Cochlear system uses the SPEAK coding strategy, originally developed for the Nucleus CI. Although the Nucleus 24 ABI is technically capable of more sophisticated speech-processing algorithms, including continuous interleaved sampling (CIS) and advanced combination encoding, the FDA has not approved these other sound-processing strategies.
However, as of May 2015, the Nucleus 24 ABI has been phased out. In late 2015 or 2016, Cochlear Corporation will be introducing a new ABI system pending US regulatory approval of their new profile platform. Until then, their new ABI may only be used in the United States after securing approval through an FDA compassionate use exemption.
The magnet within the polymeric silicon pocket of the surgically implanted ABI receiver stimulator is retained to improve close contact between the external speech processor and the internal components. This retention is possible because most non-NF2 pediatric ABI candidates do not require routine MRI surveillance in comparison with all patients with NF2. Ideally, future ABI designs that reach regulatory approval for use in the United States should include magnet designs that allow for MRI scans, as a young non-NF2 child who receives an ABI may need imaging done in their lifetime for unrelated reasons. As one example, MED-EL has a SYNCHRONY ABI (not approved for the United States) that allows for 1.5-T MRI scans without the need for magnet removal or even a pressure dressing.
In contrast, patients with NF2 require serial MRIs to monitor the growth of multiple CNS tumors; therefore, most centers will replace the ABI magnet during craniotomy surgery with a nonmagnetic metallic spacer provided by the company’s prior electrode placement. The scalp is tattooed in the region of the receiver-stimulator telecoil after the ABI is inserted into the subperiosteal pocket. The tattoo provides a visual guide for patients to place an adhesive magnetic disk on the scalp, facilitating headpiece retention. At Massachusetts Eye and Ear, we also offer focal laser hair removal of the scalp in the region of the telecoil (especially important in patients with thick or coarse hair) to improve retention of the adhesive magnetic disk.
A 1.5-T MRI can be obtained in the United States with the magnet surgically removed from the FDA-approved ABI. Some international centers will retain the magnet in the ABI in patients with NF2 to improve device retention and patient use. In these cases, a 1.5-T MRI scan is performed with a tight mastoid dressing and a custom mold or plastic card placed over the scalp flap in the location of the receiver-stimulator.
MED-EL offers an ABI, but this device is only available in the United States through compassionate use exemption from FDA. The MED-EL ABI has mirrored advancements in the MED-EL CI over the last two decades, with the current iteration being the SYNCHRONY ABI, and has been used internationally for both NF2 and non-NF2 applications. It consists of an internal receiver-stimulator and external microphone speech processor with attached transmission coil. The MED-EL ABI has 12 platinum electrode contacts (.55 mm diameter) and uses a simplified placing electrode to identify the optimal location for EABRs. This placing electrode is smaller than the actual ABI paddle and can help localize the CN before committing to the actual ABI. This system includes the SONNET audio processor which offers the High Definition Continuous Interleaved Sampling (HDCIS) coding strategy. Finally, the SYNCHRONY ABI has approval in Europe for MRI at 0.2, 1.0 and 1.5T without the need to remove the magnet, although the magnet is optionally removable in the event that the area to be imaged is in the vicinity of the implant itself.
The Advanced Bionics (Valencia, CA) ABI was based on the Clarion 1.2 CI; however, after a brief period of use in Europe, Advanced Bionics discontinued the Clarion ABI. This device consisted of a polymeric silicone electrode array with 16 platinum-iridium electrodes (1.0 mm diameter). This implant was manufactured without a magnet and used a special headset to hold the external headpiece in position.
Evaluation
Evaluation of a child for possible ABI surgery is a multidisciplinary effort requiring evaluation of several specialists in addition to the neurotologist and neurosurgeon. All patients undergo a preoperative history and examination and complete surgical assessment, behavioral and electrophysiologic measurement of hearing, formal speech therapy evaluation, and neuropsychological consultation. In prelingually deafened patients, both behavioral thresholds and acoustically evoked auditory brainstem responses (ABRs) are carefully analyzed and repeated as needed to ensure that there is no residual hearing that might support a CI trial before consideration of an ABI. Pediatric patients receive a comprehensive evaluation of their language skills by a speech and language pathologist as well as a formal neuropsychological evaluation to assess overall progress with cognitive, motor, and language development. Sign language is encouraged in order to provide a basis for language development in prelingually deafened pediatric ABI candidates as overall outcomes with the ABI still lag behind the CI. In addition, neurodevelopmental delay is more commonly found among pediatric ABI candidates compared with CI candidates. Finally, a crucial component of the preoperative evaluation is determining whether there is an appropriate level of family support and realistic expectations to facilitate success with an ABI in a congenitally deafened child.
Radiographic Assessment
Imaging with high-resolution computed tomography (CT) and MRI followed by interpretation by a tertiary center neuroradiologist is essential to assess the anatomic details of the internal auditory canal (IAC), lateral recess, and brainstem. Typically this imaging consists of a temporal bone CT as well as MRI with T2-weighted fast imaging employing steady-state acquisition (FIESTA)/constructive interference into steady state sequences. At Massachusetts Eye and Ear, we rely on T2-weighted 3-dimensional turbo spin echo with direct driven equilibrium radio frequency reset pulse parasagittal imaging of the IAC. Reconstructions of the IAC on MRI to image the cross section of the auditory nerve are often not sufficient to rule out auditory nerve hypoplasia compared with direct parasagittal imaging. The Massachusetts Eye and Ear imaging protocol for pediatric ABI candidates offers enhanced visualization of the IAC and neural anatomy ( Fig. 3 ), with a direct impact on clinical decision making. The surgical team should also carefully evaluate the pontomedullary junction, taking note of the lower cranial nerves and lateral recess of the fourth ventricle. The presence of vascularity, scar tissue, or anomalous lower nerves may influence the surgical approach with the ABI electrode. Because the CN is not easily distinguishable on MRI, the surgeon is limited to a gross evaluation of the brainstem and cranial nerve rootlets.
Selection Criteria and Candidacy
In the United States, the FDA has approved ABI surgery in patients with NF2 fulfilling several specific criteria ( Box 1 ). There are no audiologic criteria for this cohort because of (1) the history of ABI surgery with early cases performed in patients who were undergoing removal of a second vestibular schwannoma and left with no hearing after tumor resection and (2) the natural history of NF2 resulting in profound hearing loss in virtually all affected patients. Clinical studies have shown that about 8% of patients will fail to gain any useful hearing with the ABI. Hence, some centers have placed the ABI even when there is residual hearing in the contralateral ear in order to maximize the chances of providing sound awareness in at least one ear. With the advent of chemotherapeutic options for NF2 including bevacizumab, a monoclonal antibody against the ecto-domain of vascular endothelial growth factor, early ABI placement has been increasingly deferred in favor of maximizing the duration of acoustic hearing before tumor resection and ABI surgery. At the Massachusetts Eye and Ear, all patients with NF2 with tumor burden and progressive hearing loss are first evaluated at the Neurofibromatosis Clinic at Massachusetts General Hospital for a multidisciplinary evaluation and possible chemotherapy trial before consideration for tumor and/or ABI surgery.
- •
Diagnosis of NF2
- •
12 years old or older
- •
High degree of motivation to comply with rehabilitation
- •
Reasonable patient and family expectations
Notably, there are no audiologic criteria.
Although most adult ABI users have NF2, only a small percentage of pediatric patients are implanted because of NF2. Most pediatric ABI users are younger children with anatomic limitations that preclude successful CI surgery. Several studies from Europe have suggested improved outcomes in nontumor adult and pediatric patients compared with patients with NF2. Accordingly, a European ABI consensus group concluded that indications for pediatric ABI surgery should include the following ( Box 2 ) :
- •
Prelingually deafened children with inner ear malformation and cochlear nerve hypoplasia/aplasia
- •
Postlingually deafened children with cochlear ossification from meningitis, cochlear nerve avulsion from bilateral temporal bone fractures, gross cochlear ossification caused by otosclerosis, or intractable facial nerve stimulation with CI.
Well-defined congenital indications
- 1.
Complete labyrinthine aplasia (Michel aplasia)
- 2.
Cochlear aplasia
- 3.
Cochlear nerve aplasia
- 4.
Cochlear aperture aplasia
Possible congenital indications
- 1.
Hypoplastic cochleae with cochlear aperture hypoplasia
- 2.
Common cavity and incomplete partition type I cases if the cochlear nerve is not present.
- 3.
Common cavity and incomplete partition type I cases if the cochlear nerve is present. If the nerve is present, the distribution of the neural tissue in the abnormal cochlea is unpredictable and an ABI is indicated if CI fails to elicit an auditory sensation.
- 4.
Unbranched cochleovestibular nerve is a challenge. If there is a doubt, a CI can be used first, and ABI can be reserved for the patients with an insufficient response.
- 5.
Hypoplastic cochlear nerves (<50% of usual size of cochlear nerve or less than diameter of the facial nerve) present a dilemma. If a sufficient amount of neural tissue cannot be followed into the cochlear space, an ABI may be indicated.
Acquired indications
- 1.
Postlingual deafness caused by meningitis with severe ossification of the cochlea (white cochleae on CT with no cochlear duct signal on MRI) should undergo ABI surgery. If the cochlea appears patent on T2 MRI, CI should be the first option.
- 2.
Bilateral temporal bone transverse fractures with cochlear nerve avulsion.
- 3.
Cochlear otosclerosis with gross destruction of the cochlea; in addition, some otosclerosis patients have abnormal facial nerve stimulation, which may limit CI use.
- 4.
Unmanageable facial nerve stimulation with CI.
In pediatric patients with cochlear and cochlear nerve aplasia, consideration of an ABI without a CI trial is reasonable. In contrast, a CI could be offered as a first option for a child with profound hearing loss and cochlear nerve hypoplasia or partial cochlear ossification, provided that the inner ear anatomy supports reasonable electrode insertion with a standard array. The decision to pursue CI surgery should also be influenced by any detectable behavioral thresholds that may be associated with auditory neuronal viability. Ultimately, comprehensive psychophysical and electrophysiologic measurements obtained by an experienced pediatric audiologist is critical to determine whether a congenitally deafened child with poor neural anatomy would benefit from a CI trial before ABI surgery. In some centers, EABRs generated by cochlear promontory electrical stimulation can help discern whether a functional neural connection exists between the cochlea and central auditory pathways. Patients with inconsistent or absent EABR responses are unlikely to derive substantial benefit from the CI.
The ABI research team at Massachusetts Eye and Ear recently reviewed auditory implant candidacy in the United States to determine the relative need for ABI surgery. Based on documented rates of cochlear and cochlear nerve aplasia/hypoplasia and population-level sensorineural hearing loss data, we estimated that 2.1% of potential implant candidates (1266 children) meet absolute indications for an ABI in the United States, with another 3.2% of potential implant candidates (1928 children) meeting relative indications for an ABI. The actual number may be smaller after imaging, as most children who undergo MRI scans to evaluate the auditory nerve rely on reformatted parasagittal images that do not provide adequate resolution of detailed neural anatomy. Pediatric ABI candidates are rare, but there is a legitimate need for dedicated ABI centers of excellence to gather the experience and expertise required to offer safe surgery and ABI mapping for this specialized cohort of deaf children who are not candidates for the CI.
The European consensus group on ABI surgery in children has explored the optimal time for ABI surgery in children. At earlier ages, children demonstrate increased plasticity and are likely to accrue greater benefit from early auditory sensations; however, infants less than 1 year of age have less blood and CSF volume with a smaller window of access to the lateral recess, potentially increasing the risks of craniotomy and ABI surgery. Based on these factors, there is consensus that implanting pediatric patients between 18 months and 3 years of age may provide a compromise between these physiologic and surgical considerations. To date, almost 200 children have received ABIs internationally, with approximately 20 non-NF2 pediatric ABIs placed in the United States as of June 2015.
Our pediatric ABI candidacy algorithm at Massachusetts Eye and Ear includes a formal multidisciplinary preoperative evaluation, retrosigmoid craniotomy and ABI placement, and postoperative care as outlined in Box 3 .



