Purpose
To better characterize a novel spectral-domain optical coherence tomography (OCT) presentation, termed paracentral acute middle maculopathy, to describe this finding in patients with nonischemic central retinal vein occlusion (CRVO), and to support a proposed pathogenesis of intermediate and deep retinal capillary ischemia.
Design
Retrospective observational case series.
Methods
Clinical histories, high-resolution digital color imaging, red-free photography, fluorescein angiography, near-infrared reflectance, and spectral-domain OCT images of 484 patients with acute CRVO from 2 centers were evaluated for the presence of coexisting paracentral acute middle maculopathy.
Results
Of 484 patients diagnosed with CRVO, 25 (5.2%) demonstrated evidence of concurrent paracentral acute middle maculopathy. Patients averaged 51 years of age and presented with complaints of paracentral scotomas. All patients demonstrated hyper-reflective plaquelike lesions at the level of the inner nuclear layer by spectral-domain OCT and showed corresponding dark-gray lesions on near-infrared reflectance and perivenular deep retinal whitening on color fundus photography. There was no fluorescein angiographic correlate to these lesions. On follow-up spectral-domain OCT imaging, the lesions had resolved into areas of inner nuclear layer atrophy with persistence of scotomas.
Conclusions
Paracentral acute middle maculopathy refers to characteristic hyper-reflective spectral-domain OCT lesions involving the middle layers of the retina at the level of the inner nuclear layer that may develop in response to ischemia of the intermediate and deep capillary plexuses. This series is the largest to describe this spectral-domain OCT finding to date, and it is the first to associate it with nonischemic CRVO.
Recently, we identified characteristic bandlike hyper-reflective spectral-domain optical coherence tomography (OCT) lesions in patients with presumed acute macular neuroretinopathy involving the middle layers of the retina at the level of the inner nuclear layer, a novel finding we termed paracentral acute middle maculopathy. Since these initial reports, a smaller case series additionally observed this finding in 4 patients, including 1 with underlying diabetic retinopathy. Retinal capillary ischemia has been proposed as the causative factor in the development of these lesions, which localize histologically at the level of the intermediate and deep retinal capillary plexuses flanking the inner and outer boundaries of the inner nuclear layer, respectively.
This article describes 25 new cases of paracentral acute middle maculopathy occurring in association with acute nonischemic central retinal vein occlusion (CRVO), and will help to further elucidate the underlying pathogenesis of these middle retinal lesions.
Methods
Institutional review board approval for this retrospective 2-center study was obtained through the Wills Eye Hospital, Philadelphia, Pennsylvania, and the University of California, Los Angeles, Office of the Human Research Protection Program. Research adhered to the tenets of the Declaration of Helsinki and was conducted in accordance with regulations set forth by the Health Insurance Portability and Accountability Act.
Using International Classification of Diseases, 9th Revision (ICD-9), billing codes for CRVO, 2 of our authors (ER, DS) reviewed the spectral-domain OCT imaging database at each of their retinal care centers and studied the findings of 484 cases of CRVO diagnosed between January 2010 and September 2013. We identified 25 cases of acute CRVO with simultaneous acute paracentral acute middle maculopathy lesions and assessed the clinical and imaging data for each case, focusing primarily on multimodal imaging correlations. Baseline and follow-up demographic, clinical and laboratory data were extracted from patient charts and analyzed. Statistical analysis was performed by a simple 2-tailed t test using GraphPad Software (GraphPad, La Jolla, California).
High-resolution digital color imaging, red-free photography, and fluorescein angiography at baseline presentation were analyzed, when available, for each patient. Initial near-infrared reflectance and spectral-domain OCT examinations utilizing the Heidelberg Spectralis (Heidelberg Engineering, Heidelberg, Germany) were evaluated at baseline in every patient and correlated with subsequent follow-up scans during the course of a patient’s follow-up when available. We used the registration feature specific to Heidelberg Spectralis, which allows each spectral-domain OCT B-scan to be coupled to its exact location on the near-infrared reflectance image, facilitating point-to-point correlations of the retinal findings between the near-infrared reflectance and spectral-domain OCT images.
Results
Of the 484 patients diagnosed with CRVO, 25 (5.2%) demonstrated evidence of concurrent paracentral acute middle maculopathy at the time of their initial office evaluations. Baseline patient demographics and ocular examination findings in these eyes are outlined in the Table . The mean age at presentation was 51 years (range, 19–78; standard deviation (SD), 16.6) in the group with paracentral acute middle maculopathy, which was significantly younger than the 69.6 years (range, 20 to 95; SD, 13.9) in the remainder of the patients with CRVO ( P < .001). There was no gender predilection for the development of paracentral acute middle maculopathy (males, 48%; females, 52%).
| Age, years | |
| Mean ± SD | 51 ± 16.6 |
| Range | 19–78 |
| Gender (n = 25) | |
| Male | 12 (48%) |
| Female | 13 (52%) |
| Eye (n = 25) | |
| Right | 12 (48%) |
| Left | 13 (52%) |
| CRVO Type (n = 25) | |
| Nonischemic | 25 (100%) |
| Ischemic | 0 (0%) |
| Systemic/ocular associations | |
| Hypertension | 8 (32%) |
| Hypercholesterolemia | 6 (24%) |
| Diabetes mellitus | 4 (16%) |
| SLE | 3 (12%) |
| Open-angle glaucoma | 3 (12%) |
| OCP use | 2 (8%) |
| Marathon running | 1 (4%) |
| MGUS | 1 (4%) |
| BCVA | |
| Snellen mean | 20/120 |
| Snellen range | 20/20-HM |
| logMAR mean | 0.767 |
| logMAR range | 0–2.28 |
With respect to pre-existing systemic and ocular comorbidities, 8 patients had known histories of hypertension, 6 had hypercholesterolemia, 4 had diabetes mellitus, 3 had systemic lupus erythematosus, 3 had open-angle glaucoma with optic disc cupping, and 1 had active pulmonary tuberculosis who was undergoing treatment. After detailed histories were obtained, 2 patients endorsed current use of oral contraceptive pills, and 1 individual was a long-distance marathon runner. Hematologic laboratory workup, when obtained, was negative for any hypercoagulable state in all but 1 case, in which an underlying diagnosis of monoclonal gammopathy of undetermined significance was uncovered.
Patients typically presented with subjective central visual deficits that began, on average, 8.3 days prior to office evaluation (range, 1–21 days). Complaints ranged from generalized blurring of the central vision and difficulty focusing to more specific patterns of paracentral scotomas, including the following patient descriptions: “pieces of central vision missing” ( Figure 1 ); “concentrically arranged fixed gray spots”; “like looking through cracked glass”; “numerous small blind spots”; and “blank spots in central vision.” On initial examination, Snellen best-corrected visual acuity (BCVA) ranged from 20/20 to hand motions, with an average of 20/120 (logarithm of minimal angle of resolution [logMAR] equivalent, 0.76). The vast majority of eyes demonstrated good initial acuity, with 14 (56%) of 25 patients presenting with BCVA of 20/50 or better; however, 8 (32%) of 25 had vision of 20/200 or worse, all of which were noted to have concurrent cilioretinal artery occlusion ( Figure 2 ). Altogether, simultaneous cilioretinal artery occlusion was a common occurrence in our cohort (10 (40%) of 25 patients), and their mean BCVA of 20/800 (logMAR equivalent, 1.60) was significantly lower than the 20/40 (logMAR equivalent: 0.26) for noncilioretinal artery occlusion patients ( P < .001).
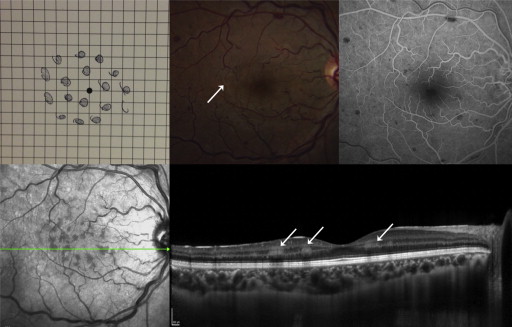
The diagnosis of CRVO was established on the basis of characteristic funduscopic findings: tortuosity and dilatation of the central retinal vein, intraretinal hemorrhages throughout all 4 quadrants, and/or optic disc and macular edema. In all eyes, detailed examination of the macula in the involved eye revealed patchy areas of deep retinal whitening centered within the macula, often in the distribution of the venous tributaries and always correlating with paracentral acute middle maculopathy on spectral-domain OCT ( Figures 1–6 ). Compared to cotton-wool spots, the retinal whitening associated with paracentral acute middle maculopathy was noticeably distinct, appearing as a duller gray-white in color, less opaque, deeper in the retina, and not following the distribution of the nerve fiber layer ( Figure 3 ). Similarly, the lesions of paracentral acute middle maculopathy were uniquely different in appearance and location from associated cilioretinal artery occlusion, when present ( Figure 2 ), which was more superficial and whiter.
Because of the presence of concurrent retinal hemorrhages and cotton-wool spots, the extent of paracentral acute middle maculopathy was not always as readily apparent on examination; however, with ancillary red-free photography ( Figure 4 ) and near-infrared reflectance imaging ( Figures 1–6 ), the lesions were more clearly identified, appearing dark and more precisely delineated. Specifically, near-infrared reflectance confirmed the perivenular location of paracentral acute middle maculopathy in the majority of cases. Conversely, the fluorescein angiogram had no correlation with the lesions ( Figure 1 and Figure 4 ), and no cases displayed angiographic evidence of an ischemic CRVO (10 or greater disc diameters of capillary nonperfusion).
Corresponding spectral-domain OCT imaging registered through the zones of retinal whitening revealed multifocal hyper-reflective plaquelike lesions at the level of the inner nuclear layer ( Figures 1–6 ). In 13 cases, the involvement of paracentral acute middle maculopathy was additionally noted to extend into the inner plexiform layer. Although the lesions appeared to cast a shadow over the deeper retinal layers, they spared the ellipsoid and interdigitation bands, which were always intact by spectral-domain OCT. Associated macular edema was an uncommon finding, noted in the spectral-domain OCT scans of only 5 (20%) of 25 patients.
Mean duration of follow-up was 7.2 months (range, 1–24; median, 4; SD, 7.6), although 8 of the 25 patients were lost to follow-up. Average final BCVA at the most recent clinic visit was 20/40 (logMAR equivalent, 0.339) for the entire cohort. More specifically, patients with simultaneous cilioretinal artery occlusion experienced partial resolution of vision back to an average BCVA of 20/120 (logMAR equivalent, 0.81), compared to 20/30 (logMAR equivalent, 0.20) in the noncilioretinal artery occlusion patients ( P = 0.26). Although 14 (82%) of the 17 patients tested 20/50 or better at the final visit, the subjective paracentral scotomas persisted.
On fundus examination, intraretinal hemorrhages, optic disc edema and macular edema showed variable degrees of resolution. On follow-up near-infrared reflectance imaging, the dark lesions had dissipated, and the most recent spectral-domain OCT examinations revealed zones of severe inner nuclear layer thinning and a markedly attenuated outer plexiform layer band where the hyper-reflective paracentral acute middle maculopathy lesions had been located previously ( Figure 5 and Figure 6 ). The shadowing induced by the overlying lesions seen on spectral-domain OCT had resolved.
Of the patients, 5 had received serial intravitreal antivascular endothelial growth factor therapy during their courses (2 with bevacizumab, 3 with ranibizumab) for treatment of associated macular edema. Whether a patient received intravitreal injections did not appear to impact the timeline to resolution of the paracentral acute middle maculopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


