Purpose
To investigate the surgical outcome of rectangular 4-snip punctoplasty, a modification of rectangular 3-snip procedures, using objective measurements.
Design
Noncomparative case series.
Methods
The medical charts of patients who underwent rectangular 4-snip punctoplasty for severe punctal stenosis with at least 6 months follow-up were reviewed. Before surgery and at 1 and 6 months after surgery, subjective evaluation of tearing was assessed using Munk scores. The size of the punctum was graded based on slit-lamp examination, and measurement of tear meniscus height was done using Fourier-domain optical coherence tomography.
Results
A total of 45 eyes (26 patients) were studied. The subjective epiphora score was significantly reduced after surgery and maintained until 6 months after the surgery (χ 2 for trend test, P < .001). The grade of the punctum size was also significantly enlarged after surgery and the enlarged punctum was maintained until 6 months after the surgery (χ 2 for trend test, P < .001). The mean preoperative tear height (452.4 ± 249.3 μm) was significantly reduced both at 1 month after surgery (341.6 ± 207.9 μm; P = .003, paired t test) and at 6 months after surgery (362.1 ± 212.6 μm; P = .004, paired t test). The functional success rate was 93.3% and anatomic success rate was 88.9% at 6 months after surgery.
Conclusions
Rectangular 4-snip punctoplasty was an anatomically and functionally effective procedure for severe punctal stenosis patients, maintaining large puncta for fairly long periods.
Punctal stenosis can be easily treated by punctoplasty, namely the snip procedures. The surgery for stenosis involves a 1-, 2-, or 3-snip punctoplasty. There are debates as to the number of cuts or the direction of the snip(s) that is best to prevent recurrence of epiphora and achieve anatomic and functional success. The 1-snip procedure refers to a single vertical snip down to the ampulla, which produces a high rate of failure attributable to reapproximation of the adjacent raw cut ends. To solve this problem, a 2-snip variation of the surgery was suggested by Jones. This procedure consists of removing a V-shaped wedge from the vertical portion of the canaliculus on the conjunctival surface.
More recently, the 3-snip procedure has become more widely adopted than the 1-snip or 2-snip procedure. The traditional 3-snip, specifically the triangular 3-snip procedure, is a posterior ampullectomy, which removes the triangular-shaped ampulla by a first cut at the vertical canaliculus, followed by a second cut along the horizontal canaliculus and a final snip at the base. A rectangular 3-snip punctoplasty, which involves 2 vertical snips at either side of the ampulla and a cut at the base, was recently reported to have high functional and anatomic success rates. The higher success rates are thought to be attributable to the preservation of physiology, as only the vertical portion of posterior ampulla is excised, and the anatomy and physiological functions of the lacrimal system are preserved.
At our institute, we have performed the traditional triangular 3-snip procedure and experienced relatively high rates of reapproximation, which led to more recent adoption of rectangular 3-snip punctoplasty. However, we observed that in cases of severe punctal stenosis, the punctum could not be sufficiently dilated to allow 2 vertical cuts. In addition, the size of the rectangular punctum left by this procedure was not large enough to resolve the epiphora found in severe stenotic cases.
Therefore, we modified the rectangular 3-snip procedure to create a rectangular 4-snip to maximize the punctum size, and prevent re-stenosis in cases of severe punctal stenosis. This procedure includes a small portion of the horizontal canaliculus in the rectangular flap. In this study, we retrospectively reviewed the outcomes of this new procedure.
Methods
The medical charts of the patients who underwent rectangular 4-snip procedure for severe punctal stenosis between February and September 2010 at Severance Hospital, Yonsei University College of Medicine were reviewed. To be included in the study, a patient must have had epiphora and severe stenosis of the lower eyelid puncta and/or the upper lid puncta. In those patients, the punctal dilation was performed with a punctal dilator but was not sufficient to allow the 2 vertical cuts to the ampulla. The patency of the canaliculi and nasolacrimal duct was confirmed by probing and irrigation. Patients with other causes of epiphora, such as canalicular stenosis, nasolacrimal duct obstruction, punctal malposition, lid laxity, entropion, and ectropion, were excluded. A minimum follow-up of 6 months was required for inclusion in this study.
All surgical procedures were performed by the same surgeon (J.S.Y.). Local injection of 0.3 cc of 2% lidocaine with 1:100 000 epinephrine was administered transconjunctivally, below the punctum. A pair of small spring scissors was subsequently used to make a first vertical cut down to the ampulla and a second horizontal cut (approximately 2 mm) along the roof of the canaliculus, followed by a third vertical cut from the edge of the second or a horizontal cut from the edge of the first cut to create a flap. Finally, removal of the base of the flap was performed ( Figure 1 ) . Topical antibiotics and steroids were given for 1 week postoperatively.

A subjective evaluation of tearing was done using Munk score ( Table 1 ), and the size of the punctum was visually graded based on the slit-lamp examination ( Table 2 ) prior to surgery and at 1 and 6 months post-surgery.
| Grade | Clinical Finding |
|---|---|
| 0 | No epiphora |
| 1 | Occasional epiphora requiring wiping with a tissue or handkerchief less than twice a day (<2) |
| 2 | Epiphora requiring 2 to 4 wipings per day |
| 3 | Epiphora requiring 5 to 10 wipings per day |
| 4 | Epiphora requiring >10 wipings per day or continuous tearing |
| Grade | Clinical Finding |
|---|---|
| 0 | No papilla and punctum (punctal atresia) |
| 1 | Papilla is covered by a membrane or fibrosis and difficult to recognize |
| 2 | Less than normal size but recognizable |
| 3 | Normal |
| 4 | Small slit (<2 mm) |
| 5 | Large slit (≥2 mm) |
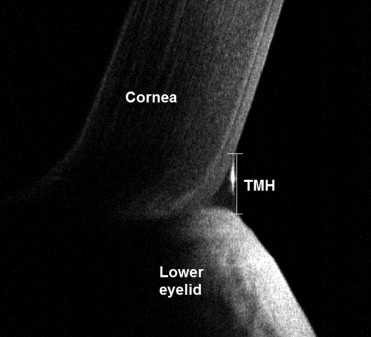
An objective analysis of tear meniscus height was performed using Fourier-domain optical coherence tomography (FD-OCT) (RTVue; Optovue Inc, Fremont, California, USA), before and at 1 and 6 months after surgery ( Figure 2 ) . We performed a vertical 2-mm scan across the lower tear meniscus below the center of the cornea at the 6-o’clock position. The tear meniscus height (TMH) was measured with a computer caliper.
Anatomic success was defined as a punctal opening grade of 3 (normal size of punctum), 4 (<2 mm slit punctum), or 5 (≥2 mm slit punctum). Functional success was defined as Munk score 0 (no epiphora) or 1 (occasional epiphora requiring <2 wipings per day).
For statistical analysis, χ 2 for trend tests and paired t tests were used where appropriate. Data were analyzed using SPSS version 18.0 (SPSS Inc, Chicago, Illinois, USA).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


