Purpose
To report optical coherence tomography (OCT) features of patients with autoimmune retinopathy.
Design
Consecutive case series.
Method
Eight patients who presented with unexplained loss of central vision, visual field defects, and/or photopsia were diagnosed with autoimmune retinopathy based on clinical features, electroretinogram (ERG) findings, and serum antiretinal antibody analysis. All patients underwent OCT testing of the macula and nerve fiber layer (NFL).
Results
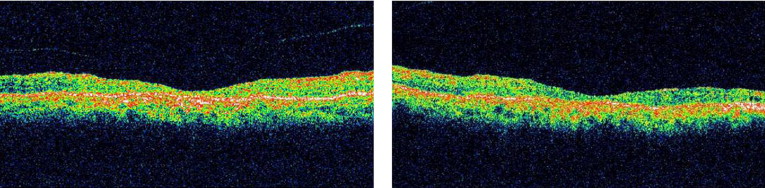
Outer retinal abnormalities and/or decreased macular thickness on OCT were seen in all patients. Macular OCT showed reduced central macular and foveal thicknesses in 6 patients (mean thickness 143 ± 30 μm and 131 ± 29 μm respectively). In all but 1 patient, loss of the photoreceptor layer or disruption of the photoreceptor outer and inner segment junction was noted. Three patients showed only mild to moderate focal NFL loss.
Conclusions
Retinal atrophy and reduced macular thickness on OCT are predominant features in patients with autoimmune retinopathy. OCT provides objective measures of retinal damage and may offer clues toward understanding the mechanism of visual dysfunction and the diagnosis of autoimmune retinopathy.
Autoimmune- and cancer-associated retinopathy represent an important cause of otherwise unexplained acute or subacute vision loss in adults. These forms of retinal disease result from a presumed immunologic process affecting the retina by autoantibodies directed against retinal antigens. Acquired immunologically mediated retinal degeneration in the absence of an underlying malignancy is commonly referred to as autoimmune retinopathy, while the term cancer-associated retinopathy is reserved for similar processes but with an associated malignancy at the time of initial evaluation. Autoantibodies against multiple retinal antigens including recoverin, α-enolase, heat-shock proteins, arrestin, transducin, neurofilament protein, carbonic anhydrase II, and TULP1 have been reported in sera of patients with autoimmune- and cancer-associated retinopathy. Patients may describe symptoms such as decreased vision, photopsias, decreased night vision, abnormal color vision, and visual field defects. As fundus evaluation may initially be normal, the diagnosis may be challenging, and ancillary testing including electroretinography (ERG) and serum antibody analysis are helpful in establishing the diagnosis. ERG is typically markedly reduced in amplitude, even in the early stages. However, in some cases the pathology may be limited to central cone abnormalities that may only be recognized using multifocal ERG testing.
We believe that optical coherence tomography (OCT) is helpful in the diagnosis and determination of prognosis in patients with autoimmune- and cancer-associated retinopathy. In addition, OCT may offer clues towards understanding the mechanism of visual dysfunction in these patients.
Methods
We analyzed a consecutive case series of 8 patients with newly diagnosed autoimmune retinopathy. All patients were seen in the department of ophthalmology at the University of Virginia. The diagnosis was based on a detailed ophthalmic examination, automated visual field testing, ERG evaluation, and serum antiretinal antibody detection. Blood samples were collected from all patients and sent to the Ocular Immunology Laboratory (Oregon Health and Science University, Portland, Oregon) for evaluation of antiretinal autoantibodies. Antibody testing was performed using previously described techniques that employed Western blot analysis using proteins extracted from human retinas and immunohistochemistry. Following initial screening test, when the serum was suspected to react with known retinal proteins, a separate confirmatory experiment was performed whereby the serum was again incubated with the purified protein on a blot. Many antiretinal autoantibodies have been previously described that may or may not be associated with cancer. The most frequent of those include antibodies against retinal α-enolase (46 kDa), recoverin (23 kDa), and p35 (35 kDa) that predominantly affect photoreceptors, but can also affect bipolar cells and retinal ganglion cells. In this study the antiretinal antibodies tested included antibodies against these 3 retinal antigens as well as antibodies against carbonic anhydrase II (30 kDa), rhodopsin (40 kDa), arrestin (48 kDa), and phosphodiesterase (PDE; 88 kDa). Other less frequently encountered autoantibodies such as antibodies against neurofilament proteins, heat-shock protein 70, TULP1 protein, 40-kDa insoluble protein, transducin-alpha, interphotoreceptor retinoid-binding protein (IRBP), and other retinal proteins of unknown identity were also tested. Additionally, autoantibodies against bipolar cells such as those seen in melanoma-associated retinopathy (MAR) syndrome were tested.
OCT of the macula and nerve fiber layer (NFL) was performed on all of these patients using a fourth-generation Zeiss Stratus OCT (Carl Zeiss Ophthalmic Systems, Dublin, California, USA), which was the most recent OCT version commercially available at the time of initiation of the study. All 6 high-definition radial line scans of the macular OCT imaging as well as all 3 scans of the NFL OCT for each patient were reviewed and analyzed for reliability of thickness measurements. Only reliable scans, according to previously reported guidelines, were included. Quantitative data are presented as mean ± standard deviation.
Patients were offered treatment with oral prednisone and subsequently intravenous immunoglobulin (IVIG) 400 mg/kg for 5 consecutive days every month for 3 months. Treatment was repeated only in case of documented improvement of antiretinal antibody titers and visual function (as indicated by visual acuity, visual fields, and ERG) measured 2 to 4 weeks after initial treatment.
Results
Seven women and 1 man, with a mean age of 59 ± 15 years, were included in the study ( Table ). In all patients a complete ophthalmic, medical, and family history failed to suggest hereditary forms of retinal degeneration or inflammatory retinal disease. The clinical, electrophysiological, laboratory, and OCT findings are summarized in the Table . Best-corrected visual acuity at presentation ranged from 20/20 to 1/200 E (defined as the ability to see the 20/200 “E” Snellen optotype at a distance of 1 foot). All 8 patients tested positive for serum antiretinal autoantibodies. Two patients had a history of malignancy: ovarian cancer in 1 patient and non-Hodgkin lymphoma as well as breast cancer in the other. The malignancies had been diagnosed years prior to presentation. Three patients had associated systemic autoimmune diseases (rheumatoid arthritis, Graves disease, systemic lupus erythematosus, and antiphospholipid antibody syndrome).
| Patient # (Age, Sex) | Presenting Symptoms | BCVA at Presentation | Fundus Findings | Serum Antiretinal Antibodies | ERG | Macular OCT Findings/Central Macular Thickness | Nerve Fiber Layer Thickness | Associated Autoimmune Disease/Malignancy |
|---|---|---|---|---|---|---|---|---|
| 1 (85, M) | Progressive loss of vision from 20/60 and 20/25 over 1 year, poor peripheral vision, photopsia | HM OD 20/70 OS | Mild optic nerve head pallor, attenuated vessels, pigment clumping in macula |
| Extinguished rod and cone responses |
| Unremarkable | RA |
| 2 (51, F) | Progressive loss of vision over 2 years, photopsia | 20/200 OU | Old PRP & focal laser, regressed PDR, attenuated vessels | 46 kDa (α-enolase) | Extinguished rod and cone responses |
| Moderate thinning inferiorly OD | None |
| 3 (54, F) | Progressive loss of vision over 1 year | 20/20- OU | Unremarkable | 30 kDa (carbonic anhydrase), 33 kDa | Normal rod, increased implicit time on cone responses |
| Mild thinning temporally OU | Lymphoma, breast cancer, cryoglobulinemia, hepatitis C |
| 4 (70, F) | Rapid decline in acuity from 20/30 over 4 months | 20/200 OU |
| 145 kDa (IRBP) | Not available |
| Unremarkable | SLE, antiphospholipid antibody syndrome |
| 5 (69, F) | Rapid decline in acuity from 20/40 over 3 months |
| Unremarkable | 46 kDa (α-enolase) | Normal rod, significantly reduced cone responses |
| Unremarkable | None |
| 6 (49, F) | Central visual loss over 6 months | 6/200 E OU | Unremarkable | 35-36 kDa and 44 kDa | Delayed and significantly reduced cone and rod responses |
| Unremarkable | None |
| 7 (78, F) | Decreased vision over 6-8 months, photopsia | 20/70 OU | Attenuated vessel, scattered RPE changes OU | 50 kDa, 62 kDa, and 67 kDa | Extinguished rod and cone responses |
| Moderate thinning inferiorly OD; moderate thinning superiorly & inferiorly OS |
|
| 8 (40, F) | Decreased acuity over 2 months, severely affected visual field on Humphrey 24-2 and 10-2 testing, photopsia OD only |
| Bilateral hypopigmentation of inferior retina | 40 kDa | Normal rod and cone responses on full-field ERG; reduced macular response OD on multifocal ERG |
| Unremarkable |
|
Outer retinal abnormalities and/or decreased macular thickness on OCT were seen in all of the patients. Macular OCT showed reduced central macular and foveal thicknesses in 6 patients (mean thickness 143 ± 30 mm and 131 ± 29 mm respectively). There was no significant difference in central macular thickness measurements between the right and left eyes ( P value = .14). In the other 2 patients the mean central macular and foveal thicknesses were not decreased and measured 244 ± 36 and 223 ± 36 mm respectively. In all but 1 patient (Patient 3) loss of the photoreceptor layer ( Figure 1 ) or disruption of the photoreceptor outer and inner segment (OS/IS) junction ( Figure 2 ) was noted on macular OCT. OCT of the NFL was largely unremarkable in all patients, with only mild to moderate focal NFL loss in 3 patients.