Purpose
To report 3 cases of myiasis with a singular subretinal track in the Northeastern part of United States.
Design
Noninterventional case series.
Methods
Three patients from Pennsylvania were referred for evaluation of a linear and serpiginous retinal scar. Funduscopic examination and fluorescein angiography were performed to assess the referred retinal lesion.
Results
Funduscopic examination showed a singular subretinal track from the superior periphery to either the posterior pole or inferior midperiphery in the study cases. Fluorescein angiography showed exudative retinal detachment in all 3 cases. Laser photocoagulation of the subretinal worm was performed in all reported cases.
Conclusions
Our case series represents a report of singular subretinal tracks presumably caused by the warble fly larva in the Northeastern part of United States.
Myiasis is an animal or human condition initiated by parasitic dipterous fly larvae feeding in the host’s necrotic or living tissue. Human myiasis can present with cutaneous, systemic, or ophthalmic manifestations. Ophthalmic myiasis or ophthalmomyiasis is classified as either externa and interna. Ophthalmomyiasis externa is restricted to the external ocular structures, such as the eyelid and conjunctival sac, and interna is characterized by myiasis larva in the anterior or posterior segments of the eye. The precise mechanism for ophthalmomyiasis infection in humans is not clearly understood. Eyelashes and eyebrows are considered likely oviposition targets ; the human scalp hair is probably the preferential site in humans on the basis of experimental models of study. Transfer of the larvae straight from the guard hairs of caribou and other hosts to the human skin or eye is another possible explanation. The parasite does not seem to finalize its life cycle in humans, which means that humans are an intermediate host of myiasis.
In its classic clinical presentation, posterior ophthalmomyiasis interna is characterized by pigmented and atrophic retinal pigment epithelium (RPE) tracts in a criss-crossing pattern seen in conjunction with hemorrhages, fibrovascular proliferation, exudative detachment of the retina, and even fibrovascular scarring. We report 3 cases of presumed ophthalmomyiasis with a singular curvilinear subretinal track seen in patients in the northeastern part of the United States.
Case Reports
Case 1
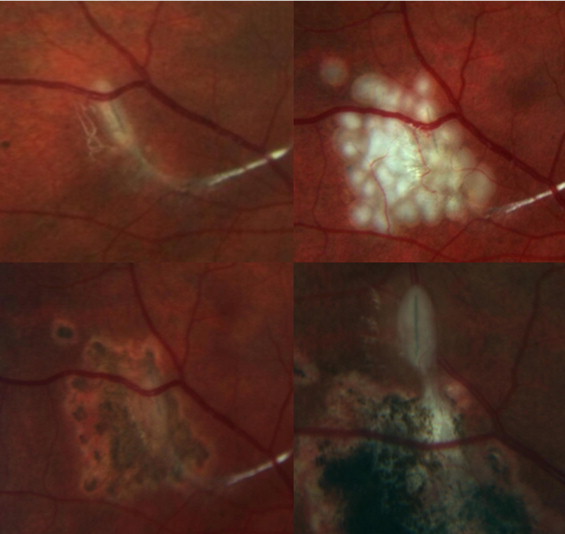
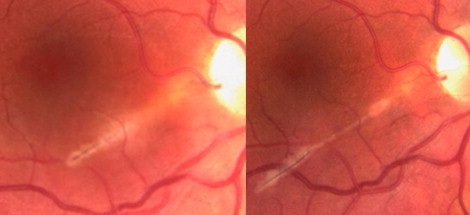
An asymptomatic 10-year-old myopic girl from Pittsburgh, Pennsylvania, was referred for evaluation of a retinal scar in the right eye. The patient and her mother reported no ocular trauma. The family frequently visited a cabin in a wooded area of western Pennsylvania, but had no other significant travel history. The patient and mother reported no history of ingestion of undercooked meat or any recent tick bites. The family had a pet dog, but no other household pets. There was no family history of eye disease. On examination, visual acuity was 20/20 in both eyes with correction. External examination and anterior segment examination results were within normal limits, with quiet anterior chambers and clear crystalline lenses. Funduscopic examination of the right eye revealed a linear, curvilinear, white, subretinal scar extending from the supertemporal periphery to the inferotemporal midperiphery. A pigmented, dome-shaped elevation with surrounding RPE atrophy also was noted temporal to the macula, suggestive of previous choroidal neovascularization. The inferotemporal edge of the scar demonstrated a focal area of inflammation surrounding a subretinal lesion, with a black line on its surface adjacent to a silver, hairpin-shaped lesion ( Figure 1 ). No disc edema was noted. Examination of the left eye was within normal limits. On follow-up examination 3 days later, a conformational change to the silver lesion was noted inferotemporally, consistent with a larval infection. Fundus photographs were repeated 15 minutes later and demonstrated further interval change in the appearance of the organism indicative of larval movement. Laser photocoagulation of the presumed subretinal larva at the slit lamp subsequently was performed with obliteration of the suspected organism. However, 4 months later, the larva moved beyond the laser photocoagulation scar ( Figure 2 ). Her follow-up visual acuity remained 20/20.

Case 2
A 33-year-old white female from Williamsport, Pennsylvania, was referred for evaluation of a subretinal lesion in the right eye. The patient had a history of being around several animals such as goats, chickens, cats, dogs, ducks, and horses. She also was around deer and wild turkeys, which are typical wild animals indigenous to Pennsylvania. In addition, she had a history of drinking unprocessed milk. The patient had no history of traveling outside the region of central Pennsylvania. She reported no history of recent tick bites or ingestion of undercooked meat. The patient did not have any other systemic manifestations. There was no family history of eye disease. The patient did not report any history of ocular trauma. On examination, visual acuity was 20/400 in the right eye and 20/20 in the left eye with correction. External examination and anterior segment examination were within normal limits. Funduscopic examination of the right eye revealed a linear, short, white subretinal lesion with a black line on its surface extending from the temporal boundary of the optic disc to the inferotemporal macular area. Fluorescein angiography showed progressive hyperfluorescence at the subretinal lesion location corresponding to a pooling of the fluorescein dye. No disc edema was noted. Examination results of the left eye were within normal limits. A diagnosis of idiopathic choroidal neovascularization was made, and the patient was treated with 2 intravitreal injections of bevacizumab; visual acuity returned to 20/20 in the right eye. On follow-up examination 2 months later, there was a progression of the subretinal lesion with a subretinal tract toward the inferotemporal macular area suggestive of a larval infection ( Figure 3 ). Laser photocoagulation of the presumed subretinal larva was performed. Her follow-up visual acuity remained 20/20.
Case 3
A 23-year-old female from Pittsburgh, Pennsylvania, was referred for evaluation of a retinal scar in the left eye. She did not report a history of ocular trauma, travel outside the United States, or family history of eye disease. Also, there was no history of tick bites or undercooked meat ingestion. The patient had a history of being around domestic animals such as cats and dogs. On examination, visual acuity was 20/20 in the right eye and 20/25 in the left eye with correction. External examination and anterior segment examination results were unremarkable. Funduscopic examination of the left eye revealed a linear and curvilinear subretinal scar extending from the supertemporal periphery to the inferotemporal posterior pole with a presumed larva at the end of the subretinal track. Laser photocoagulation of the presumed subretinal larva was performed. Examination results of the right eye were within normal limits. After a 3-month quiescent interval, a dome-shaped elevation was noted temporal to the macula, corresponding to an exudative macular detachment ( Figure 4 ). Her follow-up visual acuity remained 20/20.





