Ophthalmologic Laboratory and Diagnostic Tests
Selected Laboratory Tests in Ocular Disease
Laurance Freier
SELECTED LABORATORY TESTS IN OCULAR DISEASE
This section lists suggested laboratory and diagnostic tests for ocular disorders and systemic diseases that may have ophthalmic manifestations. These lists are not meant to be exhaustive, nor should every test listed be done in every case. In general, diagnostic tests are ordered only when their results will have a direct bearing on the management of the patient.
For the abbreviations of tests used in the lists, see Chapter 2, “Common Laboratory Tests and Procedures.” Asterisks (*) indicate a nonspecific, initial group of tests. If the patient’s history, signs, or symptoms suggest a particular etiology, additional tests should be done as indicated. See tests listed under individual etiologies. For systemic diseases associated with anterior uveitis, see Table 3-1.
Acanthamoeba
Gram stain
Giemsa stain (to help distinguish from herpes simplex)
Calcofluor white stain
Culture: Nonnutrient agar with Escherichia coli overlay
Confocal microscopy
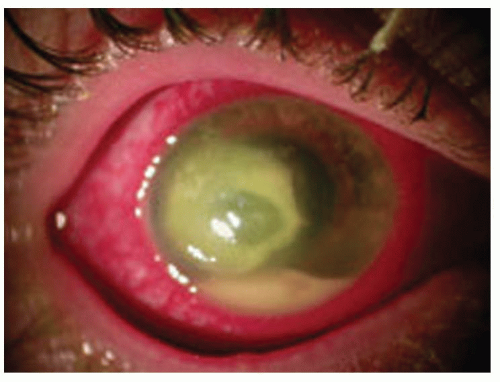
Acute Retinal Necrosis
Complete blood count (CBC) with differential
Erythrocyte sedimentation rate (ESR)
Rapid plasma reagin (RPR) and fluorescent treponemal antibodyabsorption (FTA-ABS)
Chest x-ray
Purified protein derivative (PPD) with anergy panel
Computed tomography (CT) scan of the orbit or B-scan ultrasound (to check for an enlarged optic nerve)
Consider a fluorescein angiogram
Consider urine studies for cytomegalovirus (especially if patient is immunocompromised)
Consider toxoplasmosis enzyme-linked immunosorbent assay (ELISA) and serum titers for herpes simplex and varicella zoster
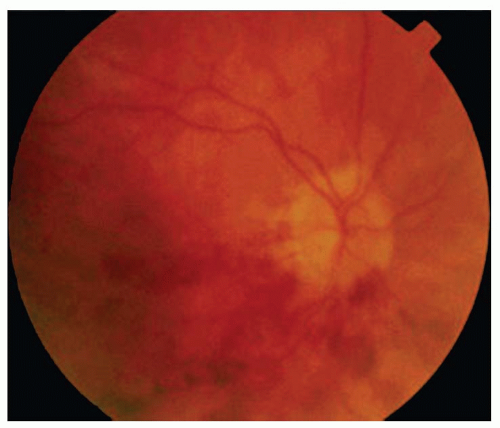
Human immunodeficiency virus (HIV) test if patient is from a high-risk group for acquired immunodeficiency syndrome (AIDS) (Fig. 3-3)
TABLE 3-1 Systemic Diseases Associated with Anterior Uveitis | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Amaurosis Fugax
Immediate ESR, Westergren method (if giant cell arteritis [GCA] is suspected)
Fasting blood sugar (FBS) and glucose tolerance test (GTT) (to rule out diabetes)
CBC with differential and platelet count (to rule out polycythemia and thrombocytosis)
Lipid profile (to rule out hyperlipidemia)
Serum cholesterol
Hemoglobin, Hct
Carotid artery evaluation (duplex scan-Doppler and ultrasound)
Two-dimensional echocardiogram
Holter monitor
ECG
Digital subtraction angiogram
CT scan or magnetic resonance imaging (MRI)
Carotid arteriogram (only if carotid surgery is planned)
Consider a fluorescein angiogram (may show focal staining at the site of the embolus)
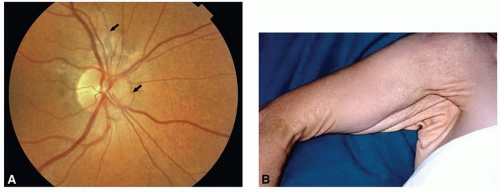
Angioid Streaks
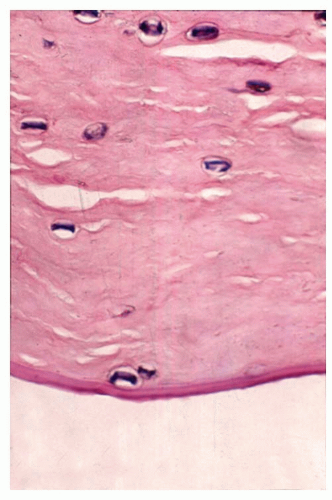
Skin biopsy (if pseudoxanthoma elasticum is suspected)
Cardiovascular exam to rule out aortic aneurysm
Skull x-ray to rule out Paget’s disease
Serum alkaline phosphatase and urine calcium level if Paget’s disease is suspected
Sickle cell prep and hemoglobin electrophoresis (to rule out homozygous sickle cell disease) if patient is black or has Mediterranean background
PO4 levels (to rule out hyperphosphatemia)
Fluorescein angiogram to check for neovascular membrane (Fig. 3-4A,B)
Aniridia
Consider renal ultrasound (if Wilms tumor is suspected)
Consider intravenous pyelography (if ultrasound suggests possibility of Wilms tumor)
Consider chromosomal karyotype (deletion of the short arm of chromosome II suggests an increased chance of a Wilms tumor)
Anisocoria (Pharmacologic Tests)
Greater in light or dark (nonbenign)
Light (abnormal large pupilparasympathetic lesion)
Weak pilocarpine test (1/16% to 0.0625%): Adies tonic pupil
Strong pilocarpine test (1%): Pharmacologic versus neurologic pupil
Dark (abnormal small pupil-sympathetic lesion)
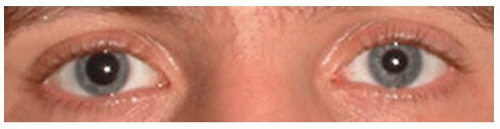
Aproclonidine 1%: Differentiate second versus third neuron lesion (Fig. 3-5)
Ankylosing Spondylitis
Men: x-ray of sacroiliac joints; CT scan
Women: x-ray of shoulders
ESR
HLA-B27
Anterior Uveitis; Iritis/Iridocyclitis*
Antinuclear antibody (ANA)
CBC
ESR
RPR or Venereal Disease Research Laboratory (VDRL) and FTA-ABS
Chest x-ray (to rule out sarcoidosis and tuberculosis)
PPD and anergy panel
In endemic areas, lab tests for Lyme’s disease
Arcus Senilis (in a Patient <50 Years Old)
Serum cholesterol
Lipoprotein electrophoresis
Serum triglycerides (to rule out type II or V hyperlipoproteinemia)
FBS (to rule out adult onset diabetes mellitus) (Fig. 3-6)
Argyll Robertson Pupil
RPR or VDRL
FTA-ABS or microhemagglutination assay for triponema pallidium (MHATP)
Consider a lumbar puncture (if diagnosis of syphilis is established)
Band Keratopathy
Albumin
Blood urea nitrogen (BUN)
Creatinine
Magnesium
Phosphorus level
Serum calcium
Uric acid level (if gout is suspected)
ANA, ESR, rheumatoid factor (RF), x-rays of the knees (if juvenile rheumatoid arthritis [JRA] is suspected)
Other tests directed toward a specific, suspected etiology (e.g., sarcoidosis)
Behçet’s Disease
Behçet’s skin puncture test
HLA-B27 or HLA-B5
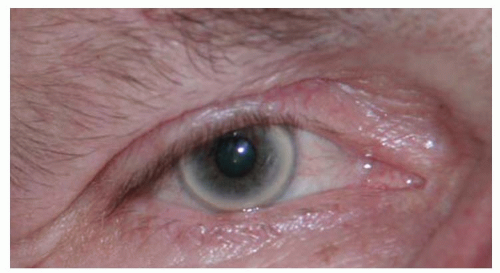
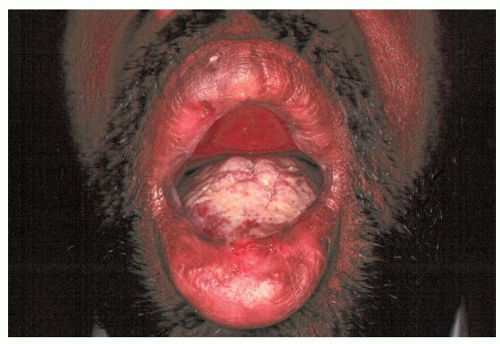
Medicine or rheumatology consult (Fig. 3-7)
Blind Infant
Electro-retinagram (ERG)
Visual-evoked potential (VEP)
Consider a CT scan and/or MRI of the brain
Blow-Out Fracture of the Orbit
CT scan (axial and coronal views) of the orbits and brain if surgery is planned or if the diagnosis is uncertain
Branch Retinal Artery Occlusion
Carotid artery evaluation (Doppler and ultrasound)
FBS (3-hour GTT if findings are negative)
Immediate ESR, Westergren method (to rule out GCA if patient is >55 years old)
Greater superficial temporal artery biopsy if GCA is suspected because of symptoms or ESR findings
Echocardiogram
Holter monitor
Blood tests: ANA, CBC with differential and platelets, FTA-ABS, lipid profile, prothrombin time (PT) or partial thromboplastin time (PTT), and RF
Hct and hemoglobin electrophoresis
Serum protein electrophoresis (Fig. 3-8)
Branch Retinal Vein Occlusion (BRVO)
FBS
CBC with differential and platelets
ANA
ESR
PT or PTT
RF
Fluorescein angiogram
Chest x-ray
Internal medicine consult (to check for cardiovascular disease) (Fig. 3-9)
Canaliculitis
Cultures of material expressed from the punctum
Blood agar
Chocolate agar
Sabouraud’s medium
Thioglycolate broth
Gram stain
Giemsa stain
Candidiasis
BUN
CBC
Creatinine
Liver function tests (see list under “Postoperative Endophthalmitis”)
Blood and urine cultures for Candida
Vitreous cultures (when there is a significant amount of vitreous involvement) can be used to confirm a diagnosis and to test sensitivity to antifungal agents
Consider HIV tests
Cavernous Sinus Syndrome: Multiple Ocular Motor Palsies
CT scan (axial and coronal views) or MRI of the brain, orbit, and sinuses
If the CT scan and MRI are normal, consider the following:
ANA, CBC with differential, ESR, and RF (to rule out infection, malignancy, or a systemic vasculitis)
A blind nasopharyngeal biopsy (to rule out a nasopharyngeal carcinoma)
Chest x-ray
Lumbar puncture (three times; to rule out carcinomatous meningitis)
Lymph node biopsy (if a lymphadenopathy is present)
A repeat CT scan or MRI if the cavernous sinus was not well visualized
A cerebral arteriogram to rule out an aneurysm or arteriovenous fistula (but these are usually seen on the CT scan)
Blood cultures (three times) plus a culture of the presumed primary source of infection if a cavernous thrombosis is suspected
Central Retinal Artery Occlusion
Immediate ESR, Westergren method (to rule out GCA if patient is >55 years old)
Greater superficial temporal artery biopsy if GCA is suspected because of symptoms or ESR findings
Carotid artery evaluation (Doppler and ultrasound)
FBS (3-hour GTT if findings are negative)
Echocardiogram
Holter monitor
Blood tests: ANA, CBC with differential and platelets, lipid profile, FTA-ABS, PT or PTT, and RF
Hct and hemoglobin electrophoresis
Serum protein electrophoresis
Consider ERG or fluorescein angiogram to help confirm diagnosis
Central Retinal Vein Occlusion (CRVO)
CBC with differential and platelets
FBS
Lipid profile
VDRL and FTA-ABS
Serum protein electrophoresis
ANA
Cryoglobulins
ESR
Hemoglobin electrophoresis
PT or PTT
Fluorescein angiogram (to rule out diabetic retinopathy)
Ophthalmodynamometry or oculopneumoplethysmography (to help distinguish a CRVO from carotid artery disease; ophthalmic artery pressure is usually normal or elevated in a CRVO but is usually low in carotid disease)
Chest x-ray (to rule out an underlying medical problem)
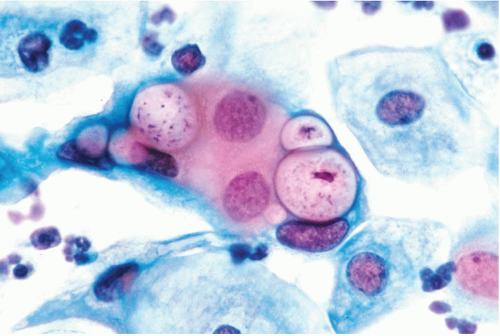
Chlamydial Inclusion Conjunctivitis
Giemsa stain of conjunctival scraping (will show inclusion bodies within epithelial cells, lymphocytes, and polymorphonuclear leukocytes)
Chlamydial immunofluorescence test
Detection of Chlamydia antigen (enzyme immunoassay [EIA], direct fluorescent antibody [DFA]) or DNA (Fig. 3-10)
Choroidal Detachment
B-scan ultrasonography if melanoma is suspected
Congenital Cataract
B-scan ultrasound if fundus view is obscured
Red blood cell (RBC) galactokinase activity and RBC galactose-1-phosphate-uridyltransferase activity (to rule out galactosemia)
Serum calcium (to rule out hypocalcemia or hypoparathyroidism)
Serum glucose (to check for diabetes mellitus and hypoglycemia)
Urine copper level (to check for Wilson’s disease)
Urine amino acid content (to check for Lowe’s syndrome)
Urine protein and blood quantitation (to check for Alport’s syndrome)
Urine sodium nitroprusside test (to rule out homocystinuria)
Rubella antibody detection test
Conjunctival Laceration
B-scan ultrasound
CT scan of the orbit (axial and coronal views) to rule out an intraorbital or intraocular foreign body or a ruptured globe
Hyperacute Conjunctivitis
Gram stain
Cultures:
Blood agar (supports growth of most bacteria)
Chocolate agar (enhances isolation of Haemophilus, Moraxella, and Neisseria)
Thayer-Martin plate (isolates Neisseria)
Antibiotic sensitivity testing (Fig. 3-11)
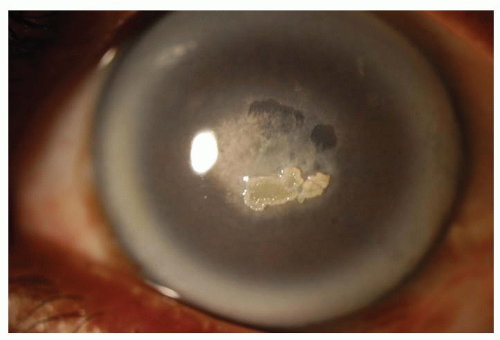
Cornea: Central Crystalline Dystrophy
Fasting serum cholesterol
Serum triglycerides (to check for hypercholesterolemia and hyperlipidemia) (Fig. 3-12)
Corneal Thinning
CBC with differential, ESR, RF, and ANA (to rule out collagen vascular disease)
Cultures (if infection is suspected):
Blood agar
Chocolate agar
Sabouraud’s agar
Thioglycolate agar
Gram stain
Giemsa stain
If a scleritis is present:
RPR and PTA-ABS
Uric acid
FBS
Serum protein electrophoresis and circulating immune complexes (if connective tissue disease is suspected)
C-reactive protein
B-scan ultrasound (to detect posterior scleritis)
CT scan or MRI, if indicated
Chest x-ray
PPD with anergy panel
X-rays of joints
X-ray of sacroiliac joints
Internal medicine consult if collagen vascular disease or leukemia is suspected
Infectious Corneal Ulcers
Smears and cultures:
Blood agar
Chocolate agar
Sabouraud’s medium
Thioglycolate broth
Gram stain
Giemsa stain
Other stains:
Methenamine silver (if fungal infection)
Potassium hydroxide preparation and periodic acid-Schiff (PAS) stains (useful in identifying fungi)
Papanicolaou stain (to rule out intranuclear inclusions)
Acid-fast (when Mycobacterium or Nocardia is suspected)
Calcofluor white (when Acanthamoeba is suspected)
Other media:
Lowenstein-Jensen agar (if Mycobacterium or Nocardia are suspected)
Thayer-Martin agar (to isolate Neisseria)
Brain-heart infusion broth (useful in patients with fastidious bacteria or fungi, or those already on antibiotics)
Nonnutrient agar with E. coli overlay (if Acanthamoeba is suspected)
Cortical Blindness
CT or MRI scan of the brain
CBC (to rule out polycythemia)
Neurologic consult to evaluate risk of stroke
Cranial Arteritis (See Headache) Cystoid Macular Edema
Fluorescein angiography (may show classic “flower petal” pattern)
When indicated:
FBS
GTT
CRVO lab tests
BRVO lab tests
ERG (retinitis pigmentosa [RP]); other lab tests indicated by suspected etiology
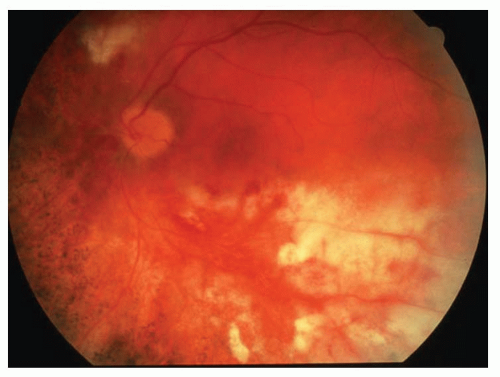
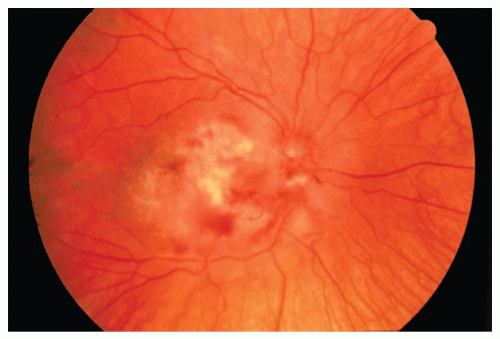
Cytomegalovirus (CMV) Retinopathy
Urine studies for CMV
ESR
Consider fluorescein angiography
Complement fixation test
Internal medicine consult
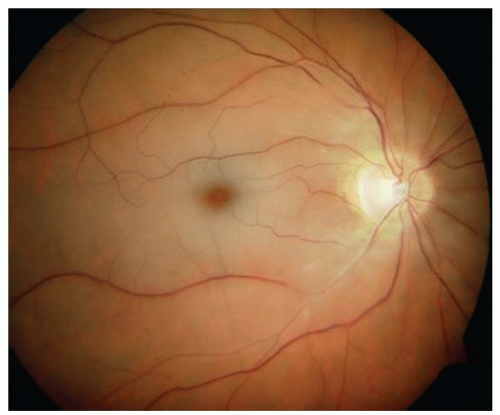
Consider HIV tests (Fig. 3-13)
Dacryoadenitis
Acute Infectious
Cultures of any discharge:
Blood agar
Chocolate agar
Sabouraud’s medium
Thioglycolate broth
Gram stain
CBC with differential (if patient is febrile)
CT scan (axial and coronal views) of the orbit and brain (if a mass is suspected, if there is a motility restriction, or if there is a proptosis)
Chronic
CBC with differential
ESR
ACE
PPD with anergy panel
Chest x-ray (to help detect sarcoidosis or TB)
RPR or VDRL and FTA-ABS
CT scan (axial and coronal views) of the orbit
Lacrimal gland biopsy (if a malignant tumor is suspected or if the diagnosis is uncertain)
If a lymphoma is suspected:
Bone marrow biopsy
CT scan of the abdomen
CT scan of the brain
Serum protein electrophoresis
Internal medicine or oncology consult
Dacryocystitis
Cultures of material expressed from punctum:
Blood agar
Chocolate agar
Sabouraud’s medium
Thioglycolate broth
Gram stain
CT scan (axial and coronal views) of the orbit and paranasal sinuses (if condition does not improve, or in atypical cases)
Diabetic Retinopathy