Purpose
To determine ocular signs predictive of tubercular uveitis.
Design
Retrospective, nonrandomized, comparative interventional case study.
Methods
Three hundred eighty-six patients with active uveitis were treated at a tertiary care single-center uveitis practice. Uveitis was presumed to be tubercular in patients who showed evidence of latent or manifest tuberculosis without any other known cause and who did not show recurrence of uveitis after 12 months of antitubercular therapy. One hundred eighty-two patients who thus obtained clinical diagnoses of presumed tubercular uveitis were enrolled in group A. Two hundred four patients with uveitis resulting from a nontubercular cause were enrolled in group B. Patients were monitored for the presence of types of keratic precipitates (mutton fat or fine), posterior synechiae (broad based or filiform), iris nodules, snowballs, snow banking, vasculitis (with or without choroiditis), serpiginous-like choroiditis, and other types of posterior uveitis (choroidal abscess, retinochoroiditis, or exudative retinal detachment) which were compared between the 2 groups. Statistical analysis was carried out at a 5% level of significance. The main outcome measures were clinical signs significantly associated with tubercular uveitis.
Results
Broad-based posterior synechiae, retinal vasculitis with or without choroiditis, and serpiginous-like choroiditis were seen significantly more commonly in patients with tubercular uveitis. Filiform posterior synechiae were more frequent in eyes with nontubercular uveitis.
Conclusions
Broad-based posterior synechiae, retinal vasculitis with or without choroiditis, and serpiginous-like choroiditis in patients with latent or manifest tuberculosis in tuberculosis-endemic areas are suggestive of a tubercular cause of uveitis and merit specific treatment.
Intraocular tuberculosis (TB) produces a wide spectrum of clinical signs, including anterior granulomatous uveitis, chronic anterior uveitis, intermediate uveitis, choroiditis, retinal vasculitis, serpiginous-like choroiditis, choroidal granuloma, and panuveitis. Because many of these entities also may be the result of nontubercular causes, diagnosing tubercular uveitis in TB-endemic areas poses a major challenge. In the absence of confirmatory investigations, the diagnosis of presumed tubercular uveitis is made in patients with supportive clinical findings and a positive clinical response to antitubercular therapy with no recurrences of inflammation thereafter.
Antitubercular therapy is highly effective in reducing the recurrences of uveitis in patients with latent or manifest TB. By time patients seek treatment for uveitis, most do not show evidence of manifest TB. The tuberculin skin test and the more recent QuantiFERON Gold test detect tubercular infection, and a positive test result may suggest a possible tubercular cause. Confirmatory test results, such as demonstration of acid-fast bacilli, culture of Mycobacterium tuberculosis , or histopathologic evidence, seldom are available from the ocular specimens. The conventional polymerase chain reaction technique to detect mycobacterial deoxyribonucleic acid from the ocular fluids, although highly specific, is an invasive procedure, besides having poor sensitivity. Determining specific clinical signs that predict a possible tubercular cause may enhance the pretest probability of a positive result from these investigations.
Methods
We conducted a retrospective chart analysis of all consecutive uveitis patients attending the uveitis clinic of our institution between 1991 and 2005. Institutional ethics committee approval was obtained. We compared clinical signs between 2 groups of patients. Group A included patients with a diagnosis of presumed TB uveitis. Group B, which served as the control group, included patients with uveitis presumed to be of nontubercular origin. Patients with the following inclusion criteria were enrolled in group A: (1) complete clinical records of ophthalmic examination including visual acuity, intraocular pressure, slit-lamp biomicroscopic findings including anterior as well as posterior segment details, laboratory investigations, and treatment records at the baseline and at all follow-up visits; (2) all known causes of infectious uveitis except TB and known noninfectious uveitic syndromes ruled out; (3) a documented positive tuberculin skin test (10 mm of induration or more) at 48 to 72 hours; (4) received antitubercular therapy for a minimum of 12 months in addition to conventional corticosteroids; (5) a minimum follow-up of 1 year from the initiation of antitubercular therapy; and (6) no recurrence of uveitis after receiving a minimum of 12 months of antitubercular therapy. Patients in group B with the following inclusion criteria served as the controls: (1) a documented negative tuberculin skin test (less than 10 mm of induration) at 48 to 72 hours; (2) no evidence of extraocular manifest TB; (3) never received antitubercular therapy; and (4) a minimum of 6 months of follow-up from the initiation of anti-inflammatory therapy.
As a routine, all patients recruited in the uveitis clinic of our institution undergo a complete ocular as well as systemic examination. Systemic evaluation is carried out by consultant internists (P.B., A.S.) who have a special interest in systemic inflammatory diseases. The baseline investigations for every patient include complete blood counts, erythrocyte sedimentation rate, tuberculin skin test, chest radiograph, and Treponema pallidum hemagglutination test. The tuberculin skin test is ordered when the patient first seeks treatment at the uveitis clinic. An induration of 10 mm or more is considered positive. Ancillary tests such as ultrasonography, fundus fluorescein angiography, indocyanine green angiography, optical coherence tomography, or ultrasound biomicroscopy and specific laboratory tests are performed as and when indicated. Intraocular fluid (aqueous or vitreous) is subjected to polymerase chain reaction analysis as and when suggested by the treating ophthalmologist.
The specific investigations and management of uveitis patients, including initiation of antitubercular therapy, have been described earlier. Corticosteroids are the mainstay of therapy in all cases of noninfectious uveitis. Patients with infectious uveitis receive specific antimicrobial therapy. Immunosuppressive therapy is administered when the inflammation has responded poorly to initial treatment with corticosteroids or as corticosteroid-sparing treatment. Immunosuppression requires diligent management and is always supervised by the internist(s) (P.B., A.S.).
Besides recording demographic information such as patient’s age, sex, laterality of uveitis, treatment record in the form of antitubercular therapy, routes of corticosteroid or immunosuppressive therapy (or both), response to treatment, and the duration of follow up, the information that we retrieved specifically for this study included all the clinical signs of uveitis (present in one or both the eyes). For statistical purposes, only certain specific signs such as types of keratic precipitates (mutton fat or fine), broad-based (base wider than the height) or filiform posterior synechiae, iris nodules, snowball opacities in the vitreous, exudates in the pars plana (snow banking), retinal vasculitis (with or without an accompanying choroiditis scar), serpiginous-like choroiditis, or other types of active choroiditis were analyzed. Other manifestations of posterior uveitis, such as focal retinitis or retinochoroiditis, exudative retinal detachment, necrotizing retinitis, choroidal abscess or granuloma, and neuroretinitis, also were noted.
Statistical Analysis
A chi-square test (or Fisher exact test wherever necessary) was applied to qualitative variables such as the groups (A and B) and the clinical signs (mutton fat or fine keratic precipitates, broad-based or filiform posterior synechiae, iris nodules, snowballs, snow banking, retinal vasculitis with or without active or healed choroiditis patch, serpiginous-like choroiditis, other types of active choroiditis, and other types of posterior uveitis) as a test of independence, in addition to descriptive statistics like mean, median, standard deviation, and range. Univariate as well as multivariate logistic regression analyses were carried out to determine the clinical predictors of tubercular uveitis. Sensitivity, specificity, positive predictive value, negative predictive value, and likelihood ratio of each clinical sign were calculated using Sharon E. Straus’s Stats Calculator, available on her EBM web site ( http://www.cebm.utoronto.ca/practise/ca/statscal/ ). Statistical analysis was carried out at the 5% level of significance.
Results
There were 182 patients in group A, with 95 males and 87 females. Group B had 204 patients, with 101 males and 103 females. During the same period, an additional 134 patients were diagnosed with presumed TB uveitis but were not included in group A, because they did not fulfill the inclusion criteria, that is, less than 1 year of follow-up (92 patients), intolerance or adverse side effects to antitubercular therapy (14 patients), and poor compliance (28 patients). Likewise, 74 patients with other than tubercular uveitis were excluded from group B because of inadequate follow-up. The mean age was 34.7 ± 12.2 years (range, 12 to 70 years) in group A and 34 ± 13.6 years (range, 3 to 75 years) in group B. The median follow-up was 24 months (range, 12 to 140 months) and 33.5 months (range, 6 to 109 months) in groups A and B, respectively. Evidence of manifest systemic TB was found in 15 patients (pulmonary TB in 10, tubercular meningitis in 1, tubercular lymphadenitis in 3, and abdominal TB in 1 patient) in group A. All other patients in group A had evidence of latent TB. No patient in group B had evidence of latent or manifest systemic TB ( Table 1 ). A specific cause was established in 92 (45.1%) patients in group B ( Table 2 ).
| Baseline Characteristics | Group A | Group B |
|---|---|---|
| Total no. of patients | 182 | 204 |
| Gender | ||
| Male | 95 | 101 |
| Female | 87 | 103 |
| Age (yrs) | ||
| Mean ± SD | 34.7 ± 12.2 | 34 ± 13.6 |
| Range | 12 to 70 | 3 to 75 |
| Follow-up (mos) | ||
| Median | 24 | 33.5 |
| Range | 12 to 140 | 6 to 109 |
| TB | ||
| Latent | 167 | None |
| Manifest | 15 | None |
| Anterior uveitis | 53 | 83 |
| Intermediate uveitis | 29 | 50 |
| Posterior uveitis | 70 | 49 |
| Panuveitis | 30 | 22 |
| Cause | No. (%) |
|---|---|
| Idiopathic | 112 (54.9%) |
| Specific | 92 (45.1%) |
| Sarcoidosis | 41 (43.1%) |
| HLA B27–associated anterior uveitis/ankylosing spondylitis | 15 (15.8%) |
| VKH | 12 (12.6%) |
| Behçet disease | 11 (11.6%) |
| Fuchs uveitis | 7 (7.3%) |
| Toxoplasmosis | 2 (2.1%) |
| Juvenile idiopathic arthritis | 1 (1.1%) |
| Multiple sclerosis | 1 (1.1%) |
| Cat-scratch disease | 1 (1.1%) |
| Leprosy | 1 (1.1%) |
| Total | 204 |
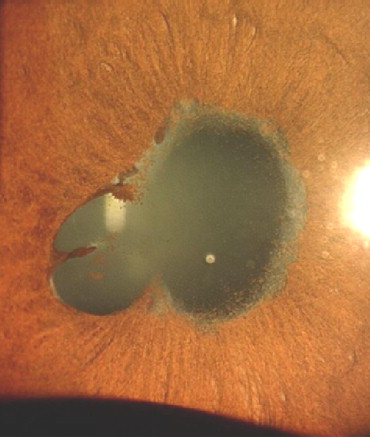
Posterior synechiae, when present, were broad based in 58 (31.9%) in group A ( Figure 1 ) and in 15 (7.4%) in group B. Filiform synechiae were seen in 30 (16.5%) patients in group A and in 55 (27%) patients in group B. The difference in both types of posterior synechiae between the 2 groups was statistically significant ( P < .0005 and P = .01, respectively; Table 3 ). Group A had 56 (30.8%) patients with retinal vasculitis ( Figure 2 ) and 26 (14.3%) patients with serpiginous-like choroiditis ( Figure 3 ). Group B had 37 (18.1%) patients with retinal vasculitis and 3 (1.5%) patients with serpiginous-like choroiditis. Both of these signs were significantly more common in group A ( P = .004 and P < .0005, respectively). Of 56 patients with retinal vasculitis in group A, active or healed choroiditis lesions ( Figure 4 ) were seen in 14 patients (25%), compared with only 1 (2.7%) of 37 patients with retinal vasculitis in group B ( P = .004).
| Clinical Signs | Group A (n = 182) | Group B (n = 204) | P Value (Chi-Square Test) |
|---|---|---|---|
| Mutton fat KP (n = 26) | 13 (7.1%) | 13 (6.4%) | .76 |
| Fine KP (n = 86) | 33 (18.1%) | 53 (26%) | .06 |
| Broad-based PS (n = 73) | 58 (31.9%) | 15 (7.4%) | <0.0005 |
| Filiform PS (n = 85) | 30 (16.5%) | 55 (27%) | .01 |
| Iris nodules (n = 9) | 5 (2.7%) | 4 (2%) | .74 a |
| Snowball (n = 127) | 60 (33.7%) | 67 (32.8%) | .85 |
| Snow banking (n = 32) | 17 (8.3%) | 15 (8.4%) | .97 |
| Vasculitis (all; n = 93) | 56 (30.8%) | 37 (18.1%) | .004 |
| Vasculitis with choroiditis patch (n = 15) | 14 of 56 (25%) | 1 of 37 (2.7%) | .004 a |
| Multifocal choroiditis (n = 34) | 14 (7.7%) | 20 (9.8%) | .46 |
| Serpiginous-like choroiditis (n = 29) | 26 (14.3%) | 3 (1.5%) | <0.0005 |
| Other posterior uveitis (n = 15) | 3 (1.6%) | 12 (5.9%) | .04 a |
On univariate logistic regression analysis, broad-based posterior synechiae, retinal vasculitis with or without choroiditis, and serpiginous-like choroiditis favored a tubercular cause. However, filiform posterior synechiae favored a nontubercular cause ( Table 4 ). On multivariate regression analysis, broad-based posterior synechiae, retinal vasculitis (with or without choroiditis), and serpiginous-like choroiditis remained independent predictors of tubercular uveitis ( Table 5 ). The odds ratio of broad-based posterior synechiae was 10.32 (95% confidence interval [CI], 5.29 to 20.16); that of retinal vasculitis without choroiditis was 3.10 (95% CI, 1.71 to 5.62); that of retinal vasculitis with choroiditis was 40.99 (95% CI, 5.13 to 327.86); and that of serpiginous-like choroiditis was 26.07 (95% CI, 7.43 to 91.47). Although all the 3 clinical signs were significant ( P < .0005), Wald statistics (46.72) were strongest for the broad-based posterior synechiae as a predictor of tubercular uveitis. Further, the 95% CIs for broad-based posterior synechiae were narrow compared with those of retinal vasculitis with choroiditis (Wald statistic, 12.25).
| Clinical Predictors | Odds Ratio | 95% Confidence Interval | P Value |
|---|---|---|---|
| Broad-based posterior synechiae | 5.89 a | 3.19 to 10.86 | <.0005 |
| Filiform posterior synechiae | 0.53 b | 0.32 to 0.88 | .01 |
| Retinal vasculitis | 2.00 a | 1.24 to 3.22 | .004 |
| Vasculitis with choroiditis patch | 12.00 a | 1.50 to 95.76 | .004 |
| Serpiginous-like choroiditis | 11.16 a | 3.31 to 37.56 | <.0005 |
| Other types of posterior uveitis | 0.26 b | 0.07 to 0.96 | .03 |
| Variables | Wald | P Value | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|
| Age | .66 | .418 | 1.01 | 0.99 to 1.03 |
| Gender | .23 | .634 | .89 | 0.53 to 1.46 |
| Broad-based posterior synechiae | 46.72 | <.0005 | 10.32 | 5.29 to 20.16 |
| Filiform posterior synechiae | .00 | .954 | 1.02 | 0.56 to 1.84 |
| Vasculitis without choroiditis patch | 13.93 | <.0005 | 3.10 | 1.71 to 5.62 |
| Vasculitis with choroiditis patch | 12.25 | <.0005 | 40.99 | 5.13 to 327.86 |
| Serpiginous-like choroiditis | 25.93 | <.0005 | 26.07 | 7.43 to 91.47 |
| Other types of posterior uveitis | 2.40 | .122 | .32 | 0.08 to 1.35 |
The sensitivity and specificity were 32% and 93%, 25% and 97%, 10% and 99%, 14% and 98% for broad-based posterior synechiae, retinal vasculitis without choroiditis, retinal vasculitis with choroiditis, and serpiginous-like choroiditis, respectively ( Table 6 ). The positive and negative predictive values were 79% (95% CI, 69 to 87) and 60% (95% CI, 55 to 65) for broad-based posterior synechiae, 93% (95% CI, 70 to 99) and 46% (95% CI, 35 to 57) for retinal vasculitis without choroiditis, 93% (95% CI, 70 to 99) and 57% (95% CI, 51 to 62) for retinal vasculitis with choroiditis, and 90% (95% CI, 74 to 96) and 56% (95% CI, 51 to 61) for serpiginous-like choroiditis. The likelihood ratios (+) were 4.33 for broad-based posterior synechiae, 9.25 for retinal vasculitis without choroiditis, 16.80 for retinal vasculitis with choroiditis, and 9.71 for serpiginous-like choroiditis ( Table 6 ).
| Clinical Signs | Sensitivity (%) | Specificity (%) | Positive Predictive Value (95% CI) | Negative Predictive Value (95% CI) | Pretest Probability | Positive Likelihood Ratio | Negative Likelihood Ratio | Posttest Probability | Overall Diagnostic Accuracy |
|---|---|---|---|---|---|---|---|---|---|
| Mutton fat keratic precipitates | 7 | 93 | 50% (32 to 68) | 53% (48 to 58) | 47% | 1.12 | 0.99 | 50% | 53% |
| Fine keratic precipitates | 18 | 74 | 38% (28 to 49) | 50% (45 to 56) | 47% | 0.70 | 1.10 | 38% | 47% |
| Broad-based posterior synechiae | 32 | 93 | 79% (69 to 87) | 60% (55 to 65) | 47% | 4.33 | 0.73 | 79% | 64% |
| Filiform posterior synechiae | 16 | 73 | 35% (26 to 46) | 49% (44 to 55) | 47% | 0.61 | 1.14 | 35% | 46% |
| Iris nodules | 2 | 98 | 55% (27 to 81) | 53% (48 to 58) | 47% | 1.40 | 0.99 | 55% | 53% |
| Snowballs | 33 | 67 | 47% (39 to 56) | 54% (47 to 59) | 47% | 1.02 | 0.98 | 47% | 51% |
| Snow banking | 8 | 91 | 47% (31 to 63) | 53% (48 to 58) | 47% | 1.01 | 0.99 | 47% | 53% |
| Retinal vasculitis (all) | 30 | 82 | 60% (50 to 70) | 57% (51 to 62) | 47% | 1.69 | 0.84 | 60% | 58% |
| Vasculitis without choroidits a | 25 | 97 | 93% (70 to 99) | 46% (35 to 57) | 47% | 9.25 | 0.77 | 93% | 54% |
| Vasculitis with choroiditis b | 10 | 99 | 93% (70 to 99) | 57% (51 to 62) | 47% | 16.80 | 0.90 | 93% | 59% |
| Multifocal choroiditis | 7 | 90 | 41% (26 to 57) | 52% (47 to 57) | 47% | 0.78 | 1.02 | 41% | 51% |
| Serpiginous-like choroiditis | 14 | 98 | 90% (74 to 96) | 56% (51 to 61) | 47% | 9.71 | 0.86 | 90% | 59% |
| Logistic regression model | 60 | 84 | 77% (70 to 83) | 70% (64 to 70) | 47% | 3.82 | 0.47 | 77% | 73% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


