Purpose
To define the maturational sequence of 3 infantile intraocular medulloepitheliomas.
Design
Retrospective clinicohistopathologic and immunohistochemical study.
Methods
Immunoreactivity of paraffin sections for CRX (cone-rod homebox transcription factor) and NeuN (biomarker for neuronal differentiation) were investigated together with other biomarkers, including S100, glial fibrillary acidic protein, epithelial membrane antigen, and various cytokeratins.
Results
Three infants (aged 1, 6, and 8 months) had iris neovascularization, 2 had anterior ciliary body tumors, and 1 a posterior tumor associated with a retinochoroidal coloboma. Each tumor displayed a premedullary monolayer of cuboidal epithelium that was S100 + , NeuN − , and CRX − and that transitioned into a multilaminar medullary epithelium forming neurotubules with adluminal cells that were CRX + . NeuN first appeared in ablumenal neurotubular cells in 1 tumor and was also discovered among neuroblast-appearing cells in another. The third tumor associated with a coloboma was CRX − and NeuN − .
Conclusions
A simple premedullary epithelial monolayer appears to be the fundamental source for the tumor and its multilaminar medullary epithelium. CRX + and NeuN + cells within the multilayered medullary layer approximate expression patterns similar to those found in retinal development and differentiation. Discovery of these biomarkers in the neoplastic ciliary epithelium in a small number of tumors indicates preliminarily that the most anterior layers of the optic cup have a retained retinal and neuroglial differentiation potentiality. The third case was CRX − and NeuN − and possibly arose from embryonic pigment epithelium at the edge of the retinochoroidal coloboma. These immunohistochemical findings offer histogenetic and potential diagnostic insights.
Intraocular medulloepithelioma is the counterpart of intracranial and peripheral medulloepitheliomas. These are rare primitive and multipotential neoplasms. Medulloepithelioma arises in the eye from embryonic neuroepithelium, traditionally termed medullary epithelium, that derives from an evagination of the anterior embryonic neural tube to form the optic vesicle and subsequent cup.
In the current study, 3 ocular medulloepitheliomas of infancy, each with its own distinctive morphologic features, were evaluated to further elucidate their histogenesis by means of careful histopathologic analyses and immunohistochemical investigations. The application of various immunoprobes led to an analysis of the tumors’ molecular overlaps and differences, with a particular emphasis on evaluating the roles of CRX for photoreceptor development and NeuN for neuronal differentiation. We are fully cognizant that our findings and interpretations are preliminary, because the small sample size of 3 cases presented herein does not fully encompass the wide spectrum of histomorphologic expressions encountered in intraocular medulloepitheliomas.
We identified a simple neuroepithelial precursor cell type that forms a monolayer that we have designated as a premedullary epithelium and that has not been well characterized in the past. It was discovered to merge into the classical formations of multilaminar or pseudostratified medullary epithelium that typifies the composition of most of the tumors. We also addressed whether the appearance of neurogenous or “brain tissue,” previously considered a teratoid or heteroplastic component, may more accurately be regarded as an intrinsic, homoplastic (ie, nonalien) differentiation feature of some of these tumors.
Methods
This clinicopathologic retrospective study was conducted under the auspices of the Massachusetts Eye & Ear Infirmary’s Institutional Review Board (IRB number 14-064H), in compliance with the rules and regulations of the Health Insurance Portability and Accountability Act and all applicable federal and state laws, and in adherence to the tenets of the Declaration of Helsinki. After searching through the regular diagnostic and consultation files of the David G. Cogan Laboratory of Ophthalmic Pathology of the Massachusetts Eye and Ear Infirmary from January of 2000 to April of 2013, 3 cases were considered acceptable for inclusion in this study based on availability of paraffin blocks dating from August of 2002, December of 2009, and March of 2013 when the enucleated eyes were processed in the laboratory. The histopathologic features displayed in formalin-fixed, paraffin-embedded, and hematoxylin-eosin-stained sections on glass slides were reexamined. Additionally, each case was sent in consultation to either Dr Ralph Eagle of the Wills Eye Hospital, Philadelphia, Pennsylvania, or Dr Ramon Font of the Baylor College of Medicine, Houston, Texas, for confirmation of the diagnosis. The paraffin blocks were used to obtain additional immunohistochemical staining. One case has been separately reported; the use of different immunohistochemical stains with a new investigative focus was the basis for the inclusion of this case in the present study. Patients’ medical records, diagnostic imaging studies, and clinical photographs were also reexamined for possible correlations.
Immunohistochemical staining was performed on the 3 cases employing the antibodies listed in Table 1 . The studies were conducted in the Diagnostic Immunopathology Laboratories of the Massachusetts General Hospital and Brigham and Women’s Hospital, Boston, Massachusetts. Immunostaining was performed using the Leica Bond III (Leica Microsystems, Bannockburn, Illinois, USA) with appropriate controls to validate antibody quality. Internal controls consisted of normal, nontumoral tissues in the enucleated globes. Endogenous peroxidase activity was blocked by H 2 O 2 before antibody incubation. The chromogen diaminobenzidine was used because background, nonspecific staining could be controlled with this agent; the tissues were counterstained with hematoxylin. Nuclear staining was recorded as percent positivity for Ki-67 (proliferation index), whereas nuclear, cytoplasmic, or cell membrane staining was noted for the other antibodies as simply positive or negative if 5% or more of the cells were stained.
| Marker | Characterization | Selected Cell/Tissue Specificities | Staining Pattern | Source | Dilution |
|---|---|---|---|---|---|
| CD99 | Cell adhesion molecule; 30-23 kDa cell surface glycoprotein | Glioblastoma and ependymoma of CNS; Ewing’s sarcoma; some primitive peripheral neuroectodermal tumors | Membranous | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | Prediluted |
| CEA (carcinonoembryonic antigen) | 180 kDa glycoprotein that is 50% carbohydrate available to a variety of CEA epitopes | Breast, gastrointestinal, hepatobiliary cancers; secretory meningiomas; pleomorphic adenomas; malignant melanomas; malignant non-Hodgkin lymphomas; thymomas | Cytoplasmic | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | Prediluted |
| Chromogranin | Acidic, soluble protein, originally identified in adrenal chromoffin granule; 48 kDa | Granule-containing neuroendocrine cells and their tumors; peripheral nerves; some meningiomas and astrocytomas | Cytoplasmic, granular | Mouse monoclonal (Dako, Carpinteria, California, USA) | 1:100–1:200 |
| CRX (photoreceptor nuclear protein) | Cone-rod homeobox transcription factor (CRX); gene product recognized by 32 kDa antibody against amino acids 166–285 near the C-terminus of protein | Expressed in the developing retina; persists as nuclear staining of photoreceptors postnatally into adulthood; labels pineal gland, as well as tumors arising from it such as ectopic retinoblastoma and pineoblastoma; 40% of medulloblastomas | Nuclear | Rabbit polyclonal IgG (Santa Cruz Biotechnology, Inc., Santa Cruz, USA) | 1:30 |
| EMA (epithelial membrane antigen) | 75 kDa transmembrane glycoprotein (related to breast mucin) | Glandular epithelium and mesothelium (indicative of epithelial differentiation together with cytokeratins); retinal pigment epithelium; squamous epithelial but not basaloid cells | Cytoplasmic and membranous | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | Prediluted |
| NeuN (neuronal nuclear protein) | Low-molecular-weight (∼40 kDa protein); a product of the FOX3 gene | Most differentiated neuronal cells, retinal ganglion cells, not photoreceptors or Purkinje cells | Nuclear | Mouse monoclonal (EMD Millipore Corp, Billerica, Massachusetts, USA) | 1:7500 |
| NSE (neuron-specific enolase) | Glycolytic homo- or heterodimeric isoenzymes (46 kDa) of glycolytic enzyme system; appear late in neuronal differentiation | Tumors derived from or containing neurons, ganglion cells, retinal cells, and peripheral nerves; neuroendocrine tumors; meningiomas, astrocytomas, schwannomas | Cytoplasmic | Mouse monoclonal (Dako, Carpinteria, California, USA) | 1:100–1:200 |
| Synaptophysin | Synaptic vesicle membrane glycoprotein, present in neuronal presynaptic vesicles | Neuronal and neuroendocrine tissue and tumors, retinal cells, optic nerve | Cytoplasmic, vesicular, and diffuse | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | Prediluted |
| S100(A) | Member of a family of calcium binding proteins such as calmodulin and troponin C; composed of dimeric alpha and beta chains; guides calcium fluxes and microtubular assembly; low-molecular-weight (21 kDa) | Mostly cytoplasm and occasionally nuclei of melanocyte, Schwann cell, glial cell, retinal pigment epithelium, retinal cells, optic nerve, among other cell types | Cytoplasmic and nuclear | Rabbit polyclonal (Dako, Carpinteria, California, USA) | 1:400 |
| GFAP (glial fibrillary acidic protein) | 50 kDa intracytoplasmic filamentous protein | Brain astrocytes; Schwann cells, especially enteric Schwann cells; myoepithelial cells; desmoplastic medulloblastoma; plexiform, diffuse and simple neurofibroma, schwannomas; glioblastoma multiforme | Cytoplasmic | Rabbit polyclonal (Dako, Carpinteria, California, USA) | 1:500 |
| Neurofilament | Intermediate cytoplasmic filaments composed of 3 subunits of related proteins: NF-L (70 kDa), NF-M (150–160 kDa), and NF-H (200 kDa) | Neuronal processes in gangliogliomas; neuronal perikarya; Merkel cell tumors; axons in bundles of Auerbach and Meissner; nerve fiber layer of retina | Cytoplasmic | Mouse monoclonal (Dako, Carpinteria, California, USA) | 1:50–1:100 |
| Vimentin | Intermediate cytoplasmic filament, 57 kDa protein | Mesenchymal cells; anterior and posterior iridial pigmented epithelium; pigmented and nonpigmented ciliary epithelium; normal subcapsular lens epithelium and cataractous epithelium (Wedl cells) | Cytoplasmic | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | Prediluted |
| Ki-67 | Nuclear protein associated with premitotic DNA replication | Cells active in phases G1, S, G2, and M of the cell cycle | Nuclear | Mouse monoclonal (Dako, Carpinteria, California, USA) | 1:200 |
| AE1 | Keratin proteins of low to intermediate molecular weights (56.5, 50, 48, and 40 kDa) in the acidic subfamily | Epithelial cells in early stages of cell development, retinal pigment epithelium | Cytoplasmic | Mouse monoclonal (Invitrogen Corp, Camarillo, California, USA) | 1:1000 |
| AE3 | Keratin proteins of intermediate to high molecular weights (65–67, 64, 59, 58, 56, and 52 kDa) in the basic subfamily | Maturing epithelial cells including squamous cells; retinal pigment epithelium | Cytoplasmic | Mouse monoclonal (Invitrogen Corp, Camarillo, California, USA) | 1:100 |
| CAM5.2 | Keratin proteins of low to intermediate molecular weights (48 and 52 kDa) | Basal cells of glandular epithelia; myoepithelia; retinal pigment epithelium; simple epithelia | Cytoplasmic | Mouse monoclonal (Invitrogen Corp, Camarillo, California, USA) | 1:80 |
| CK 7 | Cytoplasmic intermediate filament; 54 kDa; basic | Epithelia of simple glands; eccrine and apocrine secretory coils; lacrimal glands; conjunctival epithelium; metastases originating above the diaphragm | Cytoplasmic | Mouse monoclonal (Dako, Carpinteria, California, USA) | 1:3 |
| CK 10 | Intermediate filament; 56.5 kDa; acidic | Keratinized stratified epithelium; large epidermoid (prekeratinizing) cells; differentiated squamous cell carcinomas | Cytoplasmic | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | 1:200 |
| CK 14 | Intermediate filament; 50 kDa; acidic | Basal layer of squamous (conjunctival) and glandular epithelia; myoepithelial cells; sebaceous tumors; mucosal carcinomas | Cytoplasmic | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | 1:100 |
| CK 17 | Intermediate filament; 46 kDa; acidic | Basal layer of glandular epithelia; myoepithelial cells; conjunctival basal cells; conjunctival squamous dysplasias | Cytoplasmic | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | Prediluted |
| CK18 | Intermediate filament; 45 kDa; acidic | Glandular epithelia of gastrointestinal and respiratory tracts; conjunctival basal cells; rhabdoid tumors; nonpigmented ciliary epithelium | Cytoplasmic | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | 1:100 |
| CK 20 | Intermediate filament; 46 kDa; acidic | Simple epithelia of gastrointestinal tract; Merkel cells of epidermis and their tumors; epithelial tumors and metastases originating below the diaphragm; totally negative in conjunctiva (no Merkel cells present) | Cytoplasmic | Mouse monoclonal (Leica Biosystems, Newcastle, UK) | Prediluted |
Results
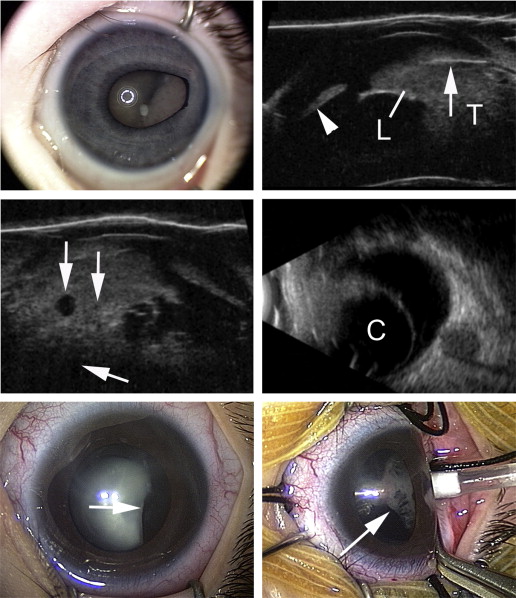
Table 2 summarizes the clinical findings of the 3 cases included in this study. Because the ages of the infants at presentation ranged from 1 month to 8 months, vision was unobtainable. The 3 cases manifested iris neovascularization at presentation. In Case 1 there was a solid-appearing, well vascularized posterior chamber mass ( Figure 1 , Top left). Ultrasonography disclosed a partially solid lesion without calcifications that displaced the iris leaflet anteriorly and embraced the lens ( Figure 1 , Top right). Small cysts ( Figure 1 , Middle left) and a dominant large cyst in the posterior half of the mass were also identified ( Figure 1 , Middle right). In Case 2 a lens coloboma was detected on clinical evaluation ( Figure 1 , Bottom left) and a delicate neoplastic posterior chamber membrane was interposed between the iris and the face of the lens ( Figure 1 , Bottom right). A mass, however, was not detectable on ophthalmoscopy or B-scan ultrasonography of the ciliary body region owing to the small size of the tumor. Ultrasonography in Case 3 disclosed a solid mass lacking calcifications with many internal acoustic interfaces; it filled the posterior and central vitreous and was inseparable from the retina. Tumor sampling performed on 2 patients by needle aspiration of the vitreous ( Table 2 , Cases 2 and 3) revealed the presence of undifferentiated neuroblastic cells, which then led to an enucleation.
| Case | Sex | Eye | Age | Initial Vision | Symptoms & Signs a | Location | Ultrasound | Procedure(s) | Follow-up b |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | OS | 6 m | Not obtainable | Enlarging leukocoria noted 2 months earlier; irregular pupil with poor response to light; iris neovascularization with ectropion uveae; shallowing of the anterior chamber; examination under anesthesia revealed tumor-associated cysts | Temporal | Enlarged eye; complex cystic mass with small and giant cysts, no calcification; measured 9 mm in height × 12 mm at base | Examination under anesthesia; enucleation | 17 m |
| 2 | M | OD | 8 m | Not obtainable | Injection of conjunctiva for 1 week; enlarged globe; glaucoma (Tmax 55) with Haab corneal striae; lens coloboma; retrolenticular membrane seen after lensectomy; no focal mass observed | Temporal | Enlarged corneal diameter and axial length; vitreous debris; no detectable ciliary body mass on ultrasonography; mass measured 1 mm in height × 1.5 mm at base in enucleation specimen | Examination under anesthesia; lensectomy; vitrectomy with positive cytologic evaluation; enucleation | 12 y |
| 3 | F | OD | 1 m (born prematurely at 31 weeks) | Not obtainable | Iris neovascularization; stalk extending from posterior pole to lens discovered during retinopathy of prematurity screening at 2 weeks postpartum, suggesting persistent hyperplastic primary vitreous; 2 weeks later developed into vascularized retrolenticular mass | Inferonasal | Large mass with displacement of iris leaflet; no calcifications; mass measured 13 mm in height × 14 mm at base | Examination under anesthesia; fine needle aspiration of vitreous; positive cytologic evaluation; enucleation | 4 y |
a No patient was noted to have an afferent pupillary defect.
The following summaries focus on the important histopathologic and immunohistochemical findings in the examination of each enucleated globe.
Histopathologic and Immunohistochemical Findings
Case 1
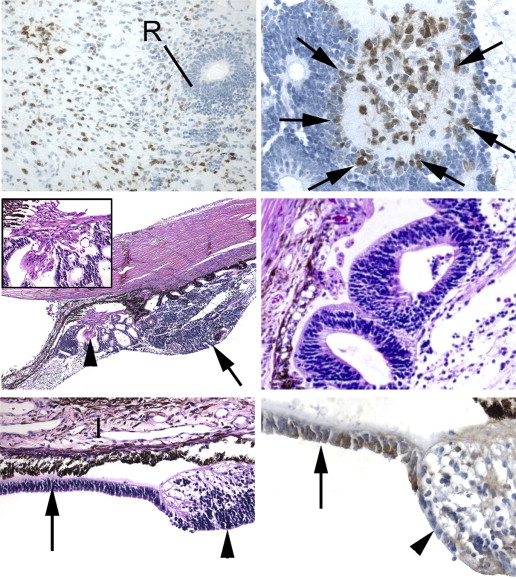
A large ciliary body tumor protruded into the pupil and displaced the iris anteriorly to create peripheral anterior synechiae ( Figure 2 , Top left). The iris manifested a delicate surface neovascular membrane with ectropion uveae. At the apex next to the lens there was a monolayer of cuboidal cells, sometimes reduplicated, that formed strands of a primitive premedullary epithelial monolayer ( Figure 2 , Top right). These cells were enveloped in Alcian blue–positive, vitreous-like material ( Figure 2 , Middle left) and disappeared anteriorly ( Figure 2 , Middle right). This simple epithelium recurved into the tumor, where it transformed into a multilayered medullary epithelium ( Figure 2 , Bottom left), forming neurotubules composed of mitotically active cells with a high nuclear-to-cytoplasmic ratio and scant detectable cytoplasm. Beneath the neuroepithelial zone was an eosinophilic neuropil composed of interweaving cellular processes. In one focus, ganglion-like cells with capacious cytoplasm and large nuclei with prominent nucleoli were observed ( Figure 2 , Bottom right). The foregoing overall architecture was seen in other regions of the mass ( Figure 3 , Top left), for example, behind the iris and near the ciliary processes. A giant cyst ( Figure 3 , Top right) and smaller cystic spaces containing eosinophilic material were distributed throughout the substance of the tumor. Some small cysts were formed that were lined by both a monolayer and multilaminar epithelium. The dominant cyst was lined by an ependyma-like, cuboidal to low columnar epithelium without identifiable cilia that focally underwent multilamination ( Figure 3 , Top right).
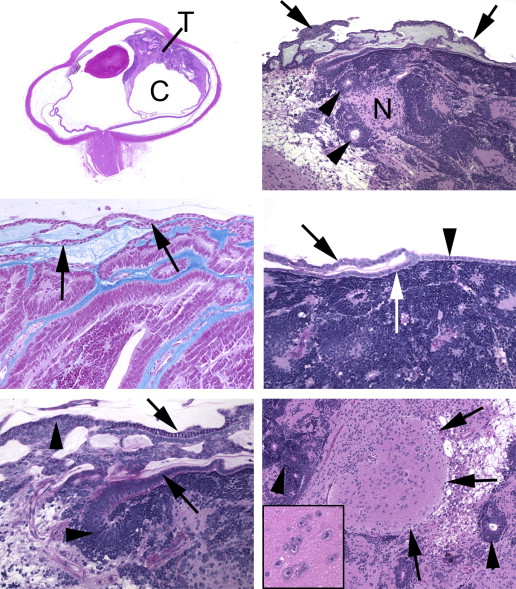
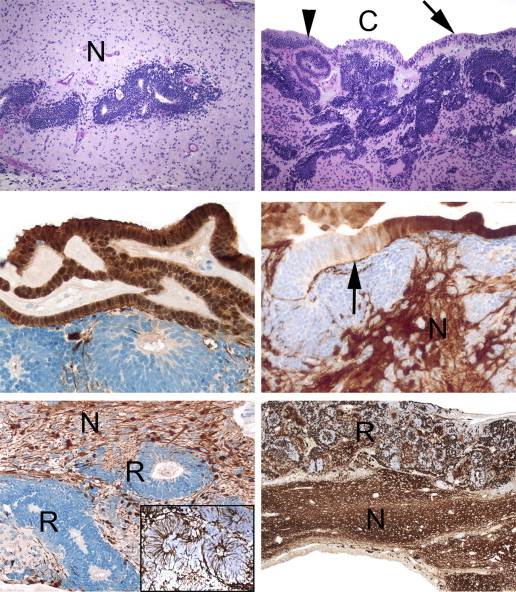
S100 and CD99 were positively immunostained in the premedullary monolayer of cuboidal epithelium ( Figure 3 , Middle left). These positivities disappeared as the monolayer transitioned into the medullary epithelium ( Figure 3 , Middle right). S100 staining was demonstrated in the neuropil and in the lining cells of the large cyst but not in the scattered neuroepithelial units ( Figure 3 , Bottom left). Vimentin was identified in the cytoplasm of all of the cell types comprising the tumor. It was distinctively arranged at the peripheries of the cells comprising the neurotubules, imparting a spidery appearance ( Figure 3 , Bottom left, inset). Small adjacent cysts in the neuropil next to the dominant cyst that had partial linings of a monolayer were focally S100 positive. Synaptophysin was identified in a vesicular form in the neurotubules ( Figure 3 , Bottom right, and Figure 4 , Top left), but not in the premedullary epithelium. Neuron-specific enolase highlighted the nuclear membranes in the medullary epithelium of the neurotubules and scattered cells in the neuropil ( Figure 4 , Top left, inset), but was negative in the premedullary epithelium and the ependyma-like cells. Epithelial membrane antigen, carcinoembryonic antigen, and cytokeratins including CK18 were negative in the premedullary epithelium, the neuroepithelial tubular formations, and the ependyma-like cells. The neuropil exhibited diffuse positive staining for synaptophysin ( Figure 3 , Bottom right). Neurofilament ( Figure 4 , Top right, left panel) and GFAP ( Figure 4 , Top right, right panel) staining was found in the neuropil surrounding the neurotubules but was negative within neuroepithelial units and the ependyma-like cells. The ependyma-like cells were synaptophysin negative. Chromogranin, myoglobin, myogenin, desmin, and smooth-muscle actin were not observed in any of the tumor cells. Ki-67 positivity was absent in the neuropil but strikingly positive in, and restricted to, the neuroepithelial tubules (proliferation index of around 10%).
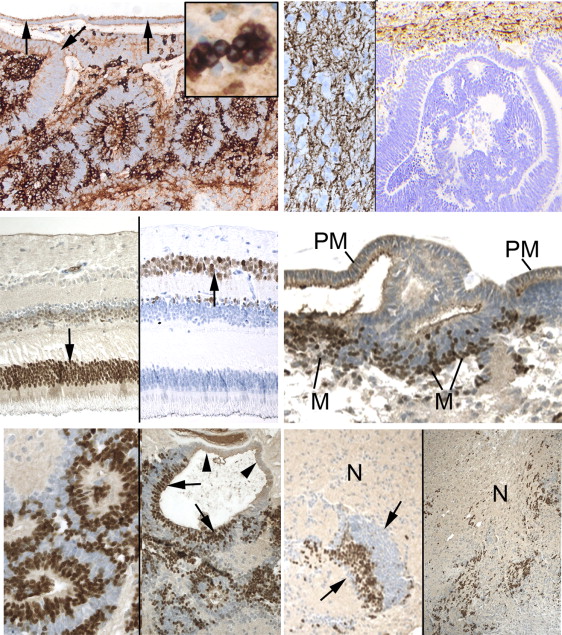
CRX, a nuclear marker for both photoreceptor progenitor cells and fully differentiated photoreceptors ( Figure 4 , Middle left, left panel), was negative in the premedullary epithelium and ependyma-like cells but strongly positive in the nuclei of the multilaminar medullary epithelium and neurotubules ( Figure 4 , Middle right and Bottom left, left panel). This marker first appeared at the juncture between the premedullary epithelial monolayer and the progressively multilayered medullary epithelium, similar to the pattern seen in normal retina at the ora serrata ( Figure 4 , Middle right). In neurotubules composed of a monolayer and multilayered epithelium, the monolayer of cells was CRX negative while the multilayered segments were positive ( Figure 4 , Bottom left, right panel). CRX-positive small cells were also located next to clusters of nonstaining cells, the latter possibly the tangentially sectioned outer portions of neurotubular formations ( Figure 4 , Bottom right, left panel). CRX-positive cells were also lightly scattered in the neuropil ( Figure 4 , Bottom right, right panel). NeuN, a nuclear marker for neurons and ganglion cells ( Figure 4 , Middle left, right panel), was not seen in the premedullary or medullary epithelium, but was exclusively observed in the neuropil in varying densities in different locales ( Figure 5 , Top left). One exception to this general statement is that occasional multilaminar neurotubular formations, or dense small “colonies” of neuroblastic-type cells within the neuropil, expressed NeuN in the outermost cells that splayed into the neuropil ( Figure 5 , Top right). The ependyma-like cells were CRX and NeuN negative. The diagnosis was a benign medulloepithelioma with prominent neuroglial differentiation.
Case 2
This tumor had caused a mild enlargement of the globe along with iris neovascularization and ectropion uveae. It was very small, achieving a maximal height of 1.5 mm. The mass grew on the surfaces of intact but blunted ciliary processes towards the pars plana ( Figure 5 , Middle left). The central portion of the lesion resting on the ciliary processes was composed of a mixture of loosely dispersed small neuroblastic cells with a high nuclear-to-cytoplasmic ratio, and non-lumen-forming curvilinear cords and circlets of 1 or 2 layers of cuboidal cells enclosing lightly eosinophilic amorphous material that was Alcian blue positive. Multilaminar neurotubules ( Figure 5 , Middle right) were also noted. A bundle of eosinophilic spindle cells was located at the base of the mass and behind the root of the iris and above the ciliary processes in intimate relation to neuroepithelial cords ( Figure 5 , Middle left and inset). The dispersed neuroblastic and rosetting cells behind the iris terminated in a monolayer of premedullary epithelial cells that extended toward the pupil ( Figure 5 , Bottom left).
The posterior chamber retro-iridial premedullary epithelial monolayer was S100 positive ( Figure 5 , Bottom right); the rosette-like structures and the round neuroblastic cells were S100 negative but NSE positive. Synaptophysin positivity was not observed in the neuroblastic cells and neuroepithelial units. S100 and GFAP were positive in the cellular fascicles at the base of the mass above the ciliary processes ( Figure 6 , Top left and Top right). These spindle cells appeared to originate from incompletely lumenized curvilinear cords of neuroepithelial cells that were S100 positive, whereas most of the cells forming complete lumens were S100 negative ( Figure 6 , Top left). CD99, myoglobin, smooth-muscle actin, epithelial membrane antigen, carcinoembryonic antigen (CEA), and chromogranin were all negative. The premedullary epithelial strand in the posterior chamber was CRX negative ( Figure 5 , Bottom right). CRX was profusely positive in the neuroblastic cells on the surface of the retro-iridial membrane ( Figure 6 , Middle left and Middle right), as well as in the rosettes overlying the ciliary processes, very similar to the pattern seen in Case 1. When this primitive neuroepithelial monolayer of premedullary epithelium transformed into a multilayered region, CRX positivity became particularly apparent ( Figure 6 , Middle right). NeuN positivity was much more rarely and selectively expressed in the neuroblastic cells but not in the lumen-forming tumor cells ( Figure 6 , Middle right, inset). The Ki-67 nuclear proliferation index was 5% and was equally prominent in both rosettes and neuroblastic cells. The lesion was diagnosed as a benign medulloepithelioma with focal astrocytic differentiation.
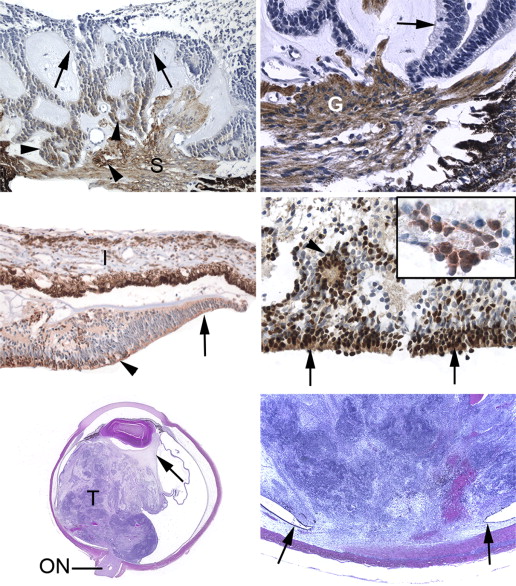
Case 3
A delicate capillarized pupillary and iris surface membrane was noted. The lens was deformed and indented posteromedially ( Figure 6 , Bottom left). The iris leaflets had been displaced forward by a solid retrolenticular mass that filled the vitreous body. The retina was identifiable and only poorly laminated in the anterior medial hemisphere; the remainder of the medial retina was not identifiable. The anterior half of the lateral hemispheric retina was intact and well formed. A loose mesenchyme was located immediately around the lens with elongated ciliary processes, suggesting persistence of primary hyperplastic vitreous ( Figure 6 , Bottom left). Behind this zone and filling most of the vitreous body was a mitotically active spindle cell proliferation forming short fascicles that alternated with myxoid zones exhibiting fewer mitoses. Posteromedially between the equator and optic nerve head, there was a retinochoroidal coloboma ( Figure 6 , Bottom right). At the edges of the coloboma and beneath the tumor the pigment epithelium underwent a transition into a nonpigmented medullary neuroepithelial monolayer composed of low cuboidal cells ( Figure 7 , Top left, Top right, and Middle left). This epithelium appeared to break up into small cell clusters that blended imperceptibly with the loose spindle and round cell proliferation constituting a large part of the tumor ( Figure 7 , Top right). Further anteriorly, the premedullary epithelium transitioned into the beginning of a multilaminar medullary epithelium that eventually transformed into partially differentiated retina ( Figure 7 , Middle left). The medullary epithelium posterior to the coloboma invaginated to create neurotubules ( Figure 7 , Middle right). The most posterior region of the tumor, adjacent to the optic nerve head, displayed multilaminar neurotubules and Homer Wright rosettes ( Figure 7 , Bottom left and Bottom right). Neuroblastic round cells were present between the more organized elements. Alcian blue staining was either negative or only very faintly positive in some regions of the tumor. There was no tumor extension into the optic nerve. The atrophic choroid was involved by the tumor only superficially in the segment of the coloboma; there was no scleral invasion.




