Purpose
To investigate the incidence and the clinical factors associated with the occurrence of multiple subretinal fluid (SRF) blebs after successful rhegmatogenous retinal detachment (RD) repair.
Design
Retrospective, observational case series.
Methods
We retrospectively investigated the medical records of 185 eyes of 184 patients who had undergone successful RD surgery, either vitrectomy or scleral buckling. Each patient had undergone spectral-domain optical coherence tomography (SDOCT) combined with infrared reflectance (IR) imaging every 3 months postoperatively. We carefully examined postoperative SDOCT and fundus IR images, in an effort to identify any SRF blebs present.
Results
Multiple (≥3) SRF blebs were observed in 40 of 185 cases (21.6%). SRF blebs were first detected 1.7 ± 1.8 months postoperatively. In 22 cases that could be fully followed up, SRF blebs were completely absorbed 13.1 ± 6.1 months postoperatively. Multiple logistic regression analysis showed that only young age (<30 years) was significantly associated with the occurrence of multiple SRF blebs (odds ratio, 5.1; 95% confidence interval, 1.5-17.6; P = .010). Serial measurements of SRF bleb size using SDOCT showed that SRF bleb height was greatest at postoperative 2.9 ± 0.9 months, while SRF bleb width tended to decrease gradually over time. The SRF blebs typically spared large retinal vessels.
Conclusions
Multiple SRF blebs are commonly found after successful RD surgery, especially in young patients. The serial morphologic features evaluated in this study indicate that multiple SRF blebs may result from the active reattachment of retinal pigment epithelium and photoreceptors during the resolution of RD.
Optical coherence tomography (OCT) has been used to elucidate the pathophysiology of many retinal diseases, which previously could only have been investigated through the use of histopathologic techniques. By incorporating OCT into the postoperative assessment of retinal detachment (RD) patients, we were able to detect subclinical levels of subretinal fluid (SRF) that is usually not detected through routine binocular ophthalmoscopic examination. Aside from the persistence of SRF, bleb-like lesions may arise in the previously detached retina during the postoperative follow-up period after successful retinal reattachment. These lesions appeared similar to those associated with serous detachment of the retinal pigment epithelium (RPE), and using fluorescein angiography, histopathologic review, and OCT, they were determined to be focal sensory retinal detachment. The described pockets were observed in subfoveal and peripheral areas, whereas the persistent SRF described previously was found primarily in dependent positions, the fovea, or the inferior part of the retina. Moreover, bleb-like SRF pockets usually arise in clusters (more than 3), in contrast to confluent SRF or single SRF blebs.
Kang and associates reported the incidence and presumed mechanism of SRF blebs. They observed SRF blebs in 11 of 118 patients (9.3%) who underwent successful scleral buckling (SB) and cryotherapy for rhegmatogenous RD. They proposed choroidal vascular damage caused by cryotherapy as the main mechanism of SRF bleb occurrence. However, when we evaluated multiple SRF blebs with serial spectral-domain OCT (SDOCT), we noticed additional characteristics that have not been suggested before.
In this study, we aimed to investigate the incidence and clinical risk factors associated with multiple SRF blebs that could be found after successful rhegmatogenous RD surgery and also to elucidate the presumed mechanism of SRF bleb occurrence.
Methods
We retrospectively reviewed the medical records of all the patients who underwent either pars plana vitrectomy (PPV) or SB surgery for rhegmatogenous RD at Seoul National University Bundang Hospital from January 1, 2009, to June 30, 2012. This study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Seoul National University Bundang Hospital. A total of 340 patients (343 eyes) underwent rhegmatogenous RD repair during that period, and ultimately 185 eyes from 184 patients were included in this study. We included only patients with primary spontaneous RD who achieved a successful postoperative course, and we excluded those with complicated RD, primary failure cases, or re-detachment cases. Specifically, we excluded patients who underwent silicone oil injection for retinal reattachment. We also excluded those with preoperative retinal pathology that could have influenced retinal reattachment—for example, trauma history, epiretinal membrane, vitreomacular traction syndrome, combined tractional RD, proliferative vitreoretinopathy (subretinal gliosis), and macular pathology. We excluded reoperation cases as well as patients with incomplete courses of postoperative OCT follow-up.
All surgeries were performed by 4 experienced retinal surgeons at Seoul National University Bundang Hospital (P.K.H., W.S.J., A.J., and H.D.J.). The surgeons decided the method of operation, either PPV or SB, based on the clinical characteristics of each patient and RD. Younger patients and those with small definite tears, especially those located inferiorly, were likely to undergo SB, whereas elderly patients with cataracts or pseudophakia and suspicious or hidden tears were more likely to undergo PPV. A 23 gauge transconjunctival sutureless vitrectomy system (Accurus; Alcon Laboratories, Inc, Fort Worth, Texas, USA) was used for PPV. In brief, we used perfluorocarbon liquids during the surgery, and internal SRF drainage was performed through the original tear. After the surgery, the eye was filled with gas (18% SF 6 or 14% C3F8). In SB surgery, we identified the retinal tear and then performed cryotherapy. The explant material was silicone sponge with width of 5 or 7.5 mm (No. 506 or 507; MIRA, Waltham, Massachusetts, USA) for the segmental SB and silicone tire (No. 287; MIRA) and silicone band (No. 240; MIRA) for the encircling SB. External SRF drainage was performed during SB surgery in 7 of 82 cases (8.5%).
Each patient underwent a thorough ophthalmologic examination, including best-corrected visual acuity (BCVA; Snellen visual acuity chart), slit-lamp examination, binocular indirect ophthalmoscopy, and SDOCT combined with infrared reflectance (IR) confocal scanning laser ophthalmoscopy (Spectralis OCT; Heidelberg Engineering, Heidelberg, Germany) at 1 month after surgery and every 3 months thereafter until any SRF disappeared.
For the visual acuity analysis, we converted Snellen visual acuity values to the logarithm of the minimal angle of resolution (logMAR). We evaluated only patients without any preoperative ocular disorders that might influence visual function (eg, amblyopia and untreated severe cataracts). Final visual acuity was defined as visual acuity obtained at least 6 months after the complete resolution of any subfoveal SRF and at least 3 months after cataract surgery in patients who underwent cataract surgery during the follow-up period.
Subretinal Fluid Bleb and Optical Coherence Tomography Analysis
We carefully searched for the presence of SRF bleb using both postoperative SDOCT images and fundus IR images. We retrieved fundus IR images to identify any bleb-like lesion that was dark and round, and then examined SDOCT volume scans spanning an area of 30 × 20 degrees for any SRF bleb lesion. If there were peripherally located SRF blebs beyond the scope of routine imaging, we obtained peripheral images. We defined multiple SRF blebs as 3 or more localized fluid pockets under the extrafoveal retina with or without subfoveal bleb. We excluded those cases with only a single subfoveal bleb. When preoperative SDOCT images were available, we evaluated whether there was any severe undulation (>3 undulations in a single section) in the outer portion of the detached retina. To characterize the serial morphologic changes typical of SRF bleb, we selected 1 SRF bleb from each patient that could be traced with SDOCT throughout the clinical course, then measured its width and height at baseline (when the SRF bleb first appeared) and at its most prominent stage (when the SRF bleb was highest in OCT images and prominent in IR images) using the caliper tool in the OCT software.
Statistical Analysis
We compared preoperative and intraoperative characteristics between those with and without multiple SRF blebs. Some of these factors were significantly associated with the occurrence of SRF bleb in the univariate analysis, which was performed using either the Student t test for continuous variables or the χ 2 or Fisher exact test for categorical variables. We performed multiple logistic regression analysis with these factors to eliminate confounding effects. All statistical analyses were performed using PASW version 18.0 (SPSS, Inc, Chicago, Illinois, USA), and P values < .05 were considered statistically significant.
Results
The 185 eyes (184 patients) that underwent successful primary rhegmatogenous RD repair were ultimately included. Multiple SRF blebs were observed postoperatively in 40 eyes (40 patients) out of 185 eyes (21.6%). In most cases (33 cases, 82.5%), SRF blebs were first detected at 1 month postoperatively; another 5 cases (12.5%) exhibited SRF blebs within 6 months after the surgery. In 2 cases (5%) with diffuse persistent subclinical SRF, SRF blebs first occurred at 8 months postoperatively, as SRF was absorbed. Overall, SRF bleb was first identified on SDOCT 1.7 ± 1.8 (mean ± SD) months postoperatively. In 22 cases, we were able to confirm the complete absorption of SRF blebs with SDOCT during the follow-up period. The SRF blebs were completely absorbed within 1 year after surgery in 10 cases (45.5%) and within 2 years postoperatively in another 10 cases (45.5%). The longest duration of SRF blebs was 28 months postoperatively (13.1 ± 6.1 months postoperatively). For those 18 cases that we could not follow fully until the SRF blebs were completely absorbed, the OCT follow-up period was relatively short (3.6 ± 2.4 months). The cumulative survival curve of SRF bleb during the follow-up period is represented in Figure 1 .
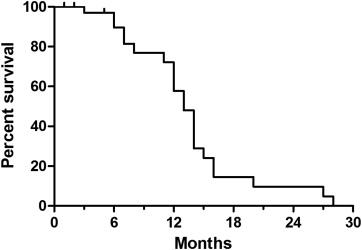
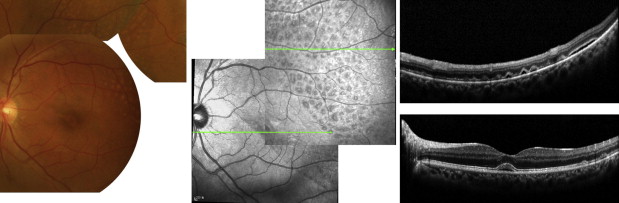
Figure 2 shows an example of a color fundus photograph and fundus IR and SDOCT images of multiple SRF blebs. The SRF blebs are more readily visible on IR images, as round dark lesions. They can be found anywhere in the previously detached retina, either submacularly or peripherally. In SDOCT images, these dark lesions were revealed to be small subretinal fluid pockets. In Figure 2 , the subfoveal fluid, separated from multiple SRF blebs in the superior temporal area, is apparent. In this study, we did not count eyes with subfoveal fluid alone as a multiple SRF bleb case.
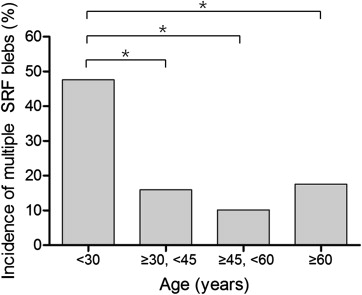
Demographics and clinical characteristics were compared between eyes with and without multiple SRF blebs. Patients with multiple SRF blebs were younger (36.6 ± 20.2 years vs 47.2 ± 15.9 years, P = .003) than those in the control group. When we stratified patient age by quartile, multiple SRF blebs were most prevalent in the youngest age group (<30 years), while the other 3 age groups did not show any significant differences ( Figure 3 , Table ). Patients with multiple SRF blebs were also associated with phakia (97.5% vs 82.8%, P = .018), preoperative macula-off (87.5% vs 64.1%, P = .005) and SB surgery (70% vs 37.2%, P = .001) compared to the control group. However, there were no significant differences between groups in terms of RD chronicity, the number or location of tears, the extent of the RD, or visual outcomes ( Table ).
| Multiple SRF Blebs (+) (N = 40) | Multiple SRF Blebs (-) (N = 145) | Odds Ratio | 95% CI | P Value a | |
|---|---|---|---|---|---|
| Age (y), mean ± SD | 36.6 ± 20.2 | 47.2 ± 15.9 | .003 | ||
| <30, n (%) | 20 (50) | 22 (15.2) | 4.3 | 1.6-11.8 | .005 |
| ≥30, <45, n (%) | 7 (17.5) | 37 (25.5) | 0.9 | 0.3-2.8 | .845 |
| ≥45, <60, n (%) | 6 (15) | 53 (36.6) | 0.5 | 0.2-1.7 | .294 |
| ≥60, n (%) | 7 (17.5) | 33 (22.8) | – | – | – |
| Male, n (%) | 24 (60) | 88 (60.7) | 1.0 | 0.5-2.0 | .937 |
| Follow-up period (months), mean ± SD | 15.4 ± 9.1 | 14.1 ± 9.4 | .460 | ||
| Symptom onset (days), mean ± SD | 13.9 ± 24.6 | 10.2 ± 15.8 | .395 | ||
| ≤7 days, n (%) | 25 (62.5) | 102 (70.3) | 0.6 | 0.3-1.3 | .230 |
| >7 days, n (%) | 15 (37.5) | 43 (29.7) | – | – | – |
| Refractive error (SEQ, diopters), mean ± SD | −2.9 ± 5.3 (N = 25) | −3.4 ± 4.1 (N = 75) | .628 | ||
| Phakia, n (%) | 39 (97.5) | 120 (82.8) | 8.1 | 1.1-61.9 | .018 |
| Macula off, n (%) | 35 (87.5) | 93 (64.1) | 3.9 | 1.4-10.6 | .005 |
| Number of tears, mean ± SD | 2.1 ± 1.4 | 2.1 ± 1.5 | .823 | ||
| Tear location, n (%) | .247 | ||||
| Superior | 24 (60) | 102 (70.3) | 1.0 | 0.3-3.2 | >.999 |
| Inferior | 12 (30) | 26 (17.9) | 2.0 | 0.5-7.1 | .305 |
| Combined | 4 (10) | 17 (11.7) | – | – | – |
| Extent of RD (clock hours), mean ± SD | 5.5 ± 2.1 | 5.2 ± 1.9 | .312 | ||
| 1-6 o’clock, n (%) | 33 (82.5) | 123 (84.8) | 0.8 | 0.3-2.1 | .720 |
| 7-12 o’clock, n (%) | 7 (17.5) | 22 (15.2) | – | – | – |
| Preoperative severe retinal undulation, n (%) | 7/27 (25.9) | 13/100 (13) | 2.3 | 0.8-6.6 | .135 |
| Operation methods, n (%) | .001 | ||||
| Pars plana vitrectomy | 12 (30) | 88 (60.7) | 0.3 | 0.1-0.6 | .001 |
| Scleral buckling | 28 (70) | 54 (37.2) | – | – | – |
| Combined | 0 | 3 (2.1) | |||
| Preoperative BCVA (logMAR), mean ± SD | 1.13 ± 0.83 (N = 32) | 0.94 ± 0.88 (N = 122) | – | – | .231 |
| 1 month BCVA (logMAR), mean ± SD | 0.40 ± 0.30 (N = 33) | 0.38 ± 0.32 (N = 121) | – | – | .457 |
| Final BCVA (logMAR), mean ± SD | 0.21 ± 0.34 (N = 23) | 0.14 ± 0.18 (N = 105) | – | – | .982 |
a P values by Student t test or Mann-Whitney test for continuous variables and by χ 2 test or Fisher exact test for categorical variables.
We also performed multiple logistic regression analysis using the 5 most significant factors as identified by the univariable analysis: age, lens status, preoperative macula status, preoperative severe undulation in OCT images, and operation method. We converted age into a dichotomous variable (<30 or ≥30 years), according to the results of the univariable analysis. Only younger age (<30 years) was significantly associated with the occurrence of multiple SRF blebs after RD surgery (odds ratio, 5.1; 95% confidence interval, 1.5-17.6; P = .010).
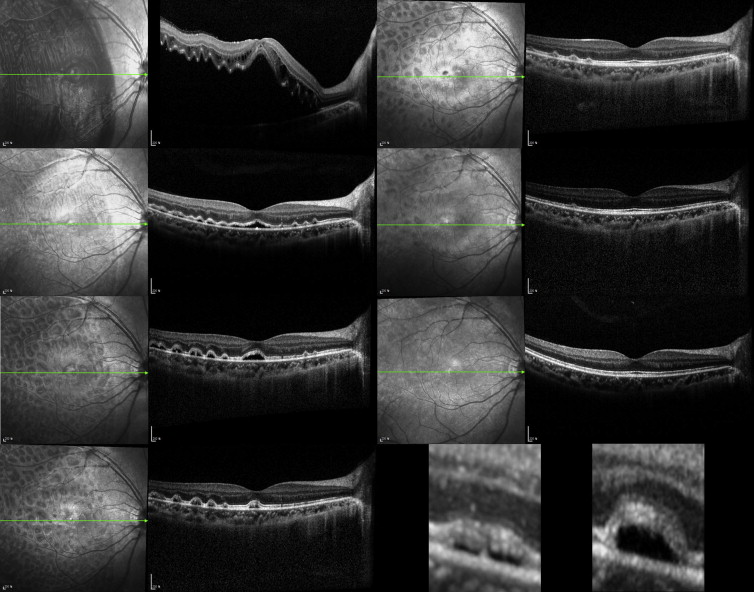
We have presented representative serial fundus IR and SDOCT images showing the dramatic resolution of a prominent cluster of SRF blebs after RD surgery ( Figure 4 ). An 11-year-old boy visited the emergency room complaining of decreased vision with shadowing in the right eye that had started 1 day earlier. Visual acuity was hand motion (OD), 20/25 (OS); and refractive error was −5.75 Dsph = −0.75 Dcyl × Axis 180 (OD), −5.0 Dsph = −1.25 Dcyl × Axis 180 (OS). The fundus examination revealed a temporal macula-off RD with 3 peripherally located tears at the 8, 9, and 10 o’clock position. He underwent SB and cryotherapy with a 506 silicone sponge. Visual acuity in the right eye gradually improved after surgery, ultimately reaching 20/25 postoperatively. In preoperative OCT images, the outer portion of the detached retina showed severe undulation ( Figure 4 , Top left). One month after surgery, the detached retina was approximated on RPE, and multiple SRF blebs were observed. However, these blebs were not readily visible on fundus IR images ( Figure 4 , Second row left and Bottom middle). Three months after surgery, the SRF blebs were prominently visible on fundus IR images, and SRF bleb height on OCT images had increased as well ( Figure 4 , Third row left and Bottom right). The SRF bleb size decreased thereafter, regressing gradually until complete absorption 2 years after the surgery ( Figure 4 , Third row right).