Purpose
To evaluate the multilayer Gore-Tex patch as temporary coverage of deep, noninfectious corneal defects.
Design
Retrospective, interventional case series.
Methods
Setting: University Medical Center Schleswig-Holstein, Kiel, Germany. Patient population: Thirty-nine eyes of 38 patients with noninfectious, deep corneal defects. Underlying disorders included neurotrophic or immunologic ulcers in 37 eyes (94.9%) and traumatic defects in 2 eyes (5.1%). Intervention procedures: Corneal defects were covered with multiple Gore-Tex layers, of which the uppermost was sutured to the cornea. The Gore-Tex patch was kept in place until an appropriate corneal transplant was obtained and effective systemic immunosuppression was initiated. Main outcome measures: Long-term preservation of the eye, frequency of resuturing of the Gore-Tex patch, and best-corrected visual acuity.
Results
In 38 cases, the eye could be preserved. In 10 eyes, additional sutures were required. Before surgery, the mean best-corrected visual acuity (logMAR) was 1.14 ± 0.45 (20/250), and that at final follow-up was 1.13 ± 0.41 (20/250). The Gore-Tex patch remained in place 4 days to 32 months (mean, 6.4 ± 8.3 months) until corneal transplantation (27 eyes) or until an alternative way of defect coverage could be performed. Three eyes did not require further coverage after explantation of the Gore-Tex patch. In 6 eyes, either the Gore-Tex patch was kept in place or the patients died.
Conclusions
Temporary coverage of deep corneal defects with multilayer Gore-Tex patches allows time until an appropriate corneal transplant is obtained. The technique is particularly useful in patients with underlying autoimmune disorders, because an effective systemic immunosuppression can be initiated before corneal transplantation.
Deep corneal ulcers with pending or existing perforation are not always sufficiently treatable with local or conservative therapy, or both. In addition to systemic anti-inflammatory and immunosuppressive therapy, surgery can become mandatory when stromal defects are present. Defects of the periphery can be covered by conjunctival flaps. Amniotic membrane transplantations (AMTs) have been conducted successfully in many cases. AMT facilitates re-epithelialization and reduces inflammation. AMT is a procedure with a low incidence of complications. However, amniotic membranes demand an elaborate preparation and cryofixation and are not universally available. Moreover, because of their minor thickness and limited elasticity, they are hardly suitable for establishing mechanical stabilization in more extensive stromal defects. In cases of corneal perforation with only small stromal defects, a therapeutic contact lens or the use of tissue adhesives may provide mechanical stability and sealing of the anterior chamber. Larger stromal defects often are covered with emergency corneal transplants. However, this procedure often is associated with poor functional outcome. Keratoplasty à chaud for immune-mediated corneal ulcers often is complicated after surgery by impaired epithelial wound healing, a recurrence of corneal melting, and an elevated risk of graft rejection. In traumatic corneal perforation, herpetic ulcers, and immunologic ulcers, a delay of the keratoplasty for 6 to 12 weeks can be beneficial for the clarity and the survival of the graft. This may be connected to a better control of local inflammatory responses, an optimized systemic immunosuppression, and a better quality of the selected graft.
In 1991, Legeais and associates first reported successful temporary coverage of corneal defects with a Gore-Tex patch in 6 patients with corneal perforation. In 1994, Huang and associates reported 3 eyes with corneal defects caused by a Mooren ulcer or necrotizing scleritis covered successfully with a Gore-Tex patch. However, although Gore-Tex material was in use experimentally for keratoprosthesis in a few patients since these first 2 reports of small case series, the Gore-Tex patch as a temporary coverage of corneal defects has not been described in the literature. The technique is not widely applied by ophthalmic surgeons. To our knowledge, after our initial preliminary report of 6 cases, the present study is the first larger case series with long follow-up reporting promising results in patients with corneal defects mostly caused by underlying local or systemic disorders that usually are difficult to manage. The main outcome measures of this retrospective interventional case series were long-term preservation of the eye, frequency of resuturing of the Gore-Tex patch, and best-corrected visual acuity (BCVA).
Methods
The medical records of all patients treated with a temporary Gore-Tex patch between 2000 and 2008 were reviewed. The study was designed as retrospective interventional case series. Mean follow-up was 33.9 ± 29.2 months (range, 1.5 to 108 months). Thirty-eight consecutive patients (24 male, 14 female) with deep noninfectious corneal defects were included. One patient received a Gore-Tex patch in both eyes. Thirteen eyes had perforated corneal defect ulcers; in 11 eyes, a descemetocele was present; and 15 eyes had deep stromal corneal defects without perforation or descemetocele. The corneal defects were of neurotrophic, immunologic, or traumatic origin without signs of bacterial infection. The patients had a number of systemic immunologic diseases, as shown together with the demographic data and the initial diagnosis in Table 1 . At presentation, 10 patients (26.3%) were receiving systemic immunosuppression. Eleven patients (28.9%) died during the observation period as a result of multimorbidity. The mean age at the time of the operation was 62.2 years (standard deviation [SD], 20.5 years; range, 3 to 90 years). Thirty-seven eyes (94.9%) exhibited trophic or immunologic corneal ulcers. Two of these cases sustained injuries decades ago (1 chemical burn and 1 penetrating injury). A 3-year-old patient demonstrated congenital corneal anesthesia. Two patients (5.3%) exhibited acute traumatic corneal defects.
| Patient No. | Age (yrs) | Defect Depth | Defect Location | BCVA (logMAR) | Ocular Diseases | Systemic Diseases | Previous Systemic Immunosuppression | Previous Ocular Surgery |
|---|---|---|---|---|---|---|---|---|
| Primary Gore-Tex patch group (Gore-Tex patch applied as primary coverage) | ||||||||
| 1 | 77 | Perforated | Peripheral | 0.8 | Herpes zoster ophthalmicus | |||
| 2 | 56 | Descemetocele | Peripheral | 1.3 | Chemical burn | |||
| 3 | 57 | Perforated | Peripheral | 0.0 | Primary trophic ulcer | Mycophenolate mofetil | ||
| 4 | 62 | Stromal defect | Peripheral | — | CRVO, secondary glaucoma | Sarcoidosis | ||
| 5 | 58 | Descemetocele | Peripheral | 1.4 | Rheumatoid arthritis | |||
| 6 | 72 | Perforated | Peripheral | 1.3 | Rheumatoid arthritis | MTX, Infliximab | ||
| 7 | 68 | Stromal defect | Peripheral | 0.7 | Primary trophic ulcer | |||
| 8 | 73 | Perforated | Peripheral | 1.0 | Primary trophic ulcer | |||
| 9 | 86 | Perforated | Peripheral | 1.5 | Herpes simplex keratitis | |||
| 10 | 71 | Perforated | Peripheral | 1.4 | B-cell lymphoma, radiation | |||
| 11a | 30 | Perforated | Peripheral | 0.9 | GVHD | Mycophenolate mofetil, CSA | ||
| 11b | 30 | Perforated | Peripheral | 0.4 | GVHD | Mycophenolate mofetil, CSA | ||
| 12 | 23 | Perforated | Peripheral | 1.1 | Acute injury | |||
| 13 | 88 | Perforated | Peripheral | — | Primary trophic ulcer | |||
| 14 | 77 | Descemetocele | Peripheral | 1.0 | POAG | Rheumatoid arthritis | ||
| 15 | 54 | Stromal defect | Peripheral | 1.5 | Psoriatic arthritis | MTX | ||
| 16 | 82 | Perforated | Peripheral | 1.5 | Entropion, POAG | |||
| 17 | 76 | Descemetocele | Peripheral | 1.3 | Herpes zoster ophthalmicus | |||
| 18 | 35 | Stromal defect | Peripheral | 1.2 | Herpes simplex keratitis | Atopic dermatitis | ||
| 19 | 81 | Descemetocele | Central | 0.9 | Rheumatoid arthritis | |||
| 20 | 64 | Stromal defect | Central | 1.3 | Rheumatoid arthritis | Corticosteroids, chloroquine | ||
| 21 | 83 | Descemetocele | Central | 1.5 | Rheumatoid arthritis | |||
| Secondary Gore-Tex patch group (Gore-Tex patch applied as secondary coverage) | ||||||||
| 22 | 71 | Stromal defect | Peripheral | 1.3 | Rheumatoid arthritis | Etanercept | HLA-unmatched penetrating keratoplasty | |
| 23 | 50 | Perforated | Peripheral | 0.6 | Bell palsy | AMT | ||
| 24 | 79 | Descemetocele | Peripheral | 1.6 | Ocular cicatricial pemphigoid | Corticosteroids, MTX | HLA-unmatched penetrating keratoplasty (2x), conjunctival flap | |
| 25 | 63 | Stromal defect | Peripheral | 0.1 | Ocular cicatricial pemphigoid | AMT, HLA-unmatched lamellar keratoplasty | ||
| 26 | 69 | Descemetocele | Peripheral | 0.7 | Acute injury | Rheumatoid arthritis | Chloroquine, azathioprine, etanercept | HLA-matched penetrating keratoplasty, AMT |
| 27 | 79 | Stromal defect | Peripheral | 1.4 | Pseudophakia | HLA-unmatched penetrating keratoplasty | ||
| 28 | 54 | Stromal defect | Peripheral | 1.5 | Previous injury | HLA-unmatched penetrating keratoplasty (2x) | ||
| 29 | 31 | Descemetocele | Peripheral | 1.4 | Keratoconus | HLA-matched penetrating keratoplasty | ||
| 30 | 78 | Descemetocele | Peripheral | 1.1 | Retinal detachment, PPV (3x) | AMT, contact lens | ||
| 31 | 34 | Perforated | Peripheral | 1.6 | Bell palsy | HLA-unmatched penetrating keratoplasty | ||
| 32 | 62 | Stromal defect | Peripheral | 0.1 | Ocular cicatricial pemphigoid | Corticosteroids | HLA-unmatched penetrating keratoplasty | |
| 33 | 89 | Stromal defect | Central | 1.5 | Rheumatoid arthritis | Etanercept | HLA-unmatched lamellar keratoplasty | |
| 34 | 40 | Stromal defect | Central | 1.6 | Eyelid coloboma | HLA-unmatched penetrating keratoplasty | ||
| 35 | 3 | Stromal defect | Central | — | Congenital corneal anesthesia | HLA-matched lamellar keratoplasty | ||
| 36 | 68 | Stromal defect | Central | 1.5 | Previous injury | HLA-matched penetrating keratoplasty | ||
| 37 | 90 | Descemetocele | Central | 1.5 | POAG, multiple surgery | HLA-unmatched penetrating keratoplasty , AMT | ||
| 38 | 61 | Stromal defect | Central | 1.6 | Chemical burn | HLA-unmatched penetrating keratoplasty | ||
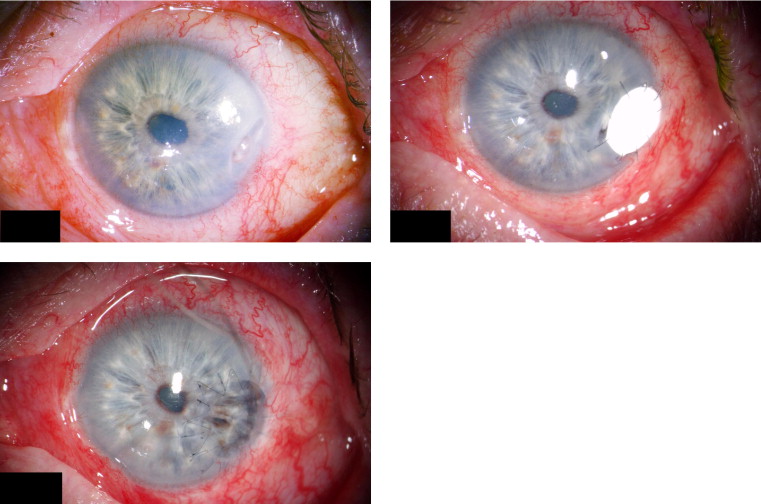
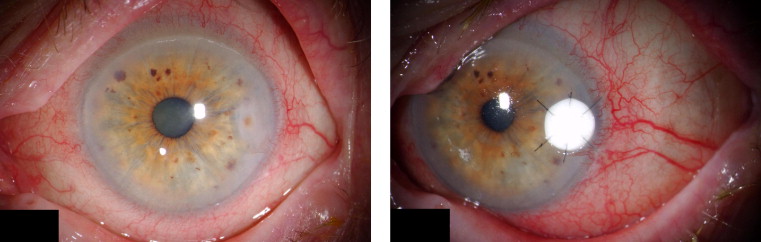
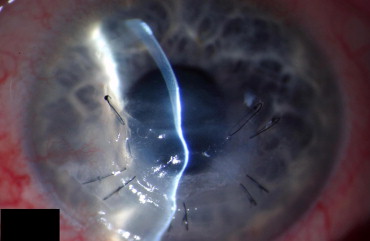
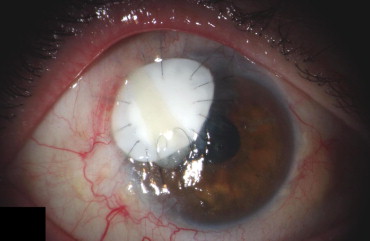
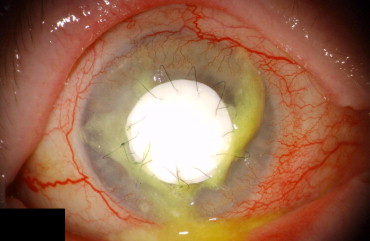
In 22 cases (56.4%), a Gore-Tex patch was applied as a primary coverage (primary GTXP group; cases 1 through 22). In 17 cases (43.6%), a Gore-Tex patch was applied secondary to previous corneal surgery (secondary GTXP group; cases 23 through 38). Sterile Gore-Tex membranes (polytetrafluoroethylene; Gore Preclude, W. L. Gore & Associates, Inc, Flagstaff, Arizona, USA) of 0.1-mm thickness were used in all patients. Figures 1-5 show representative examples. Temporary defect coverage with a Gore-Tex patch was performed with general anesthesia in 20 cases. In the other 19 cases, surgery was performed under local anesthesia. In 20 cases, the patches were manually cut to size ( Figures 1 , Top right, and 4 ), and in 19 cases, a trephine was used ( Figures 2 , Right, and 5 ). To fit the trephined patch into the cornea, a superficial trephination of the cornea of the same diameter was performed, so the patch could be adapted onto resilient tissue. Additionally, the bottom of the lesion was cleared of cellular debris and the surface was disinfected with povidone–iodine. Deeper defects were covered with multiple layers of Gore-Tex of increasing size, of which the uppermost was sutured to the cornea ( Figure 1 , Top left and right). A mean of 2.3 ± 0.8 layers (range, 1 to 4 layers) was used. The largest patch had a size of 6 × 8 mm, and the smallest patch was a trephined disc of 2.5-mm diameter. The graft was secured in place with 10-0 nylon sutures. In 3 cases, running sutures (see Figure 5 ) were placed; in all other cases, interrupted sutures were placed with the knot buried in the host tissue (see Figures 1 , Top right, 2 , Right, and 4 ). Overall, a mean of 9 ± 4 interrupted sutures were placed. After surgery, broad-spectrum antibiotic and prednisolone ointments were applied. In case of insufficient immunosuppression, systemic immunosuppression was initiated in cooperation with the rheumatologists (3 cases) or either adjusted or intensified (5 cases). All surgeries were carried out by the same experienced surgeon (B.N.). A Gore-Tex patch was chosen when success of alternative treatments such as AMT or keratoplasty, either lamellar or perforating, seemed unlikely. In the statistical analysis of the outcome measures, the type I error (α) was set at 0.05. The results were analyzed statistically using Statistica 7.1 (Statsoft, Inc, Tulsa, Oklahoma, USA).
Results
Follow-up until Gore-Tex Patch Explantation
The Gore-Tex patches remained in place for a mean of 6.4 months (SD, 8.3 months; range, 4 days to 32 months). In 4 cases (10.3%), the patch has not been removed so far. Two patients died before the patch was removed. Indications for graft explantation were as follows: in 13 cases (33.3%), an HLA-matched keratoplasty was conducted ( Figure 1 , Bottom). Of these, 3 transplantations were without mismatches (MMs), 4 transplants had 1 MM, 4 transplants had 2 MMs, and 2 transplants had 3 MMs. In 14 cases (35.9%), untyped grafts were used. In 3 cases (7.7%), the corneal situation stabilized to an extent that a tectonic coverage was no longer necessary. In 2 cases (5.1%), coverage was achieved with a conjunctival flap, and in 1 case (2.6%), an AMT was performed. In 10 cases (25.6%), because of a loss of tension of the patch, additional sutures were placed between 2 days and 23 months after the operation (once in 5 patients, twice in 3 patients, 3 times in 1 patient, and 4 times in 1 patient). The necessity for resuturing did not depend on the presence of rheumatoid arthritis or any systemic immunologic disease, on ulcer location, on ulcer perforation, or on primary or secondary Gore-Tex patch coverage ( P = .16; P = .47; P = .44; P = .61; P = .49; Fisher exact test). No additional superficial or intraocular complications occurred. The surface of the Gore-Tex tissue was not epithelialized.
Additional Surgical Procedures
Besides additional sutures, a mean of 1.7 ± 1.4 additional surgical treatments were necessary. In 38 cases (97.4%), the eye could be preserved. In 1 case (2.6%), the eye had to be enucleated 4 years after the Gore-Tex patch was applied, after unsuccessful attempts to undergo a keratoplasty à chaud after an uncontrollable hypotonia bulbi. In 22 cases in which the Gore-Tex patch was applied primarily to cover corneal defects (primary GTXP group), a mean of 1.9 (SD, 1.5) additional surgical interventions were necessary. Seventeen cases that had already undergone surgery before the Gore-Tex patch was applied (secondary GTXP group) needed a mean of 1.5 (SD, 1.2) surgical treatments. The difference between these 2 groups was not statistically significant according to the Mann–Whitney U test ( P = .41). However, the overall number of necessary surgical treatments before and after Gore-Tex patch application was different between these 2 groups. In the primary GTXP group, a mean of 1.9 (SD, 1.5) surgical treatments were conducted. In the secondary GTXP group, a mean of 3.2 (SD, 1.3) operations were performed in addition to the Gore-Tex patch. This difference was statistically significant ( P = .004, Mann–Whitney U test). Mean follow-up was 33.5 months (SD, 33 months) in the primary GTXP group and 34.4 months (SD, 25.5 months) in the secondary GTXP group; the difference was not statistically significant ( P = .36, Mann–Whitney U test). In those 13 cases that received an HLA-matched keratoplasty, 1.1 (SD, 1.4) additional surgeries were performed to stabilize the eye. In those 14 cases that received untyped grafts, a mean of 0.9 (SD, 1.2) operations were needed. The difference between these 2 groups was not statistically significant according to the Mann–Whitney U test ( P = .95). Further information about eye-stabilizing surgeries, follow-up, and visual acuity is shown in Table 2 .



