Objective
To analyze the morphologic features of the choroidoscleral interface in a healthy population using swept-source optical coherence tomography (SS OCT).
Design
Retrospective data analysis of a subgroup of eyes from a previous single-center, prospective, cross-sectional, noninterventional study.
Methods
A total of 276 healthy eyes from 154 subjects were evaluated using SS OCT. Inclusion criteria were best-corrected visual acuity between 20/20 and 20/25, spherical equivalent between ±3 diopters, and no systemic or ocular diseases. Two independent investigators analyzed the morphologic features of the choroidoscleral interface in a masked fashion, classifying the contour and shape as concave (bowl-shaped) or inflective (S-shaped contour with ≥1 inflection point).
Results
The presence of a temporal choroidoscleral interface inflection was identified in 12.8% of the eyes. The mean choroidal thickness was 372.1 ± 76.8 μm and the average distance from the inflection point to the fovea was 4427.3 ± 627.9 μm. Nine patients showed an inflective profile in both eyes. No changes in the retinal profile were found in any of these cases. The mean age of the patients with an inflective profile was 16 ± 19 years (range 4–82) vs 36 ± 25 years (range 3–95) in the group with a concave contour ( P = .001). The temporal choroidal thickness at 4000 and 5000 μm from the fovea was thicker in the group with a concave contour.
Conclusions
Temporal choroidoscleral interface inflection or S-shaped profile of the choroidoscleral interface with focal thinning of the choroid can be considered a normal variation without clinical significance, especially in younger populations.
In recent years, studies of the choroidal anatomy in posterior segment disease using optical coherence tomography (OCT) have increased our knowledge of the role of choroidal changes in various conditions such as central serous chorioretinopathy, age-related macular degeneration, polypoidal choroidal vasculopathy, myopic maculopathy, posterior uveitis, and choroidal tumors. Spaide and associates introduced a technique for improving choroidal imaging using spectral-domain OCT (SD OCT) devices called enhanced depth image (EDI) OCT. EDI OCT provides improved choroidal visualization in most eyes, permitting quantitative and reproducible determination of choroidal thickness. Longer-wavelength swept-source OCT (SS OCT) is an innovative technology available for OCT imaging that further improves choroidal imaging compared to EDI SD OCT. Copete and associates, Ruiz-Moreno and associates, and our group reported that reliable measurement of choroidal thickness is possible in 100% of eyes using an SS OCT device.
Age-related reduction of choroidal thickness in normal eyes, choroidal thickness differences in adult and pediatric eyes, and differences between right and left eye are reported findings using this technique. However, knowledge of choroidal morphology is not complete yet. Adhi and associates described significant alterations in choroidal morphologic features in eyes with advanced diabetic retinopathy (DR). These alterations included an irregular or a temporal choroidoscleral interface inflecting in most DR eyes. In addition, a recent paper reported a focal inferotemporal scleral bulge with choroidal thinning in normal eyes modifying the normal contour and shape (bowl-shaped or concave when looking from the inside out) of the choroidoscleral interface.
The aim of this study is to analyze the morphologic features of the choroidoscleral interface in a healthy population using SS OCT.
Patients and Methods
The data and images of a specific population subgroup from a previously published prospective study were analyzed. This study followed the tenets of the Declaration of Helsinki and the original study was approved by the institutional review board of Vissum Alicante. Data were collected from December 2011 to January 2013. The subjects provided informed consent to participate in the research to study the thickness and morphology of the choroid in a healthy population. Participation was offered to subjects who were attending routine ocular examinations and voluntarily agreed to participate, provided they met the inclusion criteria, with no age limitations, and signed an informed consent. Inclusion criteria were best-corrected visual acuity (BCVA) between 20/20 and 20/25, spherical equivalent (SE) between ±3 diopters (D), and no systemic or ocular diseases (other than cataract). Patients with prior history of any retinal condition in either eye were not included. All examinations were obtained in the afternoon (between 4 PM and 8 PM) to avoid diurnal variations.
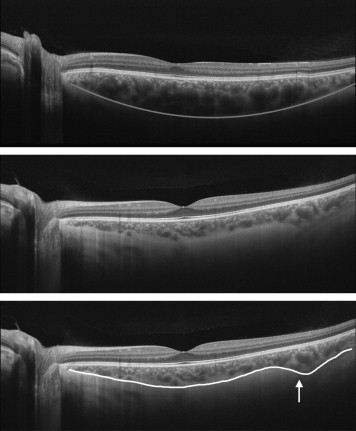
Two independent investigators performed an analysis of the morphologic features of the choroidoscleral interface in a masked fashion, classifying and labeling the contour and shape of the horizontal choroidoscleral interface as previously published. Specifically, the choroidal morphology was defined as being concave (or bowl-shaped) or with temporal choroidoscleral interface inflecting (having an irregular or concave-convex-concave shape with ≥1 inflection point). If the contour was labeled as temporal choroidoscleral interface inflecting, choroidal thickness at the level of the inflection point was measured (as described below), as well as the distance to the fovea ( Figure 1 ).
The mean choroidal thickness measurements in healthy eyes reported previously were used as a reference to define focal thinning/thickening. According to Adhi and associates, eyes were considered to have focal thinning/thickening if choroidal thickness at the measured location was 50% less/more than that of the mean choroidal thickness of normal eyes at the corresponding location. The procedure followed to analyze and measure choroidal thickness profile has been previously described. The macular horizontal choroidal thickness profile (choroidal thickness measured using a horizontal line centered at the fovea, containing 1024 axial scans and with a length of 12 mm) was created with an SS OCT system (Topcon Corporation, Tokyo, Japan), after the patients provided informed consent. A horizontal choroidal thickness profile of the macula was manually created by measuring the choroidal thickness from the posterior edge of retinal pigment epithelium (RPE) to the choroid/sclera junction under the fovea using the prototype software. Eight further determinations were performed every 1000 μm temporal (T1, T2, T3, T4, and T5) and nasal (N1, N2, and N3) to the fovea. The outer aspect of the lamina fusca, rather than the outer limit of the choroidal vessels, was the landmark used to determine the most distal aspect of the choroid and the inner edge of the sclera.
For this study, the reference mirror of SS OCT was placed at the deeper position of the retina so that the sensitivity was higher at the choroidal area in macular imaging. A 1-line scanning mode, which produces an OCT image containing 1024 axial scans with a scan length of 12 mm, was employed. Two observers determined choroidal thickness independently and in a masked fashion.
An experienced technician determined refractive errors and BCVA using an autorefractometer (Nidek, Gamagori, Japan) that was later checked by a certified optometrist.
Data obtained were statistically analyzed using a licensed version of SPSS 17.0 for Windows (SPSS, Chicago, Illinois, USA). The Kolmogorov-Smirnov test was applied for all data samples in order to check normality. Intergroup analysis was performed using the Student t test when samples were normally distributed or Mann-Whitney test when parametric statistics were not possible. The level of significance used was P < .05. The interobserver reproducibility was evaluated using intraclass correlation coefficient (ICC) for each variable measured (mean and 95% confidence interval), coefficient of variation between graders, and Bland-Altman plots.
Results
We analyzed 276 eyes from 154 patients. Ninety-three patients (60.4%) were male and 61 (39.6%) were female. The presence of the concave or bowl-shaped contour of the horizontal choroidoscleral interface was found in 240 of the 276 eyes analyzed (87.2%). The presence of a temporal choroidoscleral interface inflection was identified in 36 out of 276 eyes (12.8%), 19 times in the left eye and 17 in the right eye. All the irregularities or concave-convex-concave shapes with ≥1 inflection point were found in the temporal aspect of the macular choroidal thickness profile. Only 1 inflection point was found in all eyes with a mean distance to the fovea of 4427.3 ± 627.9 μm (range 2531–5492), and it was always located between 2000 and 5000 μm temporal the fovea, except in 6 eyes in which it was located more than 5000 μm away from it ( Figure 2 ). Mean choroidal thickness at the site of the inflection point was 372.1 ± 76.8 μm (range 168–538 μm). In 9 cases the temporal choroidoscleral interface inflection was bilateral ( Figure 3 ). No changes in retinal profile were found in any of these cases.
Mean age of the patients with temporal choroidoscleral interface inflection was 16 ± 19 years (range 4–82 years) vs 36 ± 25 years (range 3–95 years) in the group with bowl-shaped contour ( P = .001; Student t test for unpaired data). Temporal choroidal thickness was also different between both groups. Mean choroidal thickness in the temporal choroidoscleral interface inflection group at the site of T4 was 317.6 ± 80.2 μm (range 120–440 μm) vs 266.3 ± 76.8 μm (range 105–504 μm) in the group with bowl-shaped contour ( P = .001; Mann-Whitney U test). Choroidal thickness in the temporal choroidoscleral interface inflection group was 286.0 ± 71.7 μm (range 160–466 μm) at the site of T5, vs 252.5 ± 77.2 μm (range 66–483 μm) in the bowl-shaped group ( P = .01; Mann-Whitney U test). In contrast, the difference of mean choroidal thickness at T1, T2, and T3 was not statistically different ( P = .26, P = .39, and P = .11, respectively; Mann-Whitney U test).
The prevalence of a temporal choroidoscleral interface inflection profile was 30 out of 120 (12.5%) in the group of patients aged 15 or younger, vs 6 out of 156 (3.8%) in the group of patients aged 16 or older ( P < .01; χ 2 test).
A high agreement in the measures taken by the 2 observers was found. The ICC values obtained for the variables evaluated were within the range 0.966–0.987. The Bland-Altman plots also confirmed high agreement between measures, using ±2 standard deviations as limits of reproducibility.
Results
We analyzed 276 eyes from 154 patients. Ninety-three patients (60.4%) were male and 61 (39.6%) were female. The presence of the concave or bowl-shaped contour of the horizontal choroidoscleral interface was found in 240 of the 276 eyes analyzed (87.2%). The presence of a temporal choroidoscleral interface inflection was identified in 36 out of 276 eyes (12.8%), 19 times in the left eye and 17 in the right eye. All the irregularities or concave-convex-concave shapes with ≥1 inflection point were found in the temporal aspect of the macular choroidal thickness profile. Only 1 inflection point was found in all eyes with a mean distance to the fovea of 4427.3 ± 627.9 μm (range 2531–5492), and it was always located between 2000 and 5000 μm temporal the fovea, except in 6 eyes in which it was located more than 5000 μm away from it ( Figure 2 ). Mean choroidal thickness at the site of the inflection point was 372.1 ± 76.8 μm (range 168–538 μm). In 9 cases the temporal choroidoscleral interface inflection was bilateral ( Figure 3 ). No changes in retinal profile were found in any of these cases.




