Metastatic Carcinomas
Clinical Features
Over the time interval of our study of orbital tumors, 1948 to the present, I am impressed by the proliferation of publications describing carcinomas (chiefly adenocarcinomas) metastatic to the orbit from distant sites, either before or after the primary origin of the tumor is recognized. Included in these publications are a plethora of reports describing only one, or not more than two, patients whose presentation, clinical features, and course differ little from printed material at some prior time. This latter trait was noted in all of our prior editions. We will not reference these numerous case reports unless they contain some information other than the “norm.”
There are 78 metastatic carcinomas of the above type in our 50-year collection of orbital tumors. This is 4.3% (78 out of 1,795) of our total tumors. There were 27 men and 51 women. The predominance of women is due to the frequency of metastases from breast carcinomas. However, if the 37 breast carcinomas are excluded from the calculation, the remaining metastatic carcinomas occur predominantly in men in a ratio approximating 2:1 (32 men and 15 women). In the time interval of our study (1948 to 1997), we have referenced 15 sites of origin of these metastatic carcinomas including prostate, urinary bladder, intestine, breast, gallbladder, adrenal gland, lung, thyroid, pancreas, liver, thymus gland, kidney, cervix, urachus, and ovary.
Blepharoptosis of the upper eyelid associated with diplopia, due to a definite impairment of ocular motility, are the initial signs and symptoms at the time of presentation of these carcinomas. These features emphasize the frequent lodgement of the itinerant neoplasm in or adjacent to the extraocular muscles. Because of their excellent blood supply, these muscles are a logical location for hematogenous metastasis. Proptosis soon follows, but it is relatively slight (2 or 3 mm) compared to the marked disturbances of motility.
At this stage, pain or headache is absent in about half the cases. If pain is present, it is probably indicative of bone destruction. The pain is nagging in character. If pain is associated with visual loss, it is probably due to a tumor in the orbital apex, compressing the optic nerve, or retrobulbar space. Other signs and symptoms such as pulsation of the eye, enophthalmos, afferent pupillary defect, numbness, or paresthesia, and epiphora are infrequent.
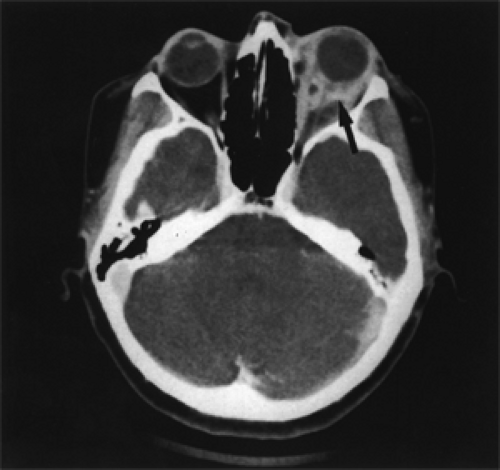
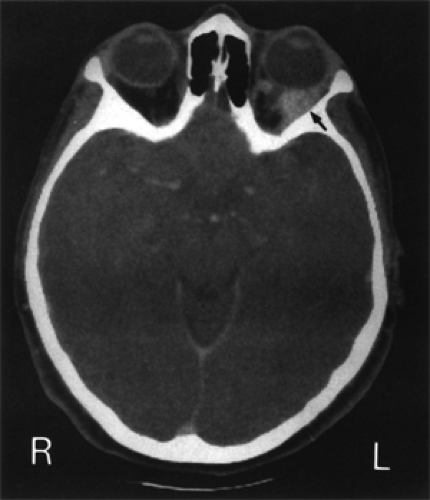
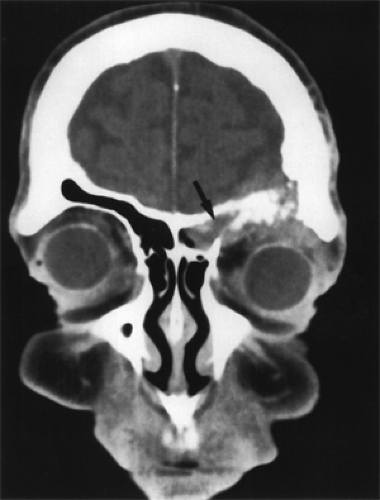
Computed tomography (CT) scan and magnetic resonance imaging will show the size, location, and composition of the neoplasm but are not particularly helpful in differentiating the site of origin of the neoplasm. However, there are some features common to all metastatic carcinomas to the orbit. They all show some degree of enhancement; areas of necrosis may appear as hypodense, and it is unusual to see calcification or cystoid changes.
Carcinoma of the Breast
Of the adenocarcinomas in our 50-year collection, metastasis from the breast is the most common, occurring in 49.3% (39 out of 75) of the total metastases. In four of the women, the metastasis to the orbit was bilateral. The average age of these patients at the time of orbital presentation was 58.9 years. An additional four patients developed bilateral orbital metastasis in the course of the disease. Therefore, 21.6% (8 out of 37) of the total patients had bilateral metastasis some time in the course of the disease.
Breast carcinoma is noted for the time lapse between recognition of the primary tumor and its metastasis. Excluding the four patients in whom the primary carcinoma was not recognized until orbital presentation, there are 33 patients in the Mayo Clinic series for whom the interval from diagnosis of the primary lesion and orbital metastasis is known. In this subgroup, the mean was 5.9 years, and the median was 4 years (range 3 months to 27 years). In a similar analysis of ten patients (Bullock and Yanes, 1980) with orbital metastasis from breast carcinoma, the interval averaged 6.5 years (range 2 to 15.3 years).
In this same field, Reeves et al. (2002) report a case with an unusual twist. At 50 years of age, the patient had a uterine metastasis of unknown origin. Eleven years later, she presented with an orbital metastasis of breast origin. A retrospective analysis of the uterine metastasis and orbital metastasis showed they were identical, but
the carcinoma in the breast was not palpable over the interim 11 years. Eight years after her orbital presentation, a resection of a metastatic adenocarcinoma of the colon was performed which proved to be another metastasis of the lobular carcinoma of the breast. In the case of Saitoh et al. (1997) the patient had a metastasis to both eyelid and orbit 8 years after mastectomy for breast carcinoma.
the carcinoma in the breast was not palpable over the interim 11 years. Eight years after her orbital presentation, a resection of a metastatic adenocarcinoma of the colon was performed which proved to be another metastasis of the lobular carcinoma of the breast. In the case of Saitoh et al. (1997) the patient had a metastasis to both eyelid and orbit 8 years after mastectomy for breast carcinoma.
In four of our patients, enophthalmos rather than exophthalmos was the clue to an orbital metastasis, usually a scirrhous type of an adenocarcinoma.
The carcinoma infiltrates the extraocular muscles. The muscles undergo fibrosis, atrophy of the surrounding orbital fat occurs, and ocular motility becomes so limited that the affected eye becomes fixed and frozen in forward gaze. The eye is so immobile that diplopia may not be present in some cases. One of these four patients thought one of her eyes was too prominent, a pseudoproptosis, (see Fig. 17.1) and was not aware of the enophthalmos of the other eye. Smith et al. (2001) report a sad case of a tethered, sunken eye in a 76-year-old woman heralding a widespread metastasis of a breast carcinoma. Eight years previously, she had had the primary carcinoma treated by wide excision, radical radiotherapy to the breast, axilla, and supraclavicular lymph nodes; and tamoxifen 20 mg daily for 2 years. Alas, the heroic therapy given to the patient was all of no avail.
Enophthalmos associated with metastatic scirrhous adenocarcinoma from the bladder and intestinal tract also occurs (vide infra).
Chandran and Lee (1998) report an interesting case of a 38-year-old woman with a history of breast carcinoma who developed increasing levels of tumor marker CA 15.3. Ten months later, visual loss, diplopia, and blepharoptosis occurred in one eye due to a metastatic adenocarcinoma in the right cavernous sinus and superior orbital fissures. She was treated with surgery and radiotherapy and did well. The authors think that physicians should be aware of the significance of increasing levels of tumor markers as a precursor sign of possible metastasis.
Sekundo and Vogel (1997) report an intriguing case of a 54-year-old woman with a metastatic orbital carcinoma from the breast. Unlike the primary tumor, the metastatic tumor was repeatedly negative for estrogen and progesterone receptor markers. Because the primary tumor was positive for these hormone receptors, the patient was treated by chemotherapy and tamoxifen. The follow-up supported a favorable effect of this adjuvant hormone therapy.
CT scan (see Figs. 17.2 and 17.3) shows several nonspecific features of metastatic breast carcinoma.
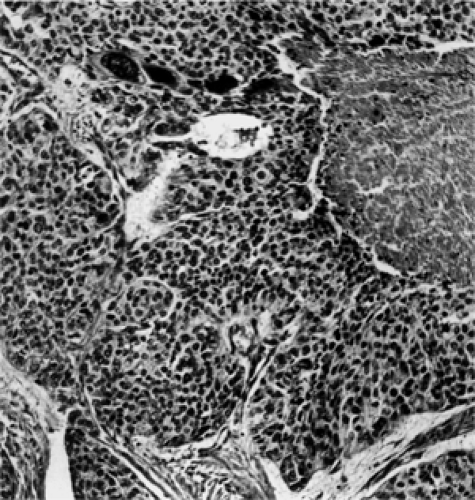
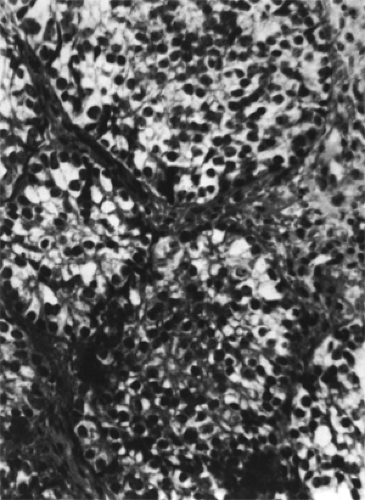
The histopathology of adenocarcinoma of the breast varies. Some may be differentiated into papillary-like growths that remain confined to intraductal, glandular units. Others may appear as a straightforward mucinous type of carcinoma. Still others show a histiocytoid pattern with the cells interspersed in a fibrous tissue stroma. The histiocytoid cells have atypical hyperchromatic nuclei and cytoplasmic, mucin-positive vacuoles. However, by the time the neoplasm has reached the orbit, the original features of the tumor have been replaced by undifferentiated, anaplastic cells that may show a “single-file” infiltration of orbital fat or densely packed cellular lobules of neoplasm. All of the neoplasms in the Mayo Clinic series except
two were anaplastic (grade 3 or grade 4) neoplasms (see Fig. 17.4).
two were anaplastic (grade 3 or grade 4) neoplasms (see Fig. 17.4).
Of our total 37 patients, 30 patients have died of their tumor, four patients are living with tumor, one patient was lost to follow-up, and in two patients the cause of death is not known. The average survival from the time of orbital metastasis was 31 months with a median of 19 months (range 1 to 116 months). On this basis, orbital metastasis can be considered an omen of doom.
Three of the four living patients have survived only 68 months, 15 months, and 13 months, respectively, from the time of orbital metastasis. In the fourth living patient, diagnosis of the primary carcinoma and its orbital metastasis was concurrent. This patient has survived 76 months from diagnosis. The interval of survival from the time of orbital metastasis in these four patients is still in the risk interval of death from tumor based on the course of the 30 patients with tumor-related deaths.
The survival data given above do not support the concept of surgical removal of an orbital metastasis although it is an initial and apparently isolated focus of disease. Unmanageable pain may be the only reason for surgical intercession. The best management option is probably orbital radiotherapy for its palliative effect. Patients whose tumor shows a positive estrogen receptor assay may also be responsive to hormone therapy with increased survival when compared to tumors with a negative estrogen receptor assay.
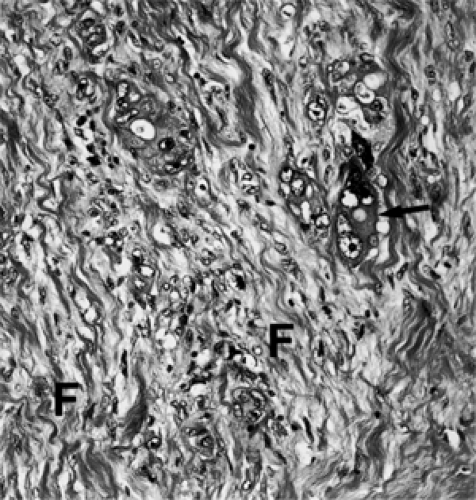 Figure 17.4 Metastatic adenocarcinoma (breast): Metastatic tumor cells (arrow) with fibrosis (F) (× 250). |
In the past decade, an antiestrogenic agent, tamoxifen, has come into widespread use as a systemic adjuvant therapeutic agent for postmenopausal women with breast carcinoma. It is most effective on adenocarcinoma, which has a positive estrogen receptor assay. Controlled studies, over a 10-year period, have provided patients with a longer, nonrecurrence survival interval when compared to patients treated prior to tamoxifen therapy.
Carcinoma of the Lung
This neoplasm is second to carcinoma of the breast in the frequency of metastasis to the orbit. However, in respect to metastasis, the carcinoma of the lung differs in its predilection for men, occurs at a younger age (age range 34 to 80 years, average 51), and is more aggressive than the breast carcinoma. Dissemination from the lung may occur so early in the tumor’s growth that a metastatic focus may precede the discovery of the primary neoplasm. In 6 of 11 cases in the Mayo Clinic series, orbital metastasis was the initial symptom of the silent primary in the lung.
The orbital presentation usually is more fulminant than most of the metastatic tumors in this chapter. Rapidly evolving proptosis is usually the predominant presenting sign. In 7 of 11 patients, orbital symptoms and signs were 3 months or less in duration at the time of presentation.
In the remaining four patients, the longest interval before presentation was 6 months. In one patient, a unilateral proptosis of 10 mm developed over a 3-month period. The orbital manifestations may appear so acute in some cases that the patient is treated for an acute inflammatory process (see Fig. 17.5). Spaide et al. (1989) also reported a patient of this type. Another patient presented with bilateral orbital masses but proptosis of only one eye. Neither enophthalmos nor the “frozen” fixed eyes are seen with metastasis of lung carcinomas as against metastatic breast carcinomas.
In the remaining four patients, the longest interval before presentation was 6 months. In one patient, a unilateral proptosis of 10 mm developed over a 3-month period. The orbital manifestations may appear so acute in some cases that the patient is treated for an acute inflammatory process (see Fig. 17.5). Spaide et al. (1989) also reported a patient of this type. Another patient presented with bilateral orbital masses but proptosis of only one eye. Neither enophthalmos nor the “frozen” fixed eyes are seen with metastasis of lung carcinomas as against metastatic breast carcinomas.
Carcinoma of the lung is an inclusive term for several histologic types regardless of their specific site. The three principal cytologic types are adenocarcinoma, squamous cell carcinoma (see Fig. 17.6), and undifferentiated carcinoma (see Fig. 17.7). The undifferentiated type is also called small cell. In 11 cases of the Mayo Clinic series, there were five adenocarcinomas, four small cell, and two squamous cell types. Each of these cell types responds differently to current chemotherapeutic regimens (vide infra).
Life expectancy in 7 of our 11 patients was nearly as short as the temporal aspects of their presentation. Death occurred from 1 to 26 months after orbital presentation. The mean was 9 months. No follow-up data were available in the remaining four patients. Radiotherapy and the chemotherapy programs in use at the time these patients were first seen were of no avail. However, none of these patients were treated in a time frame corresponding with recent programs of combined chemotherapy (vide infra).
DeLeo et al. (1979), working with immunized mice, produced an antigen, which they thought was associated with malignant transformation, and termed p53. Gradually, it was recognized that cancer patients developed antibodies to this tumor suppressor antigen. Currently, these antibodies are almost exclusively associated with a diagnosis of cancer (Campling and El-Deiny, 2003).
The latter authors have extensively studied and reviewed the literature pertaining to the possible role of gene p53 in
the diagnosis, management, and prognosis of lung cancers. The following generalities are taken from their publication.
the diagnosis, management, and prognosis of lung cancers. The following generalities are taken from their publication.
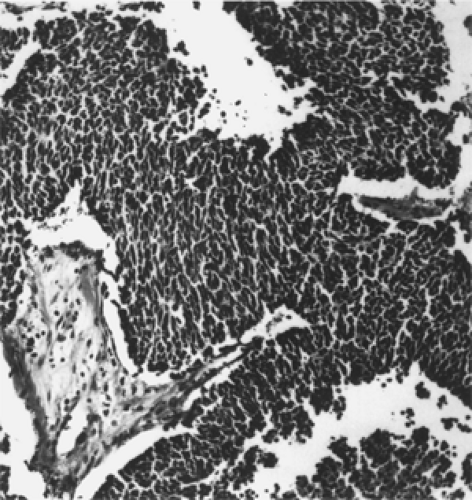 Figure 17.7 Metastatic carcinoma (lung), small cell (oat cell) type: Sheets of small cells resemble an undifferentiated retinoblastoma (× 100). |
In 1989, a study of 30 lung cancer cell lines indicated that p53 was frequently mutated or inactivated in all major types of lung cancer (Takahashi et al., 1989).
The frequency of p53 mutations is highest in squamous cell carcinoma and lowest in adenocarcinomas among non-small cell lung cancer (NSCLC) surgical samples.
A study of patients with alterations in p53 by immunohistochemistry or molecular analysis has not been completed, and the effect on prognosis is still not definitely settled. However, most of the evidence indicates that alterations in p53 are associated with a poor prognosis in NSCLC patients.
The presence of p53 antibodies in a person without a diagnosis of cancer should prompt a search for a primary tumor.
Chemotherapy is the major modality of treatment of small cell lung cancer (SCLC) and plays a significant role in treatment of locally advanced NSCLC as well as palliative therapy of metastatic NSCLC.
SCLC usually responds dramatically to chemotherapy and radiotherapy but frequently recurs and is resistant to further treatment (Murren et al., 2001).
Although NSCLC tumors often respond to chemotherapy and radiation, the responses are usually not as dramatic as for SCLC (Ginsberg et al., 2001).
Carcinoma of the Prostate Gland
This carcinoma is third in frequency of metastasis to the orbit. Metastases occur in 70% to 90% of patients with prostatic cancer (Boldt and Nerad, 1988). The route of metastasis to the orbit is either through the lung or the prevertebral venous plexus.
Patients with orbital metastasis are older than patients with other types of metastatic carcinoma. The age range of our seven patients was 61 to 85 years of age with a mean of 68.8 years. This figure is closely akin to the mean age, 70.1 years, reported by Boldt and Nerad in a larger series of prostatic carcinomas. The mean age of our patients is a decade older than the mean age, 58.9 years, of our group of patients with breast carcinoma.
Prostatic carcinoma also differs, in some respects, from other metastatic carcinomas in its orbital presentation. In addition to the usual signs and symptoms of proptosis, impairment of ocular motility, and visual loss, the patient will frequently have weight loss, nocturia, and pain. The latter is caused by orbital bone metastasis. Two of our patients also had jaundice, a sign of widespread metastasis. The prostate specific antigen level also will be markedly elevated.
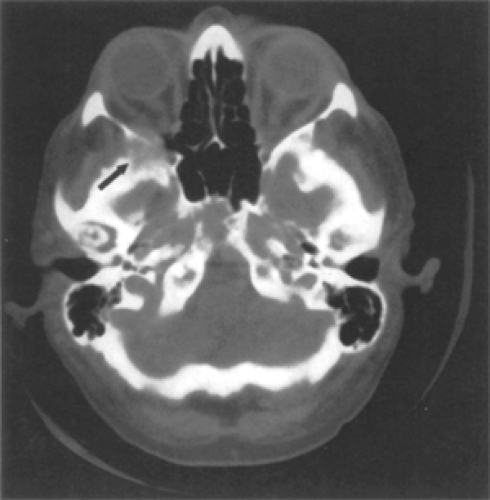
Prostatic carcinoma also has a tendency to metastasize to orbital bone more often than soft tissues. The lesion in bone may be osteolytic or osteoblastic in type, more often the latter. The osteoblastic type may simulate the imaging features of a meningioma, particularly when the greater wing of the sphenoid bone is affected (see Fig. 17.8).
Green et al., 1995, describe a case with bilateral orbital metastasis. Histopathologically, the tumor is an adenocarcinoma but may vary widely from a poorly differentiated to a well-differentiated neoplasm (see Fig. 17.9). The neoplasms have variable cellular patterns including cords, islands, cribriform arrangements of pseudoglandular or glandular patterns with or without intracytoplasmic vacuoles of mucin and some degree of desmoplasia. The tumor cells show nuclear enlargement, contour irregularity, hyperchromasia, and prominent nucleoli. Numerous mitoses may vary according to the degree of differentiation.
Raghavan (2003) includes a subset of eight pages on hormone therapy for prostate cancer. Raghavan has reviewed the literature and analyzed numerous group studies, which have searched for therapies adjuvant to the conventional radical prostatectomy and/or orchiectomy combined with radiotherapy, which might prolong the survival of patients with prostatic carcinoma.
Raghavan notes that the cure rate of early stage carcinoma by conventional local treatment (radical radiotherapy, radical prostatectomy) is <40%. However, 20% to 25% of new cases have advanced degree of carcinoma at the time of presentation. Orbital metastasis would be
considered an advanced degree. Many other authors have noted that patients with advanced carcinoma are less responsive to therapy when compared to patients with early discovery of the neoplasms. This fact is attributed to the heterogeneity of the neoplasm. In brief, not all prostatic carcinomas are alike.
considered an advanced degree. Many other authors have noted that patients with advanced carcinoma are less responsive to therapy when compared to patients with early discovery of the neoplasms. This fact is attributed to the heterogeneity of the neoplasm. In brief, not all prostatic carcinomas are alike.
According to Raghavan, various authors, over the past 15 years, have demonstrated “coincidental” subpopulations of cells with classical adenocarcinomatous features intermingled with cells that exhibit neuroendocrine differentiation, features of small cell undifferentiated carcinoma, and even cells that actually represent transitional cell carcinoma. It, therefore, has seemed unlikely that any one procedure would control these disparate cell populations, at least in the setting of advanced disease. “The possible role of genetics in this confused puzzle is still to be resolved.”
Therefore, most oncologists now direct combination therapy to patients with early stage disease. For patients with metastasis, therapy, at best is only palliative.
Carcinoma of the Kidney (Hypernephroma)
This carcinoma is the most common neoplasm of the kidney in adults. It is interesting to observe the unpredictable course of this lesion when compared to the more predictable behavior of the preceding neoplasms in this chapter. The renal cell tumor is basically an adenocarcinoma.
In our 50-year series of consecutive orbital tumors, there are six men, age range 46 to 80 years with a mean of 61.5 years. Most authors have noted a male predominance. Parnes et al. (1993) state the neoplasm “typically” occurs in men between the ages of 30 and 60 years. Nevertheless, Clinton-Thomas and Robinson (1956) reported the tumor in a 10-year-old girl.
Some cases have an unusual twist in the interval of years between either the recognition or treatment of the primary tumor and the first metastasis. In the case of Kindermann et al. (1981), orbital metastasis did not occur until 15 years after nephrectomy. In the case of Mezer et al. (1997), this interval was 7 years. Metastatic lesions have occurred 10 to 20 years after removal of the primary tumor, Woody and Geeraets (1966). The most frequent sites of metastasis are lung, liver, and bone. Orbital metastasis is less frequent but, when and if it occurs it is an ominous sign. In cases where the orbit is the initial sign of metastatic disease, 25% to 30% of cases will have multiple metastases and widespread disease, the latter remaining asymptomatic. Metastases in three of our six patients were unusual in that both brain and orbit were involved simultaneously.
Contrary to a diffuse pattern of metastasis in most other carcinomas, the renal cell carcinoma is a circumscribed, solitary, soft tissue mass with or without bone involvement. If there is no bone destruction, the retro-orbital carcinoma may be relatively asymptomatic. However, if the lesion is also osteolytic, the patient will have pain.
The soft tissue type metastasis, on CT scan, will probably appear as a well-circumscribed, homogenous mass. The metastasis associated with bone destruction will appear infiltrative, with less homogeneity (see Fig. 17.10).
The neoplasm is a type of adenocarcinoma arising either from renal tubules or from islets of nephrogenic tissue that have persisted in the renal cortex. The tumor cells are large and round with a clear vacuolated cytoplasm (see Fig. 17.11).
The cells proliferate in sheets, cords, or tube-like structures, which are compartmentalized by delicate collagen septae. There are relatively few vessels. Nuclei are vesicular, round to oval, with pleomorphism and relatively frequent mitoses. A pseudocapsule may surround the solitary, solid metastatic tumor.
All six patients in the Mayo Clinic series died of tumor on an average of 51 months (range 28 to 97 months) from the diagnosis of the primary tumor and an average of 25 months (range 1 to 97 months) from the time of orbital metastasis. Only one of these patients had a circumscribed, soft tissue metastasis without bone involvement. This mass was removed intact but had no effect on survival. All other patients had cases of bone destruction. The soft tissue component of the metastasis was simply debulked.
We have found in the literature a remarkable description of a 50-year-old man (Bersani et al., 1994) whose management included many of the unpredictable features of this neoplasm noted in the prior paragraphs. A summary follows:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree