Purpose
To assess the clinical outcomes and complications of shield ulcers by various treatment methods.
Design
Retrospective, interventional case series.
Methods
setting : Cornea and anterior segment service of L.V. Prasad Eye Institute, India. study population : One hundred ninety-three eyes of 163 patients clinically diagnosed with vernal keratoconjunctivitis and shield ulcers. intervention : The treatment algorithm was based on the Cameron clinical grading of shield ulcers. Grade 1 ulcers received medical therapy alone. Grade 2 and grade 3 ulcers received either medical therapy alone or medical therapy combined with debridement, amniotic membrane transplantation (AMT), or both. main outcome measures : Re-epithelialization time and best-corrected visual acuity.
Results
Grade 1 ulcers were seen in 71 (37%) eyes, grade 2 ulcers were seen in 79 (41%) eyes, and grade 3 ulcers were seen in 43 (22%) eyes. In the grade 1 group, re-epithelialization was seen in 67 (94%) eyes. In the grade 2 group, re-epithelialization was seen in 36 (88%) eyes that received medical treatment, in 20 (95%) eyes that underwent debridement, and in 17 (100%) eyes that underwent AMT. In the grade 3 group, re-epithelialization was seen in only 1 (1.7%) eye that received medical treatment, whereas it was seen in all eyes that underwent debridement and AMT. The mean best-corrected visual acuity after re-epithelialization of the shield ulcer was 20/30, 20/30, and 20/40 in the grade 1, grade 2, and grade 3 groups, respectively. Recurrence and secondary bacterial keratitis were seen in 28 (14.5%) and 20 (10%) eyes, respectively.
Conclusions
Grade 1 shield ulcers respond well to medical therapy alone, whereas grade 2 ulcers occasionally may require additional debridement or AMT. Grade 3 ulcers, however, largely are refractory to medical therapy and require debridement and AMT for rapid re-epithelialization.
Vernal keratoconjunctivitis (VKC) is a chronic bilateral allergic inflammation of the ocular surface, characterized by conjunctival hyperemia, chemosis, photophobia, intense itching, pseudoptosis, filamentous mucous discharge, or a combination thereof. It may be seasonal or perennial (23%) and usually is seen in young boys in the first decade of their life. VKC can present either in the palpebral form (giant papillary hypertrophy of the upper tarsal conjunctiva) or bulbar form (Tranta dots aggregates of epithelial cells and eosinophils) or a mixed form. Complications of VKC can be either disease related (shield ulcer, corneal scarring, dry eye, limbal stem cell deficiency) or treatment related (steroid-induced cataract and glaucoma).
Shield ulcer is a shallow indolent ulcer usually seen on the upper part of the cornea and takes months to re-epithelialize, depending on the severity. Two hypotheses have been proposed for the pathogenesis of shield ulcers. The mechanical hypothesis states that the corneal surface is abraded by the giant papilla on the upper tarsal conjunctiva, which explains the predilection of these ulcers to appear in the superior part of cornea. The toxin hypothesis states that the inflammatory mediators from the eosinophils induce corneal epithelial damage. Through either of the above mechanisms, initial corneal damage is manifested as coarse punctate epithelial keratopathy, which is converted to corneal ulcers by the mechanical friction of the giant tarsal papillae. A dense plaque is formed over this ulcer by the deposition of toxic eosinophilic granule major basic protein, secreted by activated eosinophils, which is cytotoxic and delays re-epithelialization. Delayed epithelial healing may lead to secondary infections, strabismus, amblyopia, and corneal perforation. Several treatments have been used in various combinations to achieve rapid re-epithelialization, such as medical treatment (with corticosteroids, nonsteroidal anti-inflammatory drugs, antiallergic medications, cyclosporine), temporary mattress sutures to the lids, debridement, superficial keratectomy, amniotic membrane transplantation (AMT), resection, and cryotherapy, combined with AMT for giant papillae and excimer laser phototherapeutic keratectomy. In 1995, Cameron proposed a classification system for diagnosing, managing, and prognosticating shield ulcers based on the clinical features, which is the largest series (66 cases) published to date in the ophthalmic literature. In this article, we describe the clinical outcomes of 193 eyes of 163 patients with shield ulcers treated with different methods.
Methods
Patients
The Institutional Review Board of L. V. Prasad Eye Institute approved the retrospective review of this data, and the study adhered to the tenets of the Declaration of Helsinki. A review of medical records of all patients clinically diagnosed to have VKC, shield ulcers, or both at the Cornea and Anterior Segment Service from January 2000 through December 2009 was performed. Patients included in the study were: those with a documented clinical history of itching, photophobia, filamentous mucous discharge, and characteristic signs of cobble stone papillae of more than 1 mm on the upper tarsal conjunctiva with no limbal infiltration (palpebral type), papillae of less than 1 mm on the upper tarsal conjunctiva with limbal infiltration (limbal type), and a mixed form (features of both palpebral and limbal types) of VKC; patients with VKC and epithelial defect on fluorescein staining with or without inflammatory deposit or elevated plaque; and patients with regular weekly follow-up visits until the resolution of the epithelial defect on fluorescein staining. Patients with a previous history of any corneal surgery, patients not compliant with medications, patients who did not comply with follow-up at regular weekly intervals until re-epithelialization, and patients with untreated concurrent problems that would affect re-epithelialization were excluded from the study. However, these excluded patients were included only for estimating the incidence and seasonal variation of shield ulcers.
Data Collection
The following data were retrieved from the medical records: age, gender, duration of VKC, duration of present symptoms (exacerbation), history of atopy, signs of VKC, location, laterality, grade and size of shield ulcer, medications used, surgical details, time for re-epithelialization, Snellen best-corrected visual acuity (BCVA) at presentation and after re-epithelialization, complications, microbiologic profile, and duration of follow-up.
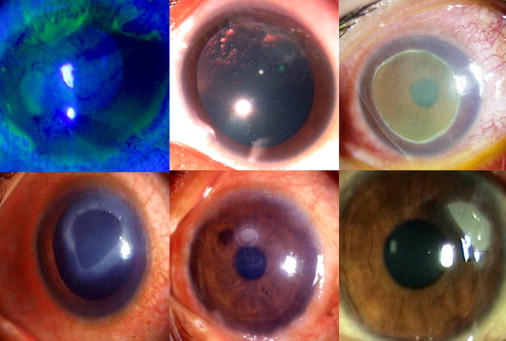
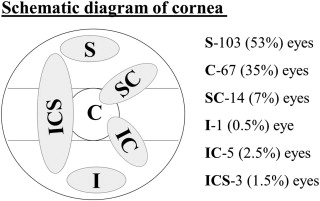
The Cameron grading system is as follows: grade 1, transparent base; grade 2, translucent base with or without opaque white or yellow deposits; and grade 3, elevated plaque used for shield ulcers ( Figure 1 ). The location of the shield ulcer was determined from the schematic diagrams from the medical records ( Figure 2 ). The cornea was divided into superior, central, and inferior sectors by 2 horizontal lines passing above and below the central 4 mm area. Shield ulcers located above the superior horizontal line were segregated as only superior, ulcers below the inferior horizontal line were segregated as only inferior, ulcers between the 2 horizontal lines were segregated as central, ulcers either superior or inferior and encroaching on some part of the central area were noted as superior-central or inferior-central, and ulcers with some part encroaching on all the 3 areas were graded as inferior-central-superior. The size of the ulcer was assessed by measuring the longest dimension and the longest perpendicular to the first measurement in millimeters.
Interventions
Depending on the grade of the shield ulcer, treatment was advocated as either only medical (sodium cromoglycate 2% or 4% eye drops twice daily; topical corticosteroids: prednisolone acetate 1% or fluorometholone ophthalmic suspension 0.25% in patients with glaucoma 4 to 8 times daily depending on the severity of VKC; antibiotic eye drops 4 times daily; and lubricating eye drops 6 to 8 times daily), medical treatment combined with debridement, or medical treatment combined with AMT. The patients were followed up at weekly intervals until re-epithelialization. For patients who did not show signs of re-epithelialization (decrease in size of epithelial defect of at least 1 mm from the baseline) within 2 weeks, with primary treatment, AMT was carried out. Debridement was carried out either at the slit lamp (topical proparacaine 0.5% ophthalmic solution) or in the operating room (under peribulbar or general anesthesia) by scraping of the base and margin of the ulcer using a no. 15 surgical blade on a Bard Parker handle (Aspen Surgical, Caledonia, Michigan, USA). AMT was carried out in the operating room (under peribulbar or general anesthesia) after debridement or superficial keratectomy, either by using 10-0 monofilament nylon interrupted sutures or fibrin glue (Tisseel Kit; Baxter AG, Vienna, Austria; Figure 3 ). We used AMT in all the cases that required secondary intervention. Superficial keratectomy was carried out by using either a crescent blade (Alcon Surgical, Fort Worth, Texas, USA) or a no. 15 surgical blade on a Bard Parker handle when only debridement failed to remove the inflammatory debris or plaque.
After debridement or AMT, 0.5 ml supratarsal dexamethasone sodium phosphate (4 mg/mL), or triamcinolone acetonide (40 mg/mL) was administered in eyes with palpebral and mixed forms of VKC based on severity. Patients with pain and suspicious clinical signs (collagenolysis and hypopyon) underwent debridement and microbiological work-up. The samples obtained using a No. 15 surgical blade on a Bard Parker handle were sent for direct smear examination (Gram’s, Giemsa, and potassium hydroxide) and culture examination. The samples were inoculated directly onto blood agar, chocolate agar, nonnutrient agar with Escherichia coli overlay, Sabouraud dextrose agar, potato dextrose agar, thioglycollate broth, and brain heart infusion broth. The treatment of these patients was modified based on smear and culture results. Preparation and preservation of the amniotic membrane was carried out following the standard method as previously described.
Main Outcome Measures
Corneal re-epithelialization time and BCVA after re-epithelialization in every subgroup of shield ulcers and after different interventions were the primary outcome measures. Re-epithelialization was defined as absence of an epithelial defect (fluorescein staining) as depicted in the chart diagram at the latest visit. The secondary outcome measures were complications including recurrence and microbial keratitis.
Results
Demographics
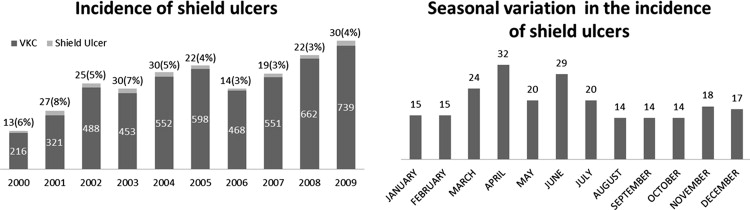
The baseline clinical characteristics are summarized in Table 1 . During the study period, the overall incidence of shield ulcers was 4.6% and the annual incidence ranged from 3% to 8% ( Figure 3 , Right). A total of 193 eyes of 163 patients were included in the study. Of these, 71 eyes had grade 1 shield ulcer, 79 eyes had grade 2 shield ulcer, and 43 had grade 3 shield ulcer or plaque. All grades showed a male predominance (males, 89% [145/163]; females, 11% [11/163]). Bilateral shield ulcers were seen in 18% (30/163) of patients, of whom 53% (16/30) had simultaneous bilateral shield ulcers. Simultaneous bilateral similar-grade shield ulcers were seen in 87.5% (14/16) of patients. (grade 1 in 6, grade 2 in 4 and grade 3 in 4) Of the nonsimultaneous shield ulcers, 43% (6/14) were of a different grade. The mean interval between shield ulcers in nonsimultaneous eyes was 44 weeks (range, 6 to 166 weeks). The size of the shield ulcers at presentation varied from 0.5 × 1 mm to 6.5 × 7.7 mm in the grade 1 group, 0.5 × 1 mm to 4.5 × 7.2 mm in the grade 2 group, and 1 × 1.5 mm to 4.8 × 9 mm in the grade 3 group. History of atopy was seen in 13 patients (8%; asthma, n = 9; atopic dermatitis, n = 4) patients. The mean duration of VKC before presentation was 30 months (median, 24 months; range, 1 to 180 months). The mean duration of symptoms of present exacerbation was 40 days (median, 27 days; range, 1 to 365 days).
| Feature | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|
| Mean age (median, range), y (n = 163) | 14 (13, 3 to 36) | 12 (10, 3 to 26) | 13 (12, 2 to 26) |
| Mean duration of VKC (median, range), mos | 30 (12, 1 to 180) | 28 (24, 2 to 120) | 32 (36, 2 to 84) |
| Mean duration of present exacerbation of symptoms (median, range), d | 36 (30, 3 to 150) | 38 (15, 1 to 365) | 46 (20, 3 to 65) |
| Type of VKC (P/M/L) | 53/14/4 | 51/28/0 | 24/18/1 |
| Epithelial defect size geometric mean (mm) | 2.24 | 3.14 | 5.45 |
Re-Epithelialization Time
The management and follow-up details are presented in Table 2 . The mean total follow-up period was 544 ± 751 days. The primary treatment for all patients with grade 1 shield ulcer was only medical. Re-epithelialization was seen in 94% eyes with a mean resolution time of 17 days. Four eyes (6%) in which the disease did not resolve with the primary medical treatment progressed to grade 2 ulcers and showed complete re-epithelialization with a mean duration of treatment of 11 ± 7 days after AMT. Five (12%) eyes in the grade 2 group, 5 (83%) eyes in the grade 3 group receiving only medical treatment, and 1 eye in the grade 2 group receiving debridement did not show signs of re-epithelialization in 2 weeks, but showed complete re-epithelialization with a mean duration of treatment of 11 ± 5 days, 28 ± 13 days, and 34 days after AMT, respectively. Superficial keratectomy was required in 12 eyes with grade 3 shield ulcer. Supratarsal steroid injection was given in 86 eyes, and the mean re-epithelialization time in these eyes was 20 days (median, 14 days; range, 3 to 90 days), which was not different from eyes that did not undergo supratarsal steroid injection.
| Feature | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|
| Method of treatment, n = 193 | |||
| Medical only | 71 | 41 | 6 |
| Debridement | 0 | 21 | 10 |
| Amniotic membrane transplantation | 0 | 17 | 27 |
| Re-epithelialized eyes, n (%) | |||
| Medical only | 67 (94) | 36 (88) | 1 (17) |
| Debridement | NA | 20 (95) | 10 (100) |
| Amniotic membrane transplantation | NA | 17 (100) | 27 (100) |
| Mean time for re-epithelialization ± SD (median, range), d | |||
| Medical only | 17 ± 12 (13, 3 to 47) | 22 ± 15 (18, 4 to 58) | 20 |
| Debridement | NA | 21 ± 16 (14, 7 to 67) | 19 ± 11 (14.5, 10 to 46) |
| Amniotic membrane transplantation | NA | 21 ± 18 (20, 5 to 80) | 23 ± 19 (15.5, 5 to 90) |
| Supratarsal steroid injection (no. of eyes) | 17 | 35 | 34 |
| Recurrence, no. of eyes (%) | 17 (24) | 10 (13) | 6 (14) |
| Mean follow-up after re-epithelialization of last shield ulcer | 1 y, 4 d | 1 y, 5 mos, 16 d | 1 y, 4 mos |
| Mean total follow-up | 1 y, 6 mos, 5 d | 1 y, 6 mos, 5 d | 1 y, 4 mos, 24 d |
| Mean BCVA at presentation (median, range) | 20/40 (20/40, 20/20 to 20/1600) | 20/40 (20/40, 20/20-20/160) | 20/125 (20/60, 20/20-20/2000) |
| Mean BCVA after re-epithelialization (median, range) | 20/30 (20/25, 20/20 to 20/200) | 20/30 (20/25, 20/20 to 20/1143) | 20/40 (20/25, 20/20 to 20/200) |
Vision
The mean BCVA at presentation and after re-epithelialization of shield ulcers was 20/40 and 20/30, respectively, in grade 1; 20/40 and 20/30, respectively, in grade 2; and 20/125 and 20/40, respectively, in grade 3. The mean BCVA for ulcers involving the central part of the cornea was 20/40, which was slightly worse as compared with ulcers not involving the central cornea (20/30). The mean BCVA in patients with only medical treatment was 20/25, compared with the eyes that received surgical intervention (20/30). The mean BCVA in patients who showed re-epithelialization with primary intervention was 20/30 and was 20/50 in patients who required secondary intervention. Twenty-five eyes (13%) lost 1 or more Snellen lines at the final visit. Eight (32%) of these eyes had some part of the ulcer located centrally, 5 (20%) eyes had recurrent shield ulcer, and 2 (8%) eyes had coexisting bacterial keratitis.
Complications
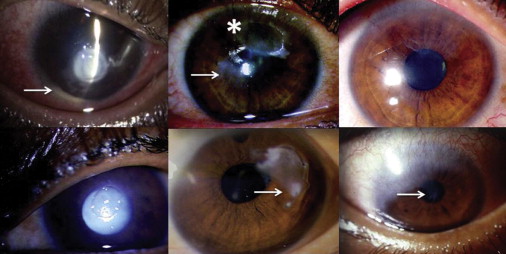
Coexisting bacterial keratitis was seen in 1, 9, and 10 eyes in the grade 1, grade 2, and grade 3 groups, respectively ( Figure 4 , Top left). On microbiologic evaluation, 4 eyes demonstrated positive results only on smears (gram-positive cocci) and were treated with broad-spectrum antibiotics. The culture positive cases with organisms like Staphylococcus epidermidis (n = 5), Streptococcus pneumonia (n = 4), Corynebacterium species (n = 2), Neisseria meningitides (n = 1), Klebsiella pneumonia (n = 1), and Brevibacterium species (n = 1) or with polymicrobial results ( Haemophilus species and Pseudomonas aeruginosa , n = 1; α-hemolytic Streptococcus and Neisseria species, n = 1) were treated based on sensitivity. Recurrent shield ulcers were seen in 14.5% (28/193) of eyes. Twenty-three eyes had a recurrence only once, and 5 eyes had a recurrence twice. Recurrence was seen at a mean period of 12.5 months (median, 9.8 months; range, 0.8 to 44.9 months) after the re-epithelialization of the primary shield ulcer. The mean re-epithelialization time of recurrent shield ulcers was 24 days (median, 21 days; range, 9 to 62 days; Table 3 and Figure 4 , Top center and Top right). Four patients were lost to follow-up before complete re-epithelialization of the recurrent shield ulcer. At presentation, 10 eyes had a steroid-induced cataract ( Figure 4 , Bottom left), 4 eyes were pseudophakic, and 3 eyes had a history of trabeculectomy ( Figure 4 , Bottom center). Two eyes had glaucomatous optic atrophy at presentation. Partial limbal stem cell deficiency was seen in 10 eyes at the final follow-up ( Figure 4 , Bottom right).
| Case No. | No. of Recurrences | Primary SU (VKC Type/Grade/Management) | Time of Recurrence from Re-epithelialization of Primary SU (y/mos/d) | Recurrent SU (VKC Type/Grade/Management) | Re-epithelialization Time (d) | Follow-up after Re-epithelialization of Recurrent SU (y/mos/d) |
|---|---|---|---|---|---|---|
| 1 | 2 | Mi/1/M Mi/2/M | 0/2/0 0/11/16 | P/2/AMT P/2/AMT | 14 11 | NA 4/10/17 |
| 2 | 2 | Mi/1/M Mi/1/M | 1/2/14 1/9/23 | P/1/M P/3/AMT | 14 14 | NA 0/11/16 |
| 3 | 1 | Mi/1/M | 2/5/28 | P/2/M | LFU | LFU |
| 4 | 1 | P/1/M | 0/0/28 | P/2/M AMT | 10-NR 12 | 0 |
| 5 | 1 | P/1/M | 0/11/0 | P/2/D | 9 | 0/3/14 |
| 6 | 1 | P/1/M | 0/5/5 | P/3/AMT | 14 | 1/7/23 |
| 7 | 1 | P/1/M | 0/4/0 | P/2/AMT | 14 | 0/8/28 |
| 8 | 1 | P/1/M | 1/10/25 | P/1/M | LFU | LFU |
| 9 | 2 | Mi/1/M Mi/2/M | 0/6/22 | Mi/2/D P/3/AMT | 42 23 | NA 4/7/28 |
| 10 | 1 | P/1/M | 0/6/16 | P/1/M | 21 | 2/9/0 |
| 11 | 1 | P/1/M | 0/6/6 | P/1/M | LFU | LFU |
| 12 | 1 | P/1/M | 0/10/27 | P/3/D | 30 | 0 |
| 13 | 1 | P/1/M | 0/2/24 | P/1/M | 9 | 0 |
| 14 | 2 | P/2/D P/1/M | 0/10/28 | P/1/M P/1/M | 62 21 | NA 0/2/5 |
| 15 | 1 | P/2/M | 0/6/18 | P/3/AMT | 18 | 2/0/0 |
| 16 | 1 | P/2/AMT | 0/1/2 | Mi/1/M | 12 | 0/1/25 |
| 17 | 1 | Mi/2/M | 0/1/17 | P/1/M | 24 | 1/2/3 |
| 18 | 1 | Mi/2/D, infiltrate | 1/11/11 | P/1/M | 30 | 1/0/22 |
| 19 | 1 | Mi/2/AMT | 2/7/19 | P/3/D | 42 | 4/6/16 |
| 20 | 1 | P/2/D | 0/0/25 | P/2/M | 50 | 2/2/6 |
| 21 | 1 | P/2/D | 1/0/0 | P/1/M AMT | 14-NR 12 | NA 0 |
| 22 | 1 | P/2/M | 0/8/0 | Mi/1/M | LFU | LFU |
| 23 | 2 | P/2/D P/1/M | 0/9/28 3/6/5 | P/1/M P/1/M | 30 20 | NA 0 |
| 24 | 1 | Mi/3/AMT | 1/0/25 | P/1/M | 22 | 0/11/27 |
| 25 | 1 | P/3/AMT | 0/11/10 | P/1/M | 45 | 1/2/24 |
| 26 | 1 | Mi/3/AMT | 0/1/26 | Mi/1/M | 9 | 0 |
| 27 | 1 | P/3/AMT | 0/5/16 | P/2/AMT | 42 | 0/10/5 |
| 28 | 1 | P/3/D | 2/5/3 | P/2/M | 22 | 0/3/28 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


