Macular Trauma
Reinaldo A. Garcia Arismendi
Virgil D. Alfaro III
Fernando J. Arevalo
Oria Veronica
Gomez Ulla
Giora Treister
Eye injury is a significant disabling American health problem. The National Research Council reported that “injury is probably the most under-recognized mayor health problem facing the nation today. The study of injury presents unparalleled opportunities for reducing morbidity and for realizing significant savings in both financial and human terms.” Data from the National Center for Health Statistics’ Health Interview Survey, conducted in 1977, estimated that nearly 2.4 million eye injuries occur in the United States annually. This report calculated that nearly one million Americans have permanent significant visual impairment due to injury, with more than 75% of these individuals being monocularly blind. Eye injury is a leading cause of monocular blindness in the United States, and is second only to cataract as the most common cause of visual impairment. A wide variety of direct and indirect closed-globe trauma can affect the posterior segment. In this chapter we will talk about the most important conditions that can affect the posterior segment and the macula.
TRAUMATIC MACULAR HOLE
The first published case of macular hole (MH) in a young man with an eye trauma appeared in 1869 by Knapp (1). In our days traumatic MH formation is a relatively common posterior segment complication of severe contusion injury; trauma itself accounts for up to 9% of eyes that develop fullthickness MHs (2). However, the etiology by which traumatic holes occur is not well understood and despite the large number of publications related to this topic, the cause of MH remains controversial.
Pathogenesis
In the setting of idiopathic MHs, the vitreous is believed to have a crucial role in the pathogenesis. Recent findings suggest that full thickness MHs develop in a situation where there is failure of normal age related separation of the vitreous cortex from the posterior pole as a result of an abnormally tenacious attachment to the fovea. The formation of an idiopathic MH typically occurs over weeks to months. Although some traumatic MHs also occur weeks or months following the trauma, traumatic MHs are typically not associated with a gradual onset.
Many mechanisms such as contusion necrosis, subfoveal hemorrhage, mechanical deformity, and vitreous traction have been considered as possible causes of traumatic MHs, and Ho and associates outlined in 1998 four basic historical theories regarding its cause: the traumatic theory, the cystic degeneration theory, the vascular theory, and the vitreous theory (1). We as others (3, 4 and 5) believe that in those cases in which the traumatic MH is not present initially but develops weeks to months following the incident the mechanism is probably similar to that of idiopathic MHs seen in elderly patients and the contusion and post-traumatic inflammation probably initiates and potentiates the abnormal epiretinal and vitreoretinal contraction. In the case of the MH that forms immediately following contusion injury, rapid changes in the shape of the eye with shortening in the anterior-posterior dimension with equatorial elongation and rebound may result in the rapid creation of anterior-posterior and tangential vitreoretinal traction in the area of the fovea. This acute event in a young patient with an attached posterior hyaloid and rigid internal limiting membrane (ILM) may lead to a small dehiscence of the fovea after trauma (4). Then, the acute transient nature of tangential traction and tissue proliferation, possibly by glial cells or retinal pigment epithelium (RPE) cells, may play an important role in MH closure and may explain the more frequent occurrence of spontaneous reapproximation of the edges of the hole in some cases.
Clinical Presentation
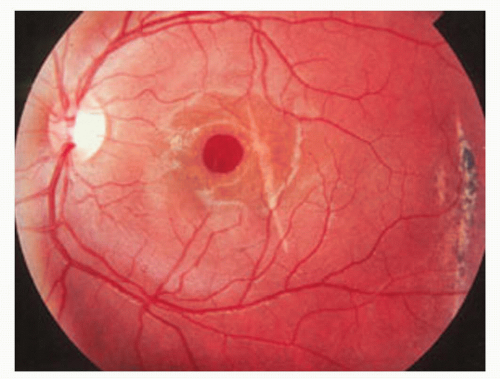
Patients with traumatic MHs tend to be young, and posterior vitreous detachment is typically absent in these eyes. Clinically, visual acuity is usually reduced to 20/80 to 20/400, and biomicroscopic examination typically shows a round, sharply defined hole measuring about 300 to 500 μm with a surrounding cuff of neurosensory detachment; however, in some instances the hole may be larger or show irregular margins (2) (Fig. 46-1). Traumatic damage of the RPE can be associated with traumatic MHs; it is usually manifested as a mottling of the RPE near or within the center of the macula. This potentially has significant importance for vision recovery after trauma and surgical repair (5).
Management
Pars plana vitrectomy (PPV) has demonstrated efficacy and safety for patients with idiopathic MHs however there is no consensus on the operative treatment for this disease, because some cases demonstrate spontaneous closure of the MH and improved visual acuity. Mitamura et al. (6) and Yamashita et al. (7) published the largest series of eleven and eighteen traumatic MHs with spontaneously resolution in 64% and 44% respectively. This result suggests that the spontaneous closure rate is much greater in traumatic MH than in idiopathic MH, although the number of cases reported was small. Common features of patients with spontaneous closure of traumatic MH
were young age, small size of MH, no fluid cuff and no posterior vitreous detachment. Several authors (6,7 and 8) reported that they observed spontaneous MH closure through 1 week to 4 to 6 months after injury. Then, some authors support that an observation for a period of up to four months may be a management of choice for traumatic MH. However, still it is very difficult to decide when to perform vitrectomy, because the longer the delay, the more likely it is that the photoreceptor cells will be damaged. Because vitreous surgery can lead to hole closure with visual improvement in most eyes and the favorable results may probably be related to the younger age of the patients and the shorter duration of the MH, others (9) believe that an observation is probably a dubious initial treatment option, since a conservative approach may lessen the chance of a good anatomical and functional recovery.
were young age, small size of MH, no fluid cuff and no posterior vitreous detachment. Several authors (6,7 and 8) reported that they observed spontaneous MH closure through 1 week to 4 to 6 months after injury. Then, some authors support that an observation for a period of up to four months may be a management of choice for traumatic MH. However, still it is very difficult to decide when to perform vitrectomy, because the longer the delay, the more likely it is that the photoreceptor cells will be damaged. Because vitreous surgery can lead to hole closure with visual improvement in most eyes and the favorable results may probably be related to the younger age of the patients and the shorter duration of the MH, others (9) believe that an observation is probably a dubious initial treatment option, since a conservative approach may lessen the chance of a good anatomical and functional recovery.
Surgical Technique
The surgical technique for traumatic MHs does not differ significantly from the idiopathic hole; however, since most of the patients with traumatic holes are younger, additional considerations are necessary. First, the posterior hyaloid may be more difficult to remove, requiring added manipulations. A few investigators have suggested enzyme assistance using plasmin for these patients (10). Younger patients tend to have more significant intraocular proliferation following trauma or retinal detachment. With this in mind, some authors (3,9) suggests epiretinal dissection or ILM removal in addition to posterior hyaloidal separation. Removal of the ILM surrounding the hole is the only way to ensure complete removal of significant epiretinal proliferation; then ILM removal may be considered as a prophylactic measure against MH reopening. Then, peeling of the inelastic ILM has proven effective and appears indicated for traumatic MHs (3,9) however, aggressive attempts to remove the ILM may result in iatrogenic injury. To facilitate and expedite removal, a dilute concentration if indocyanine green (ICG) dye may be used. Some controversy exists as to the safety of ICG in the posterior segment. Finally, silicone oil has been reported as an alternative to intraocular gas primarily because of the hypothesis that facedown positioning is less important with oil due to its prolonged, complete tamponade effect and secondarily because many of the patients are young and cannot tolerate face down positioning. However, its use does require an additional surgery for subsequent oil removal and may not provide the same efficacy as gas. Some authors believe that the silicone oil may provide less tamponade effect as the MH closes and the foveal region begins to recover the normal foveal depression (11).
In general, the success of surgical treatment in terms of anatomical closure of the traumatic hole and improvement of vision varies by study, but overall appears to be similar to idiopathic MHs (3).
TRAUMATIC MACULAR HOLE-RELATED RETINAL DETACHMENT
The role of vitrectomy surgery for MH-related retinal detachment caused by blunt ocular injury is not well established because of the rarity of the condition. Chen et al. (12) reported eight patients with traumatic MH-related retinal detachment treated with a standard three-port PPV combined with gas tamponade initially or subsequently. Because of the high incidence of peripheral retinal breaks (50%) and in order to avoid any missing breaks and mild anterior proliferative vitreoretinopathy they performed encircling scleral buckle in six selective cases; ILM peeling was done in only two cases. They reported successful retinal re-attachment in seven eyes (87.5%), and the MH was successfully closed in all eyes (100%). They concluded that extent of retinal detachment and presence of peripheral retinal breaks, vitreous hemorrhage, or hyphema had no discernible significant influence on retinal re-attachment rate in patients with MH-related retinal detachment.
COMMOTIO RETINAE (BERLIN’S EDEMA)
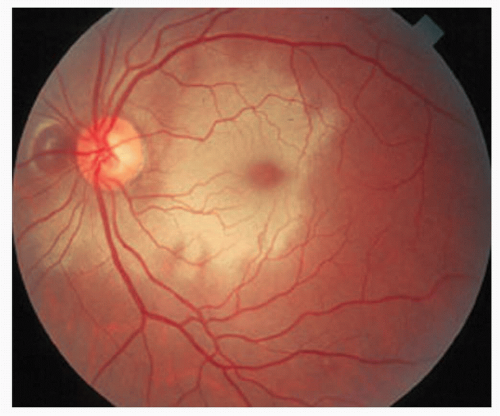
The term Commotio Retinae has been used since 1873, when Berlin described a transient whitening of the retina after blunt trauma to the globe and invoked the Latin term for retinal contusion, Commotion Retinae (13). This condition is typically characterized by transient gray-white discoloration or opacification of the outer sensory retina. The opacification may be confined to the macular area, in which case is referred to as Berlin’s edema, or it can occur peripherally. The symptoms are determined by the location of the lesion. If only the peripheral retina is involved the patient may have no visual complaints. If the posterior pole is affected the patient may report decreased vision but sometimes the lesion may take several hours to be visible ophthalmoscopically. If the entire posterior pole is involved, a pseudo cherry-red spot may be present (Fig. 46-2). As the retinal opacification resolves, vision may return to normal and there may be no ophthalmoscopic findings after the resolution. With more severe blunt trauma, visual loss may persist, and the opacification may be replaced by mottling of the RPE (14).
Pathogenesis
Berlin postulated (13) that extracellular edema resulted in the loss of retinal transparency, and the condition became known as Berlin’s edema. Subsequent histopathologic studies in animals revealed a different pathogenesis. Blight and Hart described marked intracellular edema of the retinal glial elements after trauma induced retinal whitening in pigs. They also found receptor outer segment fragmentation and marked intracellular edema of the RPE using the same pig model (15,16). Sipperly et al. (17) detected disruption of only the photoreceptor outer segment in an owl monkey model. Kohno et al. (18) demonstrated disruption of photoreceptor outer segment in addition to intracellular edema in Muller cells, retinal pigment epithelial cells, nerve fibers, and the outer plexiform layer axons of photoreceptor cells. Mansour et al. (19) in the histopathologic analysis of a single human eye showed the development of clinical commotion retinae within 24 hours of moderately severe blunt trauma. Photoreceptor outer segment disruption and damage to the RPE were noted. These findings, in addition to the aforementioned animal studies, suggest the mechanical disruption at the photoreceptor outer segment-RPE interface is most likely responsible for the gray-white appearance of the retina in commotion retinae. Although some pathology reports of commotio retinae have noted the appearance of fluid-filled spaces in the outer retinal layers, evidence of extracellular edema in commotion retinae has not been consistently found. Finally, Monsour et al. (19) attributed the susceptibility of the outer segments to the architecture of the retina, particularly the Muller cell skeletal system because Muller cells occupy the retina from the ILM to the photoreceptor inner segment and support all cellular layers except the photoreceptor outer segments.