Purpose
To investigate whether lamellar macular holes can be divided into different subgroups.
Design
Retrospective observational case series.
Methods
In this institutional study, clinical charts and spectral-domain optical coherence tomography (OCT) images of 102 eyes of 90 consecutive patients diagnosed with lamellar macular hole were reviewed. In OCT imaging, the presence of lamellar macular hole was defined according to the following findings: presence of irregular foveal contour, separation of the layers of the neurosensory retina, and the absence of full-thickness macular defect. Mean outcome was the morphologic and functional characterization of different subtypes of macular hole.
Results
Two different subtypes of lamellar macular hole were identified: tractional and degenerative. The first type, tractional, was diagnosed in 43 eyes, and was characterized by the schitic separation of neurosensory retina between outer plexiform and outer nuclear layers. It often presented with an intact ellipsoid layer and was associated with tractional epiretinal membranes and/or vitreomacular traction. The second type, degenerative, was diagnosed in 48 eyes, and its distinctive traits included the presence of intraretinal cavitation that could affect all retinal layers. It was often associated with nontractional epiretinal proliferation and a retinal “bump.” Moreover, it often presented with early ellipsoidal zone defect and its pathogenesis, although chronic and progressive, remains poorly understood. Eleven eyes shared common features with both tractional and degenerative lamellar macular holes and were classified as mixed lesions.
Conclusions
Degenerative and tractional lamellar macular holes may be 2 distinct clinical entities. A revision of the current concept of lamellar macular holes is needed.
The diagnosis “lamellar macular hole” currently refers to a retinal condition characterized by a partial-thickness defect of the macula with an irregular foveal contour and separation between outer and inner retinal layers. Distinct from other macular entities like macular hole and macular pseudohole, lamellar macular hole is typically thought of as a lesion with a lamellar loss of foveal tissue causing distortion of foveal architecture.
The concept of lamellar macular hole was first conceived by Gass in 1976. With slit-lamp biomicroscopy, he described an oval reddish macular lesion in pseudophakic patients with cystoid macular edema, and presented histologic evidence of foveal tissue loss. Later, the introduction of optical coherence tomography (OCT) created a transformative shift in our understanding of in vivo macular pathology and became the gold standard for the diagnosis of lamellar macular hole. Recently, spectral-domain technology has replaced time-domain OCT, resulting in dramatically improved resolution and allowing for more detailed analyses of the morphology and evolution of lamellar macular hole.
With improved macular imaging, a precise definition of lamellar macular hole and clear distinction between several other macular conditions such as pseudohole and macular retinoschisis have blurred. Although OCT-based diagnostic criteria have been proposed, the precise defining features and pathophysiology of these conditions remain unresolved.
We hypothesize that the current definitions and terminology may be too broad and may have unintentionally led to misclassification of the entity currently referred to as lamellar macular hole. As a consequence, high levels of heterogeneity, both functionally and morphologically, can be encountered between lesions currently classified as lamellar macular hole. This heterogeneity may also be reflected in the discordant anatomic and visual results within the natural history or after treatment with pars plana vitrectomy and relief of macular traction.
Recently, some have focused attention on the “lamellar hole–associated epiretinal proliferation,” an entity considered to be characteristic of lamellar macular hole. This epiretinal proliferation was initially described as a “thicker” or “dense” epiretinal membrane and was later redefined according to its distinctive properties, like the apparent absence of traction, further suggested by histopathologic analysis.
Due to the anatomic and functional differences between lesions with and without lamellar hole–associated epiretinal proliferation, some authors have suggested that this entity may define a particular subtype of lamellar macular hole.
However, in our view the presence or absence of this peculiar epiretinal proliferation alone is insufficient to classify lamellar macular hole. Firstly, this proliferation is not specific to lamellar macular hole, as it is also observed in eyes with full-thickness macular hole and epiretinal membrane. Secondly, we hypothesize that lamellar macular hole, as currently classified, may represent more than 1 condition with potentially different natural histories and surgical outcomes. Therefore, the purpose of this study was to investigate the anatomic and functional features of eyes classified as having a lamellar macular hole.
Methods
A retrospective, observational chart review of consecutive patients diagnosed with lamellar macular hole and seen by 2 retina specialists (J.P.H., S.D.S.) at the Stein Eye Institute, University of California Los Angeles was carried out. After the approval from the University of California Los Angeles office of human research protection, cases were identified by medical billing record search, using the International Statistical Classification of Diseases and Related Health Problems, Ninth Revision (ICD-9) diagnosis code 362.54 for macular cysts, holes, and pseudoholes.
Exclusion criteria were history of advanced age-related macular degeneration, diabetic retinopathy, myopic choroidal neovascularization, central retinal vein occlusion, uveitis, trauma, and previous pars plana vitrectomy.
In all cases, OCT images were obtained with the Spectralis OCT (Heidelberg Engineering GmbH, Heidelberg, Germany) and reviewed with the Heidelberg Eye Explorer (version 1.8.6.0) using the HRA/Spectralis Viewing Module (version 5.8.3.0). Additionally, some patients were also imaged with the RS-3000 Advance OCT (Nidek Co, Gamagori, Japan).
The presence of lamellar macular hole was defined according to the following OCT findings: presence of irregular foveal contour, separation of the layers of the neurosensory retina, and the absence of full-thickness macular defects.
Spectralis OCT scan patterns were used for all measurements. All eyes had at least 2 images per visit: 20 × 15 degrees, with 19 B-scans spaced 242 μm, and a single high-definition horizontal line at 30 degrees. In addition, some eyes had high-density 15 × 10 degrees, with 97 B-scans spaced 30 μm. Additional imaging patterns for the RS-3000 Advance OCT were the high-definition macula radial (12 lines), the macula map 9 mm × 9 mm, and a single high-definition horizontal line.
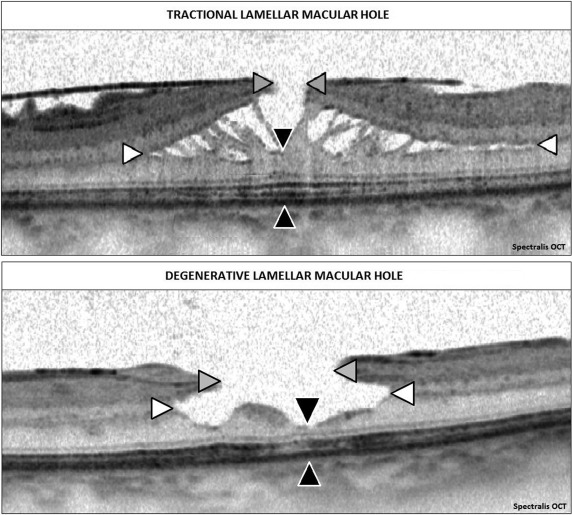
All OCT images were carefully reviewed by at least 2 independent retina specialists (A.G., E.P., H.H.). Analysis and categorization of the morphologic characteristics of lamellar macular hole included shape, minimum foveal retinal thickness, mean central foveal thickness, presence and thickness of the associated epiretinal proliferation, presence of typical epiretinal membrane, integrity of the ellipsoid layer, and the location and morphology of intraretinal separation. We also measured the maximum diameter of the edge of the hole at the level of the retinal surface (inner diameter) and the maximum intraretinal diameter (outer diameter), as seen in Figure 1 (Top and Bottom).
Diameters and minimum foveal retinal thickness measurements were performed with the “caliper” function of the Heidelberg instrument. In all cases, the images were adjusted at 1:1 μm. Mean central foveal thickness as measured was obtained with the automated “thickness map” function of the Heidelberg Eye Explorer.
The best-corrected visual acuity (BCVA) was recorded at each visit and reported in Snellen fraction, which was converted into logarithm of the minimal angle of resolution (logMAR) values for statistical analysis.
In eyes meeting the criteria for lamellar macular hole, lamellar separation of neurosensory retina demonstrated either a “cavitated” or a “schitic” appearance. The schitic appearance was defined by the presence of multiple, narrow hyperreflective tissue bridges crossing wider hyporeflective spaces, located between the outer plexiform and outer nuclear retinal layers ( Figure 2 , Top left). The cavitated appearance was defined by the presence of a homogeneous round-edged hyporeflective space in the neurosensory retina ( Figure 2 , Top right).
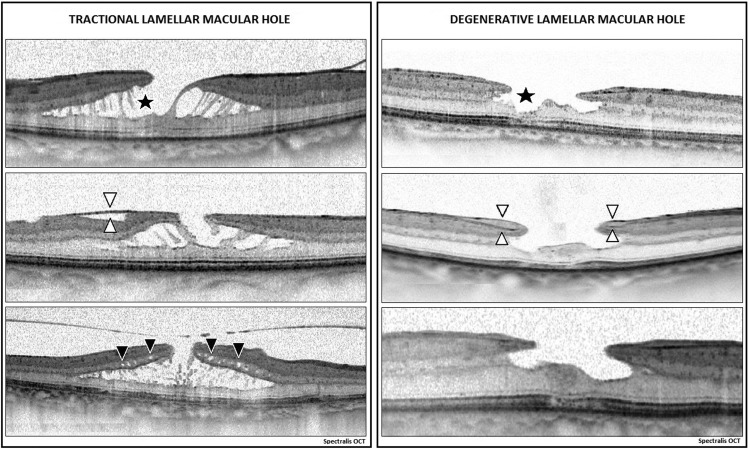
OCT imaging was also used to differentiate lamellar hole–associated epiretinal proliferation from classic or typical epiretinal membrane. The classical epiretinal membrane tissue was diagnosed as a thinner, irregular and hyperreflective line on the inner retinal surface, occasionally accompanied by areas of hyporeflective space between the membrane and the inner retina, while the lamellar macular hole–associated proliferation was defined as thicker preretinal material of homogenous medium reflectivity ( Figure 2 , Middle left and Middle right).
To assess signs of retinal traction, we investigated the presence of retinal folds and wrinkling, retinal thickening, and intraretinal cystic spaces ( Figure 2 , Bottom left and Bottom right).
The progression of lamellar macular hole was assessed both anatomically and functionally. Anatomic progression of lamellar macular hole was defined as widening by more than 50 μm of the inner diameter or of the outer diameter, and/or the appearance of a full-thickness macular hole. We also included the appearance of new defects at the level of the ellipsoid layer in our definition of anatomic progression. Anatomic regression was defined as the reduction of the size of either cavitated or schitic lesions, or the resolution of the lamellar macular hole.
Functional progression was defined as any change in BCVA that may reasonably be related to the progression of the lesion itself, and not to cataract formation or other ophthalmic and medical conditions.
Eyes that underwent surgery were excluded from anatomic and functional progression analysis.
All statistical analysis was conducted using SAS software version 9.3 (SAS Institute, Inc, Cary, North Carolina, USA). Descriptive statistics were first calculated for all variables of interest. Mean and standard deviation values were calculated for continuous variables, while frequency and percentage were calculated for categorical variables. Wilcoxon signed rank test was used to determine the statistically significant change between baseline and the end of follow-up in continuous measurements. Kruskal-Wallis test was used to compare the statistically significant difference in continuous measurements among all subgroups. Fisher exact test was used to compare the difference in categorical variables among all subgroups. A P value of less than .05 was considered statistically significant.
Results
After a comprehensive chart review, 102 eyes from 90 patients, of which 46 (51.12%) were female and 44 (48.88%) were male, met the inclusion criteria and our definition of lamellar macular hole and were enrolled in the study. Mean age was 73.2 ± 10 years and mean follow-up was 33.6 ± 21.7 months. Of the 102 included eyes, 52 (50.98%) were phakic and 50 (49.02%) pseudophakic at baseline.
Analysis of OCT images suggested 2 distinct subtypes of lamellar macular hole defined by specific morphologic features ( Figure 3 , Top and Bottom). The first type ( Figure 3 , Top) was diagnosed in 48 out of 102 eyes (47.06%) and had a “top hat” appearance. Its distinctive characteristics included the presence of a foveal bump, the presence of lamellar hole–associated proliferation, and, in the large majority of the cases, a disrupted ellipsoid zone. Generally, the ratio between inner and outer diameter was more than 1:2 in this group, with a mean value of 0.76 ± 0.38. Furthermore, this subtype was characterized by a round-edged intraretinal cavitation potentially involving outer retinal layers, rather than a “split” between inner and outer retina. We termed this condition “degenerative lamellar macular hole.”
The second type observed ( Figure 3 , Bottom) was diagnosed in 43 out of 102 eyes (42.15%) and had a “moustache” appearance. Its features included the presence of tractional epiretinal membrane. In contrast with degenerative lamellar macular hole, the ratio between inner and outer diameter was generally less than 1:2, with a mean value of 0.31 ± 0.28, and also the ellipsoid layer was intact in almost all cases. Finally, distinct from the degenerative subtype, these lesions were characterized by a sharp-edged schisis-like appearance between outer plexiform and outer nuclear layers, which rarely affected the deeper retinal layers. We termed this subtype “tractional lamellar macular hole.” Criteria for the diagnosis of both degenerative and tractional lamellar macular hole are summarized in Table 1 .
| Diagnostic Criteria a | |||
|---|---|---|---|
| Degenerative n = 48 | Tractional n = 43 | ||
| Inner/outer diameter ratio > 1:2 | n = 44 (91.67%) | Inner/outer diameter ratio < 1:2 | n = 37 (86.05%) |
| Ellipsoid defect | n = 46 (95.83%) | Intact ellipsoid | n = 42 (97.67%) |
| Round-edged cavitation | n = 47 (97.92%) | Sharp-edged split | n = 43 (100%) |
| Foveal bump | n = 42 (87.50%) | Intraretinal cystoid spaces | n = 35 (81.40%) |
| Epiretinal proliferation | n = 46 (95.83%) | Epiretinal membrane | n = 42 (97.67%) |
a Diagnosis is made with a minimum of 3 out of 5 criteria. If the lesion does not match with both categories, it is classified as “mixed.”
Eleven out of 102 eyes (10.78%) with lamellar macular hole shared common features of both tractional and degenerative lamellar macular hole and, as a consequence, were classified as “mixed” lesions. Owing to the small number of eyes included in this group, their characteristics are not described in this section.
Bilateral lamellar macular hole was diagnosed in 12 out of 90 (13.3%) of the included patients. Of those, 4 presented with bilateral tractional lamellar macular hole, while 6 were diagnosed with bilateral degenerative subtype. The remaining 2 patients had a degenerative lamellar macular hole in 1 eye and a mixed lesion in the fellow eye.
Mean follow-up for degenerative and tractional lamellar macular hole were similar: 38.2 ± 21 (range 6.1–77.4) months and 29.6 ± 21.8 (range 3.1–76) months, respectively. While there were no significant sex differences between groups ( P = .12), patients classified with degenerative lamellar macular hole were significantly older (75.8 ± 10 years) compared to those with tractional subtype (69.3 ± 8.9 years), with a P value of .004.
The morphologic differences encountered between groups were reflected in our measurements, and are reported in Table 2 .
| Measurements | Degenerative Group | Tractional Group | ||
|---|---|---|---|---|
| Baseline | Inner diameter | 521.7 ± 197.2 μm | 365.7 ± 214.8 μm | P = .002 |
| End of follow-up | 569.8 ± 203.7 μm | 456.5 ± 244.1 μm | P = .034 | |
| P = .022 | P = .031 | |||
| Baseline | Outer diameter | 789.7 ± 387.3 μm | 1510.3 ± 649.2 μm | P < .0001 |
| End of follow-up | 905.9 ± 356.8 μm | 1746.3 ± 903.7 μm | P < .0001 | |
| P = .001 | P = .001 | |||
| Baseline | Retinal thickness | 101.1 ± 34.0 μm | 140.2 ± 20.3 μm | P < .0001 |
| End of follow-up | 95.2 ± 36.4 μm | 139.0 ± 21.8 μm | P < .0001 | |
| P = .058 | P = .21 | |||
| Baseline | BCVA | 0.27 ± 0.20 logMAR | 0.13 ± 0.12 logMAR | P = .0007 |
| End of follow-up | 0.32 ± 0.26 logMAR | 0.17 ± 0.19 logMAR | P = .006 | |
| P = .42 | P = .52 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


