Purpose
To investigate the surgical outcomes of inverted internal limiting membrane (ILM) insertion in macular hole (MH)-associated retinal detachment (RD) in high myopia.
Design
Retrospective, interventional, consecutive case series.
Methods
This study was conducted at 2 medical centers. Consecutive cases of highly myopic eyes with MH-associated RD were included. Forty eyes were divided into 2 groups: Group 1 (20 eyes) received vitrectomy, ILM peeling within the arcade area, and air-fluid exchange, and Group 2 (20 eyes) received vitrectomy, inverted ILM inserted into the macular hole, and air-fluid exchange. Optical coherence tomography was used to observe the closure of the macular hole. Corrected visual acuity (VA) was also recorded. Two-sample t test and Mann-Whitney U test were used for statistical analysis to compare differences between the 2 groups.
Results
MH was closed in 35% of the eyes in Group 1 and in all eyes in Group 2 ( P < .001). Significant improvement in VA in logarithm of minimal angle of resolution (logMAR) was achieved in both groups. There was no difference in the initial, final, or improvement of logMAR VA in the 2 groups.
Conclusion
Inverted ILM insertion into a macular hole effectively helps close the macular hole in MH-associated RD in high myopia. This may prevent the possible re-detachment from the MH. A prospective study with a larger number of cases and longer follow-up may help validate our findings.
Macular hole (MH) with retinal detachment (RD) in high myopia is a challenging disease for vitreoretinal surgeons. Many surgical approaches to treat MH-associated RD have been proposed, including gas injection, vitrectomy, and posterior hyaloid removal with or without internal limiting membrane (ILM) peeling using gas or silicone oil as internal tamponade. Macular buckling and vitrectomy with scleral imbrications have also been established as treatment options to increase the success rate of surgery. Although anatomic reattachment can be achieved in a high percentage of cases undergoing vitrectomy and ILM peeling, the MH closure rate varies among different investigators in highly myopic eyes complicated by RD. With modern surgical techniques, the success rate of MH closure ranges from around 50% to 70%. Although the success rate has increased, it is still not satisfactory compared with that in MHs without RD. An open hole in an eye with high myopia poses the risk of recurrent RD in addition to contributing to hindered central vision. Recently, Michalewska and associates proposed using an inverted ILM flap as a bridging tissue across an MH for treating large MHs, with MH closure being observed in 98% of cases. However, in cases with MH-associated RD, the ILM flap proposed for a refractory MH may detach from the hole during or after surgery in the presence of a wavy retinal surface and turbulent flow of subretinal fluid, therefore failing to facilitate hole closure. We hypothesized that an inverted ILM flap of a larger size may be trapped securely within the hole and may be less likely to be dislodged from the hole during and after surgery. This procedure may lead to a more effective bridging of the hole to prompt its closure. In this report, we retrospectively reviewed cases of highly myopic eyes with MH and RD treated with an inverted ILM flap inserted into the hole. We described the technique we used in detail, and, in comparison to standard vitrectomy with ILM peeling, we sought to demonstrate the advantages of this procedure.
Methods
This study was conducted at 2 centers (Changhua Christian Hospital and National Taiwan University Hospital) and included consecutive case series with surgical interventions. From January 2013 to February 2015, 40 cases of high myopia complicated by MH with RD treated with vitrectomy were retrospectively enrolled. Eyes were divided into 2 groups: Group 1 received vitrectomy, ILM peeling within the arcade area, and air-fluid exchange, and Group 2 received vitrectomy, inverted ILM inserted into the macular hole, and air-fluid exchange. Most of the cases with ILM flap insertion underwent surgery after January 2014, and most of the cases with ILM peeling without ILM flap insertion underwent surgery from January 2013 to January 2014. Patients were informed of the risks of retinal toxicity from indocyanine green (ICG) dye and the possibility of an open MH postoperatively. The study was approved by the Institutional Review Boards of Changhua Christian Hospital (CCHIRB: 150809) and National Taiwan University Hospital (NTUH IRB: 201506065RINA). The study procedures adhered to the tenets of the Declaration of Helsinki and conformed to the HIPAA regulations. All of the surgical procedures were performed by 2 experienced surgeons (S.N. Chen and C.M. Yang, from Changhua Christian Hospital and National Taiwan University Hospital, respectively), and all of the patients provided written informed consent.
High myopia was defined as an eye with a refractive error of more than 6 diopters or an axial length of more than 26 mm. All cases were followed up for more than 6 months after surgery. Staphyloma was defined as ectasia in the posterior pole detected in optical coherence tomography (OCT) and fundus photography. Patients with concurrent peripheral breaks, proliferative vitreoretinopathy changes, or trauma were excluded. The severity of RD was classified into 2 types: within the equator (type 1) or beyond the equator (type 2). Each patient underwent a thorough ophthalmologic examination. Data including best-corrected visual acuity (BCVA), refraction status (Auto Refractometer KR-8800; Topcon Corporation, Tokyo, Japan), axial length measured by ultrasound (PAC Scan 300AP; Sonomed Inc, Lake Success, New York, USA), indirect ophthalmoscopy findings, and OCT examinations (Cirrus HD-OCT 400; Carl Zeiss Meditec, Dublin, California, USA; RTVue OCT RT100; Optovue, Fremont, California, USA; Stratus OCT 3000; Carl Zeiss Meditec) were recorded in all patients. Axial length measurements were conducted while the retina was attached. OCT studies were conducted every 3–6 months. OCT features were obtained by multiple scans centered on the fovea. The scan length was 6–10 mm depending on the machine used. The eyes were divided into 2 groups: Group 1 (20 eyes) received vitrectomy, ILM peeling within the arcade, and air-fluid exchange, and Group 2 (20 eyes) received vitrectomy, ILM insertion into the MH, and air-fluid exchange.
Surgical Techniques
Group 1
Standard 3-port 23 gauge pars plana vitrectomy was performed. After core vitrectomy and triamcinolone acetonide–assisted (TA, 2.5 mg/mL) posterior hyaloid removal, the posterior retina was carefully inspected to identify preretinal membrane. Forceps removal of the membrane (if present) was performed. An ICG solution (25 mg ICG in 15 mL 5% glucose-water solution, final concentration = 1.7 mg/mL) was then carefully applied around the macular hole within the arcade. Excessive ICG was immediately removed by suction. The ILM within the arcade was completely removed, and the subretinal fluid was drained from a separate iatrogenic break outside the staphyloma margin if the detachment extended to or beyond the equator. Air-fluid exchange was performed as completely as possible without disturbing the preexisting macular hole.
Group 2
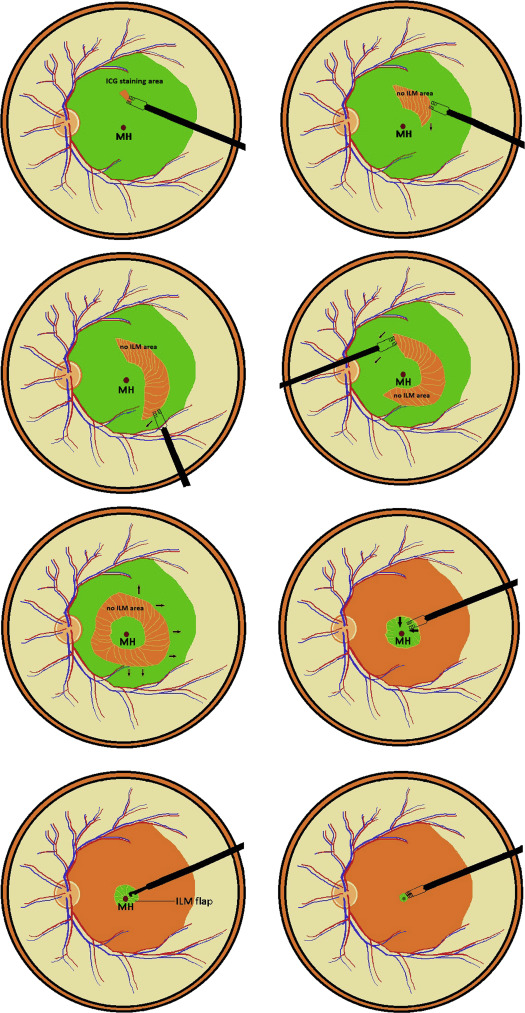
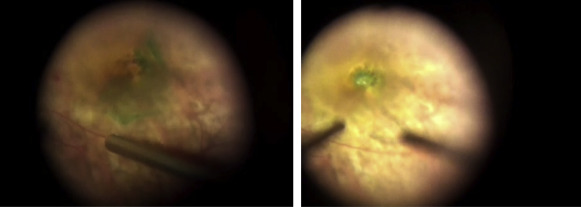
The initial surgical procedures were similar to those of Group 1; however, after ICG staining, direct forceps grasping of the superficial retina in an ICG-stained area was then performed to create an ILM break at the parafoveal area about 1.5 disc diameters away from the MH. Further ILM peeling was directed in a circular manner at the parafoveal area. Care was taken not to peel the ILM flap across the hole edge. When a piece of ILM tissue was removed, continuous ILM peeling was initiated by forceps grasping of the outer ILM tear margin, and was directed away from the center. The process was repeated in a circular fashion, leaving a ring-shaped ILM island measured about 1.5–3 disc diameters centered on the MH. The ILM outside the parafoveal area was peeled to the arcade along with the overlying epiretinal membrane (ERM). The ILM around the hole, along with the overlying ERM (if present), was then detached from the retina up to the edge of the hole. Excessive ILM was carefully trimmed with a vitreous cutter with low suction (around 50 mm Hg) in a shaving mode. The peripheral retina was then examined for possible breaks. The ILM flap anchored on the edge of the hole was inverted and inserted into the hole using microforceps with the tips closed. All free-floating ends of the ILM tissue were carefully placed under the hole. Fluid-air exchange up to the staphyloma margin or slightly above the upper margin of the detached retina was performed if the retinal detachment was localized within the arcade. Drainage retinotomy was performed with a vitreous cutter at the temporal upper detached retina outside the staphyloma for internal drainage and fluid-air exchange if the detachment extended to or beyond the equator. No complete fluid-air exchange was intended, and the air was allowed to reach the margin of the staphyloma. Laser photocoagulation was performed around the iatrogenic break. Lastly, the air was replaced by 20% C3F8 infusion into the vitreous cavity. The patients were subsequently kept in a facedown position overnight and were allowed to position themselves in any manner other than the supine position for approximately 1 week. Schematic drawings of the procedures are shown in Figure 1 ; still photographs taken during surgery are shown in Figure 2 .
Statistics
Two-sample t tests were used to calculate differences in age, axial length, duration of symptoms, follow-up duration, pre- and postoperative logMAR visual acuity (VA), and improvement in logMAR VA between the 2 groups. The Mann-Whitney U test was used to calculate differences between sex, lens statuses, extent of RD, and the MH closure rate.
Results
The study examined 40 eyes in 40 patients (10 male and 30 female), with 20 eyes in Group 1 and 20 in Group 2. The mean age was 61.25 ± 8.75 years, and the mean axial length was 28.87 ± 1.94 mm. Three eyes in Group 2 had failed previous surgery of vitrectomy, posterior hyaloid membrane peeling, air-fluid exchange, and silicone oil tamponade with RD confined to the posterior pole. The other eyes had received vitrectomy, ILM peeling or ILM insertion, and air-fluid exchange as their first surgery. There was no significant difference between the 2 groups in age, sex, duration of symptoms, axial length, lens status, extent of retinal detachment, or initial logMAR VA. The follow-up period was 14.13 ± 6.66 months in Group 1 and 8.92 ± 3.23 months in Group 2 ( P = .014), with significant difference between the 2 groups ( Table 1 ).
| Total (N = 40) Mean ± SD | Group 1 (N = 20) Mean ± SD | Group 2 (N = 20) Mean ± SD | P Value | |
|---|---|---|---|---|
| Age (y) | 61.25 ± 8.75 | 60.53 ± 8.78 | 62.06 ± 8.90 | .607 a |
| Sex (m/f) | 10/30 | 6/14 | 4/16 | .451 b |
| Lens status (Ph/PP) | 21/19 | 10/10 | 11/9 | 1.000 b |
| Mean duration of symptoms (d) | 353.7 ± 719.86 | 161.60 ± 136.25 | 587.0 ± 1032.53 | .424 a |
| Extent of RRD (type 1/type 2 c ) | 21/19 | 10/10 | 11/9 | .749 b |
| AXL (mm) | 28.87 ± 1.94 | 29.35 ± 1.88 | 28.40 ± 1.94 | .158 a |
| Duration of F/U (m) | 11.81 ± 5.94 | 14.13 ± 6.66 | 8.92 ± 3.23 | .014 a |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


