Purpose
To study the efficacy of a single intravitreal injection of expansile gas in releasing vitreomacular traction.
Design
Retrospective, interventional case series.
Methods
Fifteen eyes of 14 consecutive patients with symptomatic and persistent vitreomacular traction (>3 months’ duration) on spectral-domain optical coherence tomography (SD OCT) received a single intravitreal injection of 0.3 mL 100% perfluoropropane (C 3 F 8 ) as an alternative to pars plana vitrectomy (PPV). Primary outcome was the number of eyes with complete vitreomacular traction release on OCT 1 month following treatment. Secondary outcomes included changes in visual acuity (VA), foveal contour, central foveal thickness, and maximal foveal thickness 1 month following treatment, and final VA.
Results
Mean age (± SD) was 72.1 ± 12.6 years. Mean follow-up was 398.7 ± 174.4 days. Vitreomacular traction was idiopathic in 7 eyes and associated with diabetes in 6. One month following treatment, vitreomacular traction was released in 6 eyes (40%). Three further eyes (20%) had resolution of vitreomacular traction within 6 months, 4 (27%) underwent PPV, and 2 (13%) subsequently declined surgery. Foveal contour was restored in 7 eyes (47%). VA and central foveal thickness were similar 1 month following treatment, but maximal foveal thickness decreased by 65.8 μm ( P = .041). Mean final VA decreased 0.03 logMAR units from baseline ( P = .536). Eyes with vitreomacular traction release within 1 month had less extensive vitreomacular traction ( P = .037), low vitreous face reflectivity, and maximal foveal thickness <500 μm ( P = .004) pretreatment. There were no associated adverse events.
Conclusions
Intravitreal C 3 F 8 injection could offer a minimally invasive alternative to PPV in patients with symptomatic and persistent vitreomacular traction. It appears particularly effective in eyes with less extensive vitreomacular traction and low vitreous face reflectivity on SD OCT. Further studies are warranted.
Strong vitreoretinal adhesions are normally present at the peripheral retina, the optic nerve head, and the fovea. Usually these adhesions cause no discernible problem, but it is well recognized that abnormal vitreoretinal adhesion can cause disease. This most commonly occurs in the context of posterior vitreous detachment (PVD), where persisting vitreomacular adhesion leads to tractional macular damage. Vitreomacular traction can occur in isolation, in which case it is termed idiopathic vitreomacular traction syndrome. Optical coherence tomography (OCT), and more recently spectral-domain OCT (SD OCT), have greatly improved visualization of the vitreomacular interface. As a result, there is growing recognition that vitreomacular adhesion and vitreomacular traction may play a role in a range of diseases, such as cystoid macular edema (CME), vitreoschisis, macular pucker, macular holes, age-related macular degeneration (AMD), and diabetic macular edema (DME).
The true natural course of vitreomacular traction remains undetermined; however, spontaneous release of vitreomacular traction is generally believed to occur infrequently. Hikichi and associates found that only 11% of eyes developed complete PVD over a 5-year period, with 64% experiencing a 2-line reduction in Snellen visual acuity (VA). Pars plana vitrectomy (PPV) remains the treatment of choice for many symptomatic cases, with a success rates up to 75%. Since PPV carries risks, a minimally invasive alternative could be advantageous in terms of not only safety, but also cost, convenience, comfort, and global accessibility. One potential treatment is pharmacologic vitreolysis, in which an agent such as ocriplasmin acts on the vitreous and vitreomacular adhesion to induce a PVD and release vitreomacular traction. Although these treatments are thought to produce a chemical weakening of the vitreomacular interface, they do not induce a tractional force to exploit this weakening.
In 1995 Chan and associates first published the clinical use of an intravitreal gas bubble to treat macular holes. The presumed mechanism of action was mechanical induction of PVD. In their series, 10 of 11 impending holes responded to treatment; 3 of 6 stage 2 holes closed, but 2 stage 3 holes both failed to close. Jorge and associates reported that an intravitreal gas injection led to closure of stage II macular holes in 5 of 6 eyes. Mori and associates published a series using intravitreal gas for macular holes, producing anatomic closure in 50% (10 eyes) and detachment of the posterior vitreous at the macula in 95% of cases, both on clinical examination and using time-domain OCT. We are aware of only a single case report that demonstrated the successful treatment of an impending macular hole with an intravitreal gas bubble using SD OCT.
In 2000, Ochoa-Contreras and associates reported that they successfully induced a PVD in all 12 eyes of diabetic patients treated with an intravitreal gas bubble, as confirmed by B-scan ultrasound. These patients did not have vitreomacular traction, but interestingly the contralateral eye was used as a control and none developed a PVD during the 2-year follow-up period. More recently, McHugh and associates published a series of 5 patients with clinically significant macular edema refractory to laser therapy. None had vitreomacular traction. All patients had successful induction of a PVD within 1 month of an intravitreal gas injection.
The present preliminary study aimed to determine if intravitreal gas injection is an effective treatment for vitreomacular traction in the context of a wider range of ocular diseases. It also aimed to employ SD OCT to validate the earlier observations that used time-domain OCT. We report a consecutive case series of 15 eyes that were treated with an intravitreal gas injection to release vitreomacular traction, including the first cases of idiopathic vitreomacular traction syndrome, vitreomacular traction associated with DME and neovascular AMD. The central hypothesis was that an intravitreal gas injection may induce a PVD and subsequently release vitreomacular traction in a range of diseases. If this hypothesis is correct, then pneumatic release of vitreomacular traction may, subject to further studies, offer a minimally invasive, easily accessible treatment for a range of patients who might otherwise require PPV.
Methods
This study reports a retrospective consecutive series of patients who elected to undergo an intravitreal gas injection for the treatment of vitreomacular traction, between September 2009 and May 2011, in a tertiary retinal unit in a large London teaching hospital. All patients underwent assessment of Snellen VA, tonometry, anterior and posterior segment biomicroscopy, and SD OCT (Spectralis HRA+OCT, Heidelberg Engineering, Heidelberg, Germany; or Cirrus, Carl Zeiss Meditec, Dublin, California, USA). In accordance with National Health Service Health Research Guidance, ethics review was not required to retrospectively report this case series. This study and data accumulation were in conformity with all country, federal, or state laws, informed consent was obtained, and the study was in adherence to the tenets of the Declaration of Helsinki.
All patients were symptomatic, with long-standing metamorphopsia, micropsia, or reduced VA. The diagnosis of vitreomacular traction was based on clinical examination and SD OCT. Vitreomacular traction was defined as SD OCT-visible vitreous attachment within a 1500-μm radius of the foveal center causing anteroposterior vitreofoveal traction, with associated microstructural retinal changes. All cases had vitreomacular traction greater than a published photographic standard.
All patients were observed for 2 months prior to treatment to look for spontaneous resolution of vitreomacular traction. All patients were subsequently deemed suitable for pars plana vitrectomy. Following this, they were offered continued observation, intravitreal injection of expansile gas, or standard 23-gauge pars plana vitrectomy. Patients with any preexisting peripheral retinal pathology predisposing the eye to retinal detachment were not offered this treatment.
Surgical Procedure
All intravitreal injections of expansile gas were performed in an operating room as a day case procedure, and in accordance with the Royal College of Ophthalmologists’ guidelines for intravitreal injections, although it would have been possible to undertake the procedure in a clinic setting. Using topical anesthetic, povidone-iodine, drape, eyelid speculum, and a 27-gauge needle with a 1-mL syringe, 0.3 mL of 100% perfluoropropane (C 3 F 8 ) gas (Arceole; Arcad Ophtha, Toulouse, France) was injected intravitreally through the pars plana, within the product’s licensed indication of use for endotamponade of the retina. An anterior chamber paracentesis was undertaken if necessary.
Patients were prescribed broad-spectrum antibiotic eye drops 4 times daily for 4 days. No posturing was required. The intraocular pressure was assessed the following day. Unless otherwise indicated, patients were reviewed for a full eye examination and SD OCT scan 1 month following treatment, and as clinically indicated thereafter.
Outcome Measures
The primary outcome measure was vitreomacular traction release confirmed using SD OCT 1 month following gas injection. Secondary outcome measures were changes in VA, foveal contour, central foveal thickness, and maximum foveal thickness 1 month following injection, and vitreomacular traction release within 6 months. The primary outcome was reported at 1 month, as longer outcomes may be influenced by the clinical course of associated eye disease, such as DME; however, VA was also reported at final follow-up.
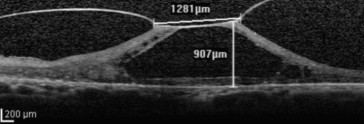
Maximal horizontal diameter of the attached vitreous face at the macula was also measured. Posterior vitreous face reflectivity was independently categorized by 2 retinal physicians as low, moderate, or high. As a reference for moderate reflectivity, we used a SD OCT image ( Figure 1 ). The observer was masked to the outcomes when making observations. Adverse events were recorded.
Ophthalmologic Examination
SD OCT scans were acquired by a trained photographer through a dilated pupil. The standard scanning protocol for the Spectralis SD OCT consisted of a Macular Volume Scan with 1024 A-scans/B-scan and 37 B-scans, and was obtained over an area of 6 × 6 mm, averaging 9 scans for each B-scan. For the Cirrus SD OCT, a Macular Cube Scan (512 A-scans × 128 B-scans) was used covering an area of 6 × 6 mm centered on the fovea.
Central foveal thickness was measured from the ETDRS subfield 9 (the central 1-mm foveal subfield) using the built-in retinal mapping software, with manual adjustment if segmentation errors were detected. The built-in software calipers were used to manually measure the maximum foveal thickness (within the central area of 1 mm in diameter, corresponding to the central fovea) between the inner and outer retinal boundaries, and the extent of maximal horizontal vitreomacular adhesion ( Figure 1 ).
Statistical Analysis
A paired or unpaired t test or χ 2 test was used to evaluate changes before and after treatment and to compare treatment outcomes with baseline characteristics. The significance level was set to P < .05. All statistical analyses were carried out using STATA statistics/data analysis software (Stata Statistical Software: Release 6, 2000; StataCorp, College Station, Texas, USA).
For statistical purposes, VA was analyzed by means of the logarithm of the minimal angle of resolution (logMAR) score, developed by Ferris and associates. The logMAR score was derived by taking the logarithm (base 10) of the Snellen fraction [logMAR = log (1/decimal acuity)]. A score of 0.0 in logMAR units is equivalent to a Snellen VA of 20/20, and 1.0 is equivalent to 20/200. Counting fingers and hand-motion VA were assigned Snellen equivalents of 0.01 (+2.0 logMAR) and 0.001 (+3.0 logMAR), respectively.
Results
Patient Demographics
Fifteen eyes of 14 patients with persistent and symptomatic vitreomacular traction were treated. Eight patients were male. Nine were white, 3 were Afro-Caribbean, and 2 were Asian. Mean age (± SD) at presentation was 72.1 ± 12.6 years (range: 36-89). Vitreomacular traction was documented on SD OCT for a mean of 328.1 ± 250.9 days prior to treatment (range: 70-860). Mean follow-up after treatment was 353.75 ± 159.62 days (range: 91-658). In 7 eyes vitreomacular traction was labeled as idiopathic vitreomacular traction syndrome, whereas vitreomacular traction was associated with diabetic macular edema in 6 eyes and 1 case each of impending macular hole and exudative AMD. Baseline and posttreatment demographics and characteristics are summarized in Table 1 .
| Case | Age | Sex | Race | Diagnosis | Before Treatment | After Treatment | FC | PPV | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VA | CFT | MFT | HVMA | VFR | VA | CFT | MFT | ||||||||
| 1 | 89.5 | M | W | DME | 1.00 | 714 | 1115 | 1270 | Mod | 2.00 | 882 | 907 | IRF | Y | Fail |
| 2 | 71.8 | M | A | VMTS | 0.20 | 298 | 440 | 134 | Low | 0.60 | 365 | 513 | Norm | N | QS |
| 3 | 36.5 | F | W | DME | 0.50 | 555 | 652 | 513 | Mod | 0.60 | 535 | 613 | IRF | Y | Fail |
| 4 | 77.3 | M | W | wAMD | 0.14 | 466 | 492 | 135 | Low | 0.12 | 272 | 229 | Norm | N | AS |
| 5 | 70.4 | F | AC | DME | 0.30 | 287 | 432 | 783 | Low | 0.30 | 366 | 393 | IRF | N | Fail |
| 6 | 67.1 | F | AC | DME | 0.30 | 340 | 431 | 668 | Low | 0.60 | 180 | 152 | Norm | N | AS |
| 7 | 77.0 | F | W | VMTS | 0.50 | 259 | 288 | 640 | Low | 0.50 | 243 | 311 | Norm | N | QS |
| 8 | 89.1 | M | W | VMTS | 0.80 | 509 | 558 | 641 | High | 0.80 | 528 | 564 | IRF | Y | Fail |
| 9 | 60.9 | M | W | VMTS | 0.50 | 254 | 335 | 177 | Low | 0.30 | 214 | 178 | Norm | N | AS |
| 10 | 72.4 | M | A | DME | 1.00 | 632 | 749 | 531 | Mod | 0.80 | 604 | 735 | IRF | Y | Fail |
| 11 | 73.6 | F | W | IMH | 0.80 | 316 | 350 | 458 | Low | 1.00 | 329 | 382 | FTMH | Y | AS |
| 12 | 80.9 | F | W | VMTS | 0.30 | 264 | 362 | 240 | Low | 0.20 | 270 | 230 | Norm | N | AS |
| 13 | 77.2 | F | W | VMTS | 0.30 | 295 | 351 | 609 | Low | 0.50 | 354 | 391 | Norm | N | QS |
| 14 | 73.5 | M | AC | VMTS | 0.60 | 383 | 406 | 1145 | Low | 0.80 | 368 | 385 | IRF | N | Fail |
| 15 | 64.8 | M | W | DME | 0.60 | 343 | 406 | 327 | Low | 0.50 | 360 | 396 | IRF | N | AS |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


