Purpose
To estimate the prevalence of untoward events during cataract surgery with the use of pupillary expansion devices and intraoperative floppy iris (IFIS).
Design
Retrospective analysis of 4923 cataract surgery cases from the Veterans Affairs Ophthalmic Surgical Outcomes Data Project.
Methods
Outcomes from 5 Veterans Affairs medical centers were analyzed, including use of alpha-blockers (both selective and nonselective), IFIS, intraoperative iris trauma, intraoperative iris prolapse, posterior capsular tear, anterior capsule tear, intraoperative vitreous prolapse, and use of pupillary expansion devices. P values were calculated using the χ 2 test.
Results
A total of 1254 patients (25.5%) took alpha-blockers preoperatively (selective, 587; nonselective, 627; both, 40). Of these 1254 patients, 428 patients (34.1%) had documented IFIS. However, 75.2% of patients with IFIS (428/569) had taken alpha-blockers preoperatively ( P < .00001). A total of 430 patients (8.7%) had a pupillary expansion device used during their cataract surgery, of which 186 patients (43.4%) had IFIS ( P < .0001). Eighty-six patients with IFIS had at least 1 intraoperative complication and 39 patients with IFIS had more than 1 intraoperative complication ( P < .001).
Conclusions
The use of either selective or nonselective alpha-antagonists preoperatively demonstrated a significant risk of IFIS. Nonselective alpha-antagonists caused IFIS at a higher prevalence than previously reported. This study did demonstrate statistically significant increased odds of surgical complications in patients with IFIS vs those without IFIS in all groups (those taking selective and nonselective alpha-antagonists and also those not taking medications).
Selective and nonselective alpha-blockers for the treatment of benign prostatic hypertrophy are used frequently in the Veterans Health Administration system and known to be associated with intraoperative floppy iris syndrome (IFIS). IFIS appears in various severities during cataract surgery and not all at-risk patients will show all or any features of IFIS. It is most correlated with selective alpha1-antagonists while nonselective alpha-antagonists show minimal, if any, effects, according to current literature. In a multicenter evaluation, Chang and associates found that 90% of IFIS was noted in 167 eyes of 136 patients taking tamsulosin. The IFIS was rated as mild in 17%, moderate in 30%, and severe in 43% of study eyes. Takmaz and associates determined that the incidence of IFIS in 858 eyes of 774 patients who had phacoemulsification surgery and were taking tamsulosin between August 2005 and November 2006 was 77.8%, and 0.16% of patients exhibited iris prolapse. Chadha and associates found that 57% of patients taking tamsulosin showed features of IFIS and diabetes was not a feature of the IFIS. Various methods have been used to overcome the small pupil and floppy iris that may occur during cataract surgery with various alpha-blockers. These would include Healon 5, iris retractors, pupil expansion rings, and topical atropine. This study reports on the prevalence of untoward events during cataract surgery in patients with intraoperative floppy iris and/or the use of pupillary expansion devices in a multicenter, retrospective analysis.
Methods
For this multicenter, retrospective analysis, internal review board (IRB) approval was obtained at all 5 Veterans Health Administration pilot sites. The data were collected and analyzed in a HIPAA-compliant fashion. Informed consent was waived by the IRB because it would be impossible to obtain consent from patients in a masked database since this was a retrospective analysis of a previously collected dataset used for internal quality assurance in the Veterans Health Administration. The initial dataset was collected as outlined below.
Ophthalmic Surgery Outcomes Database Project
A pilot project was developed to begin data collection and make recommendations regarding ophthalmic surgical procedures in the Veterans Health Administration. Only cataract surgeries were included because these represented approximately 85% of all ophthalmic surgical procedures in the Veterans Health Administration system. Five Veterans Health Administration pilot sites were selected to participate. The pilot sites had to meet the following criteria: (1) perform a minimum of 500 ophthalmic surgical cases per year; (2) have an identifiable Clinical Champion for the project; and (3) have the ability to identify and employ a nurse reviewer for the project. Registered nurse reviewers were selected to collect preoperative, intraoperative, and postoperative data from the Veterans Affairs electronic medical record and also collect preoperative (within 30-90 days of surgical procedure) and postoperative (30-90 days post procedure) National Eye Institute Visual Function Questionnaire (NEI-VFQ) forms from patients who were undergoing cataract surgery.
Development of a data collection tool known as the Risk Assessment Form (RAF) was initiated by Clinical Champion physicians at the participating pilot sites. It was decided to include data from all phases of the surgical experience. In all, approximately 150 data elements were chosen for inclusion in the original RAF. These data elements were defined by using Veterans Affairs Surgical Quality Improvement Project definitions when possible and establishing new definitions as needed when prior definitions were not available. Use of the RAF enabled the 5 pilot sites to standardize electronic templates that include preoperative assessment, intraoperative reporting, and postoperative follow-up to provide a viable framework for data gathering. Surgeons entered all relevant surgical elements in an operative note template immediately following each surgical case.
A centralized Microsoft Access database was developed and nurse reviewers began administering preoperative and postoperative NEI-VFQs and manually entering collected preoperative and postoperative clinical data on each patient, as well as the surgeons’ operative notes, and transferring these data in masked form to the database in July 2009. Data from each of the pilot sites were validated and compiled for statistical purposes.
Records for eligible patients were abstracted by the nurse reviewers and entered into individual Microsoft Access databases via a graphical user interface. The Ophthalmic Surgery Outcomes Database Project employed a statistician to help with the data management portion of the project. After records accumulated for a period of time, the Access databases were provided to the statistician for data validation and statistical analysis. The statistician first merged the individual Access databases into a central staging Microsoft SQL Server database, and then ran data validation and cleaning code using the R statistical software package. Next, the statistician discussed validation issues with the nurse reviewers and necessary corrections to the database were made. Finally, clean records were stored in a Microsoft SQL Server database for statistical analysis.
Pertaining to this retrospective analysis, the following data elements were analyzed: alpha-blockers (both selective and nonselective), IFIS, intraoperative iris trauma, intraoperative iris prolapse, posterior capsular tear, anterior capsule tear, intraoperative vitreous prolapse, and use of pupillary expansion devices. The primary endpoint of this study was to determine the prevalence of IFIS and association with the use of alpha-antagonists. Secondary endpoints included analysis of the use of pupillary expansion devices and occurrence of complications in patients experiencing IFIS and taking alpha-antagonists. The decision of determining IFIS was left to the individual surgeon, although flaccid iris that surges with normal intraoperative fluidics and progressive pupil constriction were used in the determination. All cases of IFIS were documented by the surgeon immediately after the surgical case. Iris prolapse was listed as a separate variable that was documented. Determination of use of a selective or nonselective alpha-antagonist was done by analyzing the Veterans Affairs electronic medical record, looking for selective alpha1a-antagonists (tamsulosin and alfuzosin) and nonselective alpha1-antagonists (doxazosin, prazosin, terazosin), in which the patient was currently taking the drug or had taken it in the past year. This was a dichotomous variable (ie, yes or no) and did not differentiate between medications within a specific class.
Data Analysis
Data were analyzed using Microsoft Excel 2010 (Version 14.0; Microsoft Corporation, Redmond, Washington, USA), EpiInfo (Version 7.1.0.6, 2012; Centers for Disease Control and Prevention, Atlanta, Georgia, USA), and JMP Pro software (Version 10.0, SAS Institute, Cary, North Carolina, USA). Statistical evaluation included χ 2 testing, Fisher exact test, and Mantel-Haenszel method or nominal logistic regression to estimate odds ratios (OR) with 95% confidence intervals (CI). P values <.05 were considered statistically significant.
Results
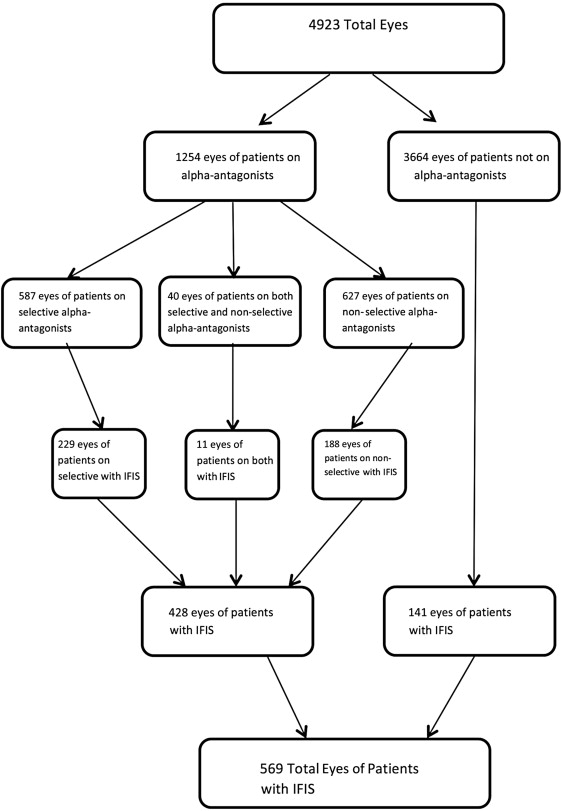
From April 1, 2009 to February 15, 2012, 4923 eyes of 3809 patients were included in the Ophthalmic Surgery Outcomes Database pilot project. A total of 1254 patients (25.5%, 1254/4923) took alpha-antagonists preoperatively. Of these patients, 587 patients (46.8%, 587/1254) took selective alpha-antagonists, 627 patients (50.0%, 627/1254) took nonselective alpha-antagonists, and 40 patients (3.2%, 40/1254) took both ( Figure ). A total of 569 patients (11.5%, 569/4923) had documented cases of IFIS. Of these patients, 428 patients (75.2%, 428/569) were on alpha-antagonists preoperatively and the rest were not ( P < .0001). A total of 229 patients (53.5%, 229/569) took selective alpha-antagonists and 188 patients (43.9%, 188/569) nonselective alpha-antagonists, while 11 patients (2.6%, 11/569) took both.
A total of 430 patients (8.7%, 430/4923) had a pupillary expansion device used during their cataract surgery, of which 186 patients had IFIS (43.4%, 186/430) ( P < .0001). We found that the odds of using of pupillary expansion devices were significantly higher in patients with IFIS vs those without IFIS (OR = 6.4, CI: 3.8, 11.4; P < .0001) after adjusting for alpha-antagonist intake (selective, nonselective, both, or none). Of the 186 patients with IFIS and the use of a pupillary expansion device, 95 patients (51.1%, 95/186) took selective alpha-antagonists, 38 patients (20.4%, 38/186) took nonselective alpha-antagonists, 3 patients took both (1.6%, 3/186), and 50 patients (26.9%, 50/186) were not taking any alpha-antagonists ( P < .001).
The intraoperative complications evaluated for patients exhibiting IFIS included anterior capsule tears, posterior capsule tears, vitreous prolapse, iris trauma, and iris prolapse ( Table 1 ). One hundred twenty-five patients with IFIS (21.97%, 125/569) had at least 1 intraoperative complication; of these, 86 (68.8%, 86/125) had 1 complication and 39 (31.2%, 39/125) had more than 1 intraoperative complication ( P < .0001). There were significant differences in the odds of having 1 complication in patients with IFIS vs no IFIS (OR: 3.94, CI: 2.9, 5.2; P < .001), as well as in the odds of having 2 or more complications (OR: 2.64, CI: 1.8, 3.8; P < .001). These differences were still significant after adjusting for the use of expansion devices in both groups (OR: 3.05, CI: 2.25, 4.1; P < .0001 and OR: 2.16, CI: 1.43, 3.2; P < .001, respectively). Of these 39 patients with IFIS and more than 1 intraoperative complication, 46.2% (18/39) had pupillary expansion devices used, compared to 9.9% (13/132) of those without IFIS and more than 1 intraoperative complication ( P < .0001). Only 1 patient had had all 5 complications listed above.
| Complication | IFIS (N = 569) | Non-IFIS (N = 4355) | Total (N = 4923) | Odds Ratio (95% CI) | P Value |
|---|---|---|---|---|---|
| Anterior capsule tear | 22 (3.9%) | 136 (3.1%) | 158 (3.2%) | 1.24 (0.78, 1.97) | .375 |
| Posterior capsule tear | 39 (6.9%) | 160 (3.7%) | 199 (4.05%) | 1.92 (1.34, 2.76) | <.001 |
| Iris prolapse | 68 (11.9%) | 41 (0.9%) | 109 (2.22%) | 14.23 (9.5, 21.2) | <.0001 |
| Iris trauma | 22 (3.9%) | 29 (0.7%) | 51 (1.1%) | 5.98 (3.4, 10.5) | <.0001 |
| Vitreous prolapse | 24 (4.2%) | 128 (2.9%) | 152 (3.1%) | 1.45 (0.9, 2.27) | .12 |
| No complications | 444 (78.0%) | 4012 (92.4%) | 4456 (90.7%) | <.0001 (Pearson χ 2 ), trend test <.001 | |
| One complication | 86 (15.1%) | 197 (4.5%) | 283 (5.8%) | 3.94 (2.9, 5.2) | <.001 |
| Any 2 complications | 31 (5.5%) | 106 (2.4%) | 137 (2.8%) | 2.64 (1.8, 3.8) | <.001 |
| Any 3 complications | 6 (1.1%) | 23 (0.5%) | 29 (0.6%) | 2.64 (1.8, 3.8) | <.001 |
| Any 4 complications | 1 (0.2%) | 4 (0.1%) | 5 (0.1%) | 2.64 (1.8, 3.8) | <.001 |
| Any 5 complications | 1 (0.2%) | 0 (0.0%) | 1 (0.02%) | 2.64 (1.8, 3.8) | <.001 |
| Total | 125 (21.97%) | 330 (7.6%) | 455 (9.2%) | 3.42 (2.7, 4.3) | <.001 |
We found a significant difference in the proportion of IFIS in those taking alpha-antagonists of any type vs those not taking alpha-antagonists ( Table 2 ). In those taking alpha-antagonists, we observed significantly higher ORs of iris prolapse and iris trauma when comparing patients with IFIS vs those with no documented IFIS (OR: 15.9, CI: 6.2, 40.9 and OR: 8.6, CI: 2.4, 30.3, respectively). These results must be cautiously interpreted, given the wide confidence intervals. After adjusting for the use of pupillary expansion devices, there were more complications in those with IFIS vs with no IFIS regardless of the alpha-antagonist intake.



