Purpose
To determine the intra- and inter-visit reproducibility of ganglion cell–inner plexiform layer thickness measures using handheld optical coherence tomography (OCT) in sedated children with optic pathway gliomas and/or neurofibromatosis type 1 (NF1).
Design
Prospective longitudinal cohort study.
Methods
Children with sporadic optic pathway gliomas and/or NF1 who had ≥2 volumes acquired over the macula using handheld OCT during sedation for clinically indicated magnetic resonance imaging were eligible for the intra-visit cohort. Children with repeat handheld OCT imaging within 6 months were eligible for the inter-visit cohort. Total retinal thickness and ganglion cell–inner plexiform layer thickness were measured using custom-designed automated segmentation software. Reproducibility was compared across average and anatomic quadrant by calculating the coefficient of variation (CV) and intraclass correlation coefficient (ICC).
Results
Forty-two subjects (median age 5.4 years, range 0.8–12.7 years) contributed 45 eyes to the intra-visit cohort. Thirty-one subject eyes had normal vision and 14 had abnormal vision (decreased visual acuity and/or visual field). Average and quadrant ganglion cell–inner plexiform layer measures demonstrated CVs ≤4.5% with excellent ICCs (>0.935). The superior quadrant CV differed between subjects with (4.4%) and without (2.1%) vision loss ( P < .05). Twenty-five subject eyes were eligible for the inter-visit cohort, demonstrating CVs from 1.6% to 5.2%. Inter-visit ICCs were excellent (0.955–0.995).
Discussion
Handheld OCT imaging in sedated children with optic pathway gliomas produces highly reproducible measures of ganglion cell–inner plexiform layer thickness.
Optic pathway gliomas, a relatively common tumor of the anterior visual pathway in children, require surveillance and treatment most frequently between 1 and 6 years of age. Since change in tumor size is not well correlated with visual outcomes, a decline in visual acuity (VA) and or visual field (VF) are the primary indications to initiate or alter treatment. Owing to their young age and comorbid medical conditions, children with optic pathway gliomas are frequently unable to complete standardized VA and or VF testing.
Recent studies have demonstrated that spectral-domain optical coherence tomography (OCT) measures of the circumpapillary retinal nerve fiber layer (RNFL) thickness and ganglion cell–inner plexiform layer thickness are correlated with the magnitude of vision loss and could potentially serve as an objective biomarker of vision in children with optic pathway gliomas. For young children who cannot cooperate with traditional table-mounted devices, a handheld OCT can image young children during sedation.
To date, no studies using handheld OCT have examined the intra- and inter-visit reproducibility of quantitative ganglion cell–inner plexiform layer measures. Establishing the intra- and inter-visit variance is essential to determining how much decline in ganglion cell–inner plexiform layer thickness represents a clinically significant change. We investigated the intra- and inter-visit reproducibility of handheld OCT ganglion cell–inner plexiform layer measurements in sedated children being evaluated for optic pathway gliomas.
Methods
Subjects
Children evaluated in the Neuro-Ophthalmology, Ophthalmology, or Neuro-Oncology clinics at Children’s National Medical Center were recruited to participate in a prospective longitudinal cohort study of handheld OCT. Written informed consent from the parent/guardian and written assent from the child (when applicable) was obtained before study enrollment. The study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board at Children’s National Medical Center. All data collected was HIPAA compliant.
Subjects were eligible for recruitment if they were scheduled to have sedated magnetic resonance imaging (MRI) for their currently diagnosed optic pathway glioma and or neurofibromatosis type 1 (NF1). Subjects that did not have a clinical indication for a sedated MRI were not enrolled in the study. All subjects underwent a comprehensive ophthalmologic examination at time of enrollment and at subsequent study visits. All subjects were required to complete quantitative VA testing at each visit (ie, qualitative measures such as fix and follow were not permitted). VA testing in preverbal children was performed using Teller acuity cards (also known as grating acuity), while older children completed age-appropriate recognition acuity tasks. Vision loss was defined as VA ≥0.2 logMAR above age-based norms, and/or visual field (VF) loss. All subjects, based on their age and ability to cooperate, had their VF assessed by either confrontation or automated or kinetic perimetry techniques. In each eye, VF loss was defined as any appreciable defect in 1 or more quadrants. Subjects with decreased vision secondary to amblyopia or glaucoma, or with a past history of papilledema, were not eligible for study enrollment.
A minimum of 2 acceptable handheld OCT macula scans acquired during a single imaging session were required for enrollment in the intra-visit cohort. Scans with motion artifact, image vignetting, or low signal quality were eliminated from analysis. Subjects that underwent a second imaging session within 6 months were eligible for the inter-visit cohort analysis as long as they did not demonstrate any of the following compared to their initial visit: (1) progressive VA loss, defined as ≥0.2 logMAR change; (2) new or progressive VF loss in any quadrant; and (3) new contrast enhancement or any increase in tumor size on their MRI.
Image Acquisition With Handheld Optical Coherence Tomography
Handheld OCT acquisition was identical to the previously published protocol. One hour before the subject was sedated for the MRI, mydriatic eye drops were instilled. Once the subject was sedated, handheld OCT imaging commenced using a high-resolution handheld device acquiring 36 000 A-scans per second (Bioptigen, Durham, North Carolina, USA); 6 × 6 × 2 mm volume scans centered on the foveola using 300 A-scans across 300 B-scans were acquired.
Handheld Optical Coherence Tomography Image Analysis
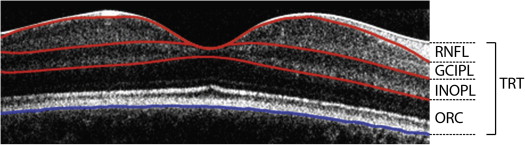
The OCT macular volume image data were segmented using an automated custom-made software program. For each volume image data, the foveola position was manually selected by looking for the largest separation between the junction of the inner and outer segments of the photoreceptors and retinal pigment epithelium as appearing on the horizontal and vertical cross-sectional B-scans. The selected foveola position was then used as the center for thickness measurements within various regions: center (region within 1-mm-diameter circle centered on the foveola); temporal (0–45 degrees and 315–360 degrees), superior (45–135 degrees), nasal (135–225 degrees), and inferior (225–315 degrees) quadrants (regions outside 1-mm-diameter circle and within 3-mm-diameter circle); and global average thickness (region within 3-mm-diameter circle centered on the foveola). Segmentation measured the total retinal thickness and ganglion cell–inner plexiform layer thickness ( Figure 1 ). A graphic description of the image analysis algorithm has previously been published. Algorithm errors were detected in 2 steps: (1) failed frames were defined as an obvious disruption of the detected border, and/or border wandering (detected border jumping to and from different anatomic structures) for larger than 15% consecutive or 20% cumulative of each horizontal frame of a given volume image data; and (2) failed analysis was defined as 15% consecutive or 20% cumulative “failed” frames within a given volume image data.
To assess signal quality, we used the previously described method to calculate the quality index (QI). Two histogram parameters, namely the intensity ratio, comparable to signal-to-noise ratio, and the tissue signal ratio, representative of the ratio of tissue signal pixels vs background noise, are both used to calculate the quality index.
All data were de-identified, not including clinical information, and processed by the same investigator (C.-L.C.). Image quality was as previously described and scans with a quality index value less than 20 were considered to be of poor image quality and discarded.
Statistics
Demographic and clinical characteristics were summarized by standard descriptive statistics. The coefficient of variation (CV) and intraclass correlation coefficient (ICC, 2-way mixed-effects model) was calculated for the global average and anatomic quadrant total retinal thickness and ganglion cell–inner plexiform layer thickness of the intra- and inter-visit cohorts. Since the number of scans acquired beyond the required 2 could vary, the 2 scans with the highest quality index were selected for the intra-visit ICC calculation. The average of all quality qualified scans from visit 1 and visit 2 were used to calculate the inter-visit ICC. Wilcoxon rank-sum test was used to compare CV between vision groups. Each subject with normal vision contributed only 1 eye, which was determined by a random number generator. If the optic pathway glioma was isolated to the optic nerve, the contralateral and unaffected eye was not included in the analysis. Children with abnormal vision in both eyes could contribute 2 eyes to the analysis, but given the potential impact of the inter-eye correlation despite disparate patterns of vision loss in each eye, the intra-visit CV analysis results were confirmed by repeating the analysis using only 1 subject eye. A post hoc analysis using a multivariable linear regression model investigated the influence of patient age and diagnosis (optic pathway glioma secondary to NF1 vs sporadic optic pathway glioma) on CV measures. Data were analyzed using commercially available software (STATA, version 13; StataCorp, College Station, Texas, USA).
Results
Intra-visit Cohort
Thirty-one subjects contributed a single eye with normal vision and 11 subjects contributed 14 eyes with abnormal vision. The clinical and demographic features of the intra-visit cohort are listed in Table 1 . One-hundred twenty-eight acquisitions met inclusion criteria and were included in the analysis. CV, ICC, and ICC 95th percentile confidence of total retinal thickness and ganglion cell–inner plexiform layer thickness are listed in Table 2 for the intra-visit cohort. The CV of total retinal thickness was significantly different between vision groups ( P < .05) only in the inferior quadrant, although it neared significance for the superior quadrant (z = 1.8, P = .069). Ganglion cell–inner plexiform layer CV was significantly different between groups only in the superior quadrant ( P < .05), but also neared significance in the inferior quadrant (z = −1.9, P = .055). The CV between groups did not significantly change if the vision loss group restricted subjects to contributing only 1 eye ( P > .05, all comparisons). All ICC values for the total retinal thickness and ganglion cell–inner plexiform layer were above 0.950 except for the temporal quadrant of the normal vision group (ICC = 0.936). Using multivariable linear regression, patient age and diagnosis (optic pathway glioma secondary to neurofibromatosis type 1 vs sporadic optic pathway glioma) failed to demonstrate a statistically significant influence on CV.
| Characteristics | Abnormal Vision (N = 11) a | Normal Vision (N = 31) |
|---|---|---|
| Age (median), y | 5.3 | 5.4 |
| Range | 1.0–8.2 | 0.79–13.0 |
| Female sex, n (%) | 7 (64) | 20 (65) |
| Race, n (%) | ||
| Asian | 1 (9) | – |
| Black | 1 (9) | 5 (16) |
| Multiracial | – | 4 (13) |
| White | 9 (82) | 22 (71) |
| Diagnosis, n (%) | ||
| NF1with optic pathway glioma | 4 (36) | 21 (68) |
| Sporadic optic pathway glioma | 7 (64) | 5 (16) |
| NF1 without optic pathway glioma | – | 5 (16) |
| Abnormal Vision (N = 14) | Normal Vision (N = 31) | |||||
|---|---|---|---|---|---|---|
| Thickness ± SD | CV (%) ± SD | ICC (95% CI) | Thickness ± SD | CV (%) ± SD | ICC (95% CI) | |
| TRT | ||||||
| Average | 397 ± 25 | 0.3 ± 0.1 | 0.998 (0.99, 0.99) | 436 ± 21 | 0.3 ± 0.2 | 0.996 (0.99, 0.99) |
| Temporal | 387 ± 23 | 0.5 ± 0.3 | 0.994 (0.98, 0.99) | 423 ± 22 | 0.7 ± 0.6 | 0.988 (0.97, 0.99) |
| Superior | 399 ± 23 | 0.6 ± 0.3 | 0.993 (0.98, 0.99) | 441 ± 20 | 0.5 ± 0.3 | 0.991 (0.98, 0.99) |
| Nasal | 397 ± 30 | 0.3 ± 0.2 | 0.997 (0.99, 0.99) | 437 ± 22 | 0.5 ± 0.4 | 0.990 (0.97, 0.99) |
| Inferior a | 406 ± 27 | 0.4 ± 0.4 | 0.995 (0.98, 0.99) | 445 ± 21 | 0.6 ± 0.4 | 0.988 (0.97, 0.99) |
| GCIPL | ||||||
| Average | 93 ± 12 | 2.1 ± 1.5 | 0.993 (0.97, 0.99) | 130 ± 12 | 1.5 ± 0.9 | 0.981 (0.96, 0.99) |
| Temporal | 90 ± 17 | 3.8 ± 2.1 | 0.983 (0.95, 0.99) | 124 ± 12 | 3.1 ± 2.1 | 0.936 (0.86, 0.96) |
| Superior a | 95 ± 19 | 4.4 ± 2.8 | 0.973 (0.91, 0.99) | 134 ± 13 | 2.1 ± 1.3 | 0.983 (0.96, 0.99) |
| Nasal | 91 ± 24 | 3.9 ± 3.1 | 0.986 (0.95, 0.99) | 129 ± 15 | 2.3 ± 2.4 | 0.955 (0.90, 0.97) |
| Inferior | 95 ± 21 | 4.5 ± 3.2 | 0.968 (0.90, 0.98) | 132 ± 13 | 2.7 ± 2.1 | 0.951 (0.90, 0.97) |
Inter-visit Cohort
A total of 144 volumes from 25 eyes (21 unique subjects) comprised the inter-visit cohort. One subject from the intra-visit cohort was not eligible for inclusion owing to progressive vision loss and tumor growth. Table 3 lists CV, ICC, and ICC 95th percentile confidence interval for total retinal thickness and ganglion cell–inner plexiform layer measures for the inter-visit cohort. The CV of total retinal thickness was not significantly different in any quadrant between vision groups. The ganglion cell–inner plexiform layer CV was not statistically different between groups for the average and all quadrants ( P > .05 for all comparisons), except for the inferior quadrant (Z = 1.98, P = .047). The magnitude of differences between vision loss groups was relatively small, as demonstrated in Bland-Altman plots for ganglion cell–inner plexiform layer average and quadrants ( Figures 2–6 ).
| Abnormal Vision (N = 8) | Normal Vision (N = 17) | |||||
|---|---|---|---|---|---|---|
| Thickness ± SD | CV (%) ±SD | ICC (95% CI) | Thickness ± SD | CV (%) ± SD | ICC (95% CI) | |
| TRT | ||||||
| Average | 402 ± 27 | 0.9 ± 0.8 | 0.985 (0.93, 0.99) | 433 ± 25 | 0.7 ± 0.6 | 0.987 (0.96, 0.99) |
| Temporal | 393 ± 23 | 1.2 ± 0.9 | 0.970 (0.84, 0.99) | 422 ± 25 | 0.7 ± 0.6 | 0.986 (0.96, 0.99) |
| Superior | 401 ± 24 | 0.9 ± 0.7 | 0.982 (0.91, 0.99) | 437 ± 25 | 0.5 ± 0.4 | 0.991 (0.97, 0.99) |
| Nasal | 399 ± 33 | 1.1 ± 0.5 | 9.989 (0.97, 0.99) | 432 ± 27 | 0.8 ± 0.6 | 0.985 (0.96, 0.99) |
| Inferior | 412 ± 28 | 1.1 ± 0.9 | 0.980 (0.90, 0.99) | 441 ± 26 | 0.9 ± 0.8 | 0.975 (0.93, 0.99) |
| GCIPL | ||||||
| Average | 94 ± 20 | 2.3 ± 1.4 | 0.994 (0.97, 0.99) | 127 ± 16 | 1.6 ± 1.0 | 0.988 (0.97, 0.99) |
| Temporal | 93 ± 17 | 2.6 ± 1.8 | 0.987 (0.93, 0.99) | 123 ± 14 | 2.7 ± 2.2 | 0.959 (0.88, 0.98) |
| Superior | 95 ± 22 | 3.7 ± 4.2 | 0.980 (0.90, 0.99) | 132 ± 17 | 2.4 ± 1.9 | 0.971 (0.92, 0.98) |
| Nasal | 90 ± 25 | 1.9 ± 1.9 | 0.995 (0.98, 0.99) | 124 ± 19 | 2.7 ± 2.0 | 0.974 (0.93, 0.99) |
| Inferior a | 97 ± 21 | 5.2 ± 2.8 | 0.971 (0.85, 0.99) | 129 ± 16 | 2.4 ± 2.1 | 0.972 (0.92, 0.98) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


