Purpose
To report the long-term functional and anatomic outcomes of osteo-odonto-keratoprosthesis and tibial bone keratoprosthesis; to analyze the influence of clinical factors, such as surgical technique, primary diagnosis, age, and postoperative complications, on the final outcome.
Design
Retrospective cohort study.
Methods
setting: Centro de Oftalmología Barraquer, between 1974 and 2005. Participants: Two hundred twenty-seven patients. intervention: Biological keratoprosthesis using osteo-odonto-keratoprosthesis or tibial bone keratoprosthesis. main outcome measures: Functional survival with success defined as best-corrected visual acuity ≥0.05; anatomic survival with success defined as retention of the keratoprosthesis lamina.
Results
Osteo-odonto-keratoprosthesis and tibial bone keratoprosthesis have comparable anatomic survival at 5 and 10 years of follow-up, but osteo-odonto-keratoprosthesis has a significantly better functional success than tibial bone keratoprosthesis at the same time periods. Among the primary diagnoses, Stevens-Johnson syndrome, chemical burn, and trachoma have generally good functional and anatomic outcomes and the least favorable prognosis is for ocular cicatricial pemphigoid. Younger patients fared better than those in older age groups. The most frequent complications were extrusion (28%), retinal detachment (16%), and uncontrolled glaucoma (11%). The glaucoma group had the best anatomic success but the worst functional results, only exceeded by the retinal detachment group in terms of functional outcome.
Conclusion
Clinical factors, such as surgical technique, primary diagnosis, age, and postoperative complications, can affect the long-term anatomic and functional successes of biological keratoprosthesis. Knowledge about the impact of each of these factors on survival can help surgeons determine the best approach in every particular case.
It was Guillaume Pellier de Quengsy, a French ophthalmologist, who first proposed in 1771 the replacement of an opaque cornea with an “artificial cornea,” using a glass cylinder mounted onto a metal ring. His monograph, published in 1789, is probably the first on keratoprosthesis. Since then, several modifications on the surgical technique, as well as the materials used, have been developed in search of the ideal artificial cornea with the best possible functional and anatomic outcomes.
In 1963, Strampelli described the use of an acrylic optical cylinder mounted onto an osteo-dental lamina from the patient, thus calling the technique osteo-odonto-keratoprosthesis. Nowadays, osteo-odonto-keratoprosthesis is considered a viable treatment in the majority of bilateral, end-stage corneal opacifications with severe dry eye and high risk of corneal graft rejection. At our institution, we started employing this technique in 1964. In 1980, Temprano modified Strampelli’s technique by using the patient’s tibial bone in edentulous patients or deciduous teeth in very young patients. Moreover, he performed lens extraction whether or not there was a cataract in order to avoid further surgical intervention after osteo-odonto-keratoprosthesis implantation. We decided to name this technique tibial bone keratoprosthesis.
In 1 of our recent publications on the long-term functional and anatomic outcomes of osteo-odonto-keratoprosthesis versus tibial bone keratoprosthesis, we reported that osteo-odonto-keratoprosthesis demonstrated a tendency toward better anatomic outcomes compared with tibial bone keratoprosthesis, although the difference was not statistically significant during the follow-up period of 10 years. As for functional results, osteo-odonto-keratoprosthesis did not differ from tibial bone keratoprosthesis at year-2 follow-up, but was significantly better at year-10 follow-up. The aim of the present study is to analyze the influence of different clinical factors, such as primary diagnosis, age, and postoperative complications, on anatomic and functional outcomes when combining osteo-odonto-keratoprosthesis and tibial bone keratoprosthesis.
Materials and Methods
We reviewed the clinical data of 227 patients who underwent tibial bone keratoprosthesis (n = 82) or osteo-odonto-keratoprosthesis (n = 145) at the Centro de Oftalmología Barraquer between January 1974 and December 2005.
Surgical Procedure
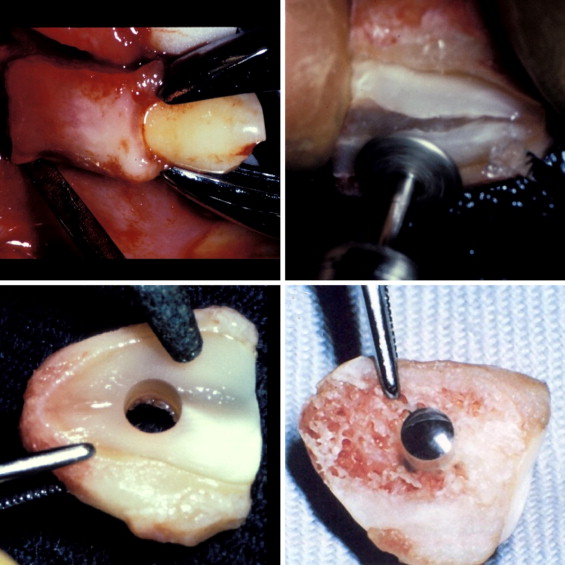
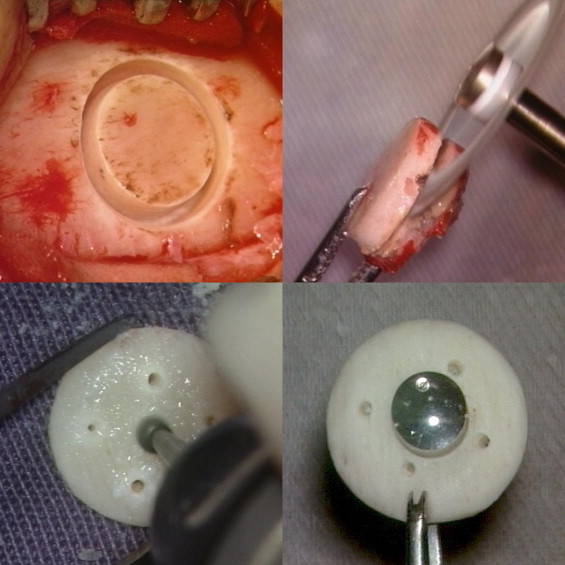
At our institution, keratoprosthesis surgery is performed in two stages. The first stage involves the following: clean-up of the ocular surface through superficial keratectomy and the release of any existing symblepharon, harvesting of a full-thickness buccal mucosal graft from the inner lower lip of the patient to be implanted onto the entire ocular surface, harvesting of a canine tooth (after radiologic examination of the mouth to confirm canine tooth and root viability) and molding of the osteo-dental lamina, and assembly of the optical cylinder onto the osteo-dental lamina and its insertion into the inferior orbital subcutaneous pocket for biointegration for 3 months. The second stage is performed 3 months later and consists of retrieval of the biointegrated piece from the inferior orbital pocket, lifting of the buccal mucosal graft, central corneal trephination, lens and iris extraction, implantation of the prosthesis into the corneal bed, and replacement of the partially lifted buccal mucosa. In edentulous or very young patients without permanent teeth, or when prognosis is very poor, we prefer to perform a less invasive procedure using the tibial bone. A round rotating saw is used to harvest the lamina from the upper third of the inner side of the tibial bone (after radiologic examination of the lower leg to confirm bone viability), which is then molded to accommodate the acrylic optical cylinder ( Figures 1 and 2 ).
Measurements and Definition of Success
The visual acuity (VA) of all patients was measured preoperatively and postoperatively using decimal scale values that were converted into logMAR scale values. No light perception was defined as 0 in the decimal VA scale, light perception as 0.00001, light projection as 0.0001, and counting fingers as 0.001. We defined functional success as best-corrected decimal visual acuity (BCVA) ≥0.05, while anatomic success was defined as retention of the keratoprosthesis lamina.
Statistical Analysis
Statistical analysis was performed using Kaplan-Meier survival curves. To avoid possible data autocorrelations, only one operated eye per patient was included in this analysis. Based on the Kaplan-Meier analysis, estimates for 5- and 10-year success with 95% confidence interval (CI) were calculated for the functional and anatomic survival curves. The Breslow (generalized Wilcoxon) test, Tarone-Ware test, and log-rank (Mantel-Cox) test were used to compare survival functions. The Breslow test measures early-term differences in survival; the Tarone-Ware test measures intermediate term; and the log-rank test measures the end-term differences in success relative to the survival curve. Multivariate analysis (Cox regression model) was applied to test the impact of the different clinical factors on functional and anatomic survival. The following variables were included for analysis: surgical technique, primary diagnosis, age, and postoperative complications. A P value less than .05 was assigned to indicate a statistically significant difference. All analyses were performed using STATISTICA 6.1 (Hille and Lewicki 2007: Statistics Methods and Applications; Starsoft, Tulsa, Oklahoma, USA) and SPSS 13 (SPSS Inc, Chicago, Illinois, USA).
Results
A total of 330 eyes in 227 patients underwent osteo-odonto-keratoprosthesis or tibial bone keratoprosthesis from 1974 to 2005. Of these, only one eye in the bilateral cases was included in the analysis to minimize statistical bias. Thus, 145 eyes were from the osteo-odonto-keratoprosthesis group and 82 eyes were from the tibial bone keratoprosthesis group. Patients were generally followed up weekly during the first month and monthly during the first 6 months. Subsequent follow-ups were determined based on the clinical course of each case. Patients with follow-up time less than one month were not included in the study. The mean follow-up time was 8.4 years for osteo-odonto-keratoprosthesis (range: 1 month to 30 years) and 3.5 years for tibial bone keratoprosthesis (range: 1 month to 12.5 years). The mean age of patients was 43 years (range: 10 to 81 years) for osteo-odonto-keratoprosthesis and 53 years (range: 14 to 86 years) for tibial bone keratoprosthesis. Male subjects were predominant in both groups, with 70% for the osteo-odonto-keratoprosthesis group and 62% for the tibial bone keratoprosthesis group.
For all 227 patients, the mean preoperative logMAR BCVA was 3.208 ± 0.926 SD (range: 1.000–5.000), corresponding to a decimal BCVA of 0.00062 (range: light perception to 0.10). The mean maximum postoperative logMAR BCVA was 0.803 ± 1.199 SD (range: 0.000–5.000), corresponding to a decimal BCVA of 0.158 (range: light perception to 1.00). At last follow-up, the mean logMAR BCVA was 2.290 ± 1.985 SD (range: 0.000–5.000), corresponding to a decimal BCVA of 0.00153 (range: light perception to 1.00) ( Figure 3 ).
Chemical burn was the most common primary diagnosis in both groups, accounting for 39% of cases. The majority of common postoperative complications were similar in both groups, with implant extrusion being the most common, followed by retinal detachment, glaucoma, and infection. Table 1 gives a summary of the different clinical factors under study in the osteo-odonto-keratoprosthesis and tibial bone keratoprosthesis groups.
| OOKP (n = 145) | Tibial Bone KPro (n = 82) | OOKP & Tibial Bone KPro | |
|---|---|---|---|
| Age | |||
| 10–29 years | 31% | 13% | 25% |
| 30–49 years | 33% | 29% | 32% |
| 50–69 years | 30% | 34% | 31% |
| 70–89 years | 6% | 23% | 12% |
| Maximum visual acuity a | |||
| <0.05 | 12% | 15% | 13% |
| 0.05–0.2 | 16% | 29% | 21% |
| 0.3–0.7 | 24% | 33% | 27% |
| 0.8–1.0 | 48% | 23% | 39% |
| Primary diagnosis | |||
| Chemical burn | 43% | 31% | 39% |
| Thermal burn | 10% | 7% | 9% |
| SJS or Lyell syndrome | 15% | 11% | 13% |
| OCP | 6% | 21% | 11% |
| Trachoma | 17% | 2% | 11% |
| Other or not assignable | 10% | 28% | 17% |
| Postoperative complication | |||
| Extrusion | 28% | 28% | 28% |
| Infection | 12% | 2% | 9% |
| Vitreous hemorrhage | 3% | 2% | 3% |
| Retinal detachment | 18% | 13% | 16% |
| Glaucoma | 10% | 13% | 11% |
| Retroprosthetic membrane | 3% | 9% | 5% |
a Maximum visual acuity is the best visual acuity ever achieved after the last step of the implantation of the keratoprosthesis (in decimal values).
Clinical Factors
Surgical technique
In the survival curves, the 5-year anatomic survival was 73.7% in the osteo-odonto-keratoprosthesis group and 65.1% in the tibial bone keratoprosthesis group, while the 10-year anatomic survival was 60% in the osteo-odonto-keratoprosthesis group and 48% in the tibial bone keratoprosthesis group ( Figure 4 , Upper left). The log-rank (Mantel-Cox) test showed no statistically significant difference between the 2 techniques ( P = .0792). Also, the Tarone-Ware and Breslow (generalized Wilcoxon) test results were not significant ( P = .0891 and P = .0993, respectively). The 5-year functional survival for the osteo-odonto-keratoprosthesis group was 50%, compared with the tibial bone keratoprosthesis group, which was only 29%. The 10-year functional survival was 39% in the osteo-odonto-keratoprosthesis group and 17% in the tibial bone keratoprosthesis group ( Figure 4 , Upper right). The log-rank test (Mantel-Cox) was statistically significant ( P = .0019), as well as the Tarone-Ware and Breslow tests ( P = .0069 and P = .0196, respectively).
Primary diagnosis
Diagnostic categories were divided into 6 groups: chemical burn, thermal burn, Stevens-Johnson/Lyell syndrome, ocular cicatricial pemphigoid, trachoma, and others. Figure 5 , Upper right and left, demonstrates the functional and anatomic success through time of the different diagnostic categories. The best functional survival at 5 years was for the Stevens-Johnson syndrome group, followed by the trachoma and chemical burn groups. As regards 10-year survival, the Stevens-Johnson syndrome group, followed by the chemical burn and trachoma groups, demonstrated the best functional results. The best anatomic survival at 5 years was for the thermal burn group, followed by the trachoma and chemical burn groups. The 10-year anatomic survival was best for the thermal burn group, followed by the chemical burn and Stevens-Johnson syndrome groups. The ocular cicatricial pemphigoid group had the worst outcomes for anatomic survival at year-5 and year-10 follow-ups, while the thermal burn group had worst functional survival at year-5 and year-10 follow-ups. The 5-year functional and anatomic survivals for the 2 different techniques with respect to clinical diagnosis are contrasted in Figure 6 , Upper right and left; the 10-year results are shown in Figure 7 , Upper right and left.
Age
Patients were divided into the following age groups: 10 to 29 years, 30 to 49 years, 50 to 69 years, and 70 to 89 years. Figure 5 , Center right and left, shows the functional and anatomic survival curves through time of the different age groups. Patients in the youngest age group had the best 5-year functional survival at 57%, while the best 5-year anatomic survival was for the oldest age group (70–89 years) at 85%. The best 10-year functional survival is similar to the best results for the youngest age group at 47%, and best 10-year anatomic survival for the 30-to-49-year age group was 70%. The 5-year functional and anatomic survivals for the 2 different techniques with respect to age are contrasted in Figure 6 , Center right and left; the 10-year results are shown in Figure 7 , Center right and left.
Postoperative complications
The most common postoperative complications were extrusion of the keratoprosthesis lamina (28%; 63/227), retinal detachment (16%; 37/227), uncontrolled glaucoma (11%; 25/227), infection (9%; 20/227), retroprosthetic membrane (5%; 11/227), and vitreous hemorrhage (3%; 7/227). Figure 5 , Lower right and left, shows the functional and anatomic survival of the different postoperative complications. Those without complications, as expected, had the best functional survival, with 57% survival at 5 years and 42% survival at 10 years. As for 5- and 10-year anatomic survival, the best retention was found in cases with glaucoma as the only complication, with 90% survival with respect to both parameters. The 5-year functional and anatomic survivals for the 2 different techniques with respect to postoperative complications are contrasted in Figure 6 , Lower right and left; the 10-year results are shown in Figure 7 , Lower right and left.
Multivariate Analysis
Cox regression analysis of the different clinical factors ( Table 2 ) shows that the surgical technique (osteo-odonto-keratoprosthesis or tibial bone keratoprosthesis) had significant impact on functional survival ( P = .008) as well as anatomic survival ( P = .049). The hazard ratio for functional failure for tibial bone keratoprosthesis is 1.762 times that of osteo-odonto-keratoprosthesis. As for primary diagnosis, only ocular cicatricial pemphigoid had a significant impact on anatomic survival versus chemical burn ( P = .010). Postoperative complications, such as glaucoma ( P = .026) and retinal detachment ( P > .0001), had significant impact on functional survival but not on anatomic survival. With retinal detachment, the hazard ratio for functional failure is 2.455 times that without retinal detachment. As for other factors, such as age and gender, no statistically significant difference was found in the above-mentioned groups.



