Purpose
To evaluate the short-term results of glued intrascleral fixation of posterior chamber intraocular lens (glued IOL) in children without adequate capsular support.
Design
Noncomparative retrospective observational case series.
Patients
Setting: Institutional practice. Methods: Forty-one eyes of 33 children who underwent glued IOL implantation were retrospectively evaluated. The indications were postsurgical aphakia, subluxated cataract, ectopia lentis, traumatic subluxation, and decentered IOL. Main outcome measures: Visual acuity (VA), endothelial cell changes, intraoperative and postoperative complications.
Results
The mean age at the time of glued IOL was 10.7 ± 3.6 years (range 5−15). The mean duration of follow-up after surgery was 17.5 ± 8.5 months (range 12-36). The mean postoperative best spectacle-corrected visual acuity (BCVA in decimal equivalent) was 0.43 ± 0.33 and there was significant change noted ( P < 0.001). Postoperatively, 20/20 and >20/60 BCVA was obtained in 17.1% and 46.3% of eyes respectively. BCVA improvement more than 1 line was seen in 22 eyes (53.6%). The mean postoperative refraction was myopic (−1.19 ± 0.7 diopters [D]) in 19 eyes and hyperopic (+1.02 ± 0.7 D) in 22 eyes. The mean endothelial loss was 4.13% (range 1.3%-5.94%). The 3 causes of reduced BCVA were the preexisting corneal, retinal pathology, and amblyopia. Postoperative complications included optic capture in 1 eye (2.4%), macular edema in 2 eyes (4.8%), and clinical decentration in 2 eyes (4.8%). There was no postoperative retinal detachment, IOL dislocation, endophthalmitis, or glaucoma.
Conclusion
Short-term results in children after glued IOL were favorable, with a low rate of complications. However, regular follow-ups are required since long-term risks are unknown.
Intraocular lens (IOL) implantation after cataract surgery in children has been challenging for ophthalmic surgeons. With excellent results seen in adults, issues such as the surgical technique, choice of the lens, and dioptric power of the lens are constantly being refined and adapted to children’s growing eyes. In eyes with an intraoperative large posterior capsular rent or preexisting ectopia lentis, IOL implantation becomes further complicated by lack of normal capsular support. Anterior chamber (AC) IOLs or sutured scleral fixated IOLs have been performed in such cases. Scleral fixated IOLs, by virtue of their anatomic location, offer numerous advantages over the AC IOL. Glued intrascleral fixation places a posterior chamber (PC) IOL in eyes with deficient capsules using a quick-acting surgical fibrin sealant derived from human blood plasma, with both hemostatic and adhesive properties. We have performed intrascleral IOL fixation with fibrin glue (glued IOL) in adult eyes with deficient capsules in the recent past and have had encouraging results. This study was undertaken to evaluate the postoperative outcome and complications after glued intrascleral PC IOLs in children with no capsular support.
Materials and Methods
This is a retrospective case series of children who underwent intrascleral IOL fixation with fibrin glue (glued IOL). Eyes operated with glued IOL from January 1, 2008 to January 1, 2010 were included. Children in the age group 5 to 15 years and who came for regular follow-up were included. The preoperative indications for the glued IOL procedure were aphakia with absent capsules, subluxated cataracts, ectopia lentis, traumatic subluxation, and decentered IOLs. Patients who were uncooperative and those who were lost to follow-up were excluded. Uncorrected visual acuity (UCVA), best spectacle-corrected visual acuity (BCVA) with Snellen visual acuity charts, retinoscopy, intraocular pressure (noncontact tonometry), slit-lamp biomicroscopy, dilated fundus examination, and anterior chamber cellular reaction (Standardization of Uveitis Nomenclature) were analyzed. Endothelial cell count and percentage of specular cell loss were determined by semi-automated analysis of endothelial pictures (SP-2000P; Topcon, Tokyo, Japan). Postoperative residual power was obtained from manual refraction and autorefractometer. The dioptric power of postoperative manifest refraction was taken for statistical analysis. Single-piece rigid polymethylmethacrylate (PMMA) IOL (Appasamy Associates, Chennai, India) and foldable 3-piece silicone IOL (Sofport; Bausch & Lomb, Rochester, New York, USA) were the type of IOLs implanted. The IOL power was calculated from SRK II formula and emmetropia was targeted using the A-scan and IOL Master (Carl Zeiss Meditec, Dublin, California, USA). In case of eyes with severe trauma, fellow eye refraction was considered for IOL power determination.
Surgical Technique
All surgeries were performed under general anesthesia. Two partial-thickness scleral flaps about 2.5 × 2.5 mm were created exactly 180 degrees diagonally apart. Either an infusion cannula or AC maintainer was fixed. In eyes with PCR or aphakia, anterior vitrectomy was performed to release any traction or vitreous in the pupillary plane. Two straight sclerotomies with a 20-gauge (G) needle were made under the existing scleral flaps about 1 mm from the limbus. In eyes with subluxated cataract or ectopia lentis, lensectomy by the vitrectomy probe was performed. The PC IOL was then introduced through the limbal incision using either a McPherson forceps (for rigid IOL) or an injector (for foldable IOL). An end-gripping 23-G micro rhexis forceps (Micro Surgical Technology, Redmond, Washington, USA) was passed through 1 of the sclerotomies to hold the haptic tip. The haptics were then externalized under the scleral flap. A circumferential scleral tunnel was made with a 26-G needle at the point of externalization of the haptic and the haptic was tucked into the intralamellar scleral tunnel. The scleral flaps were then closed with fibrin glue (Tisseel; Baxter, Deerfield, Illinois, USA). The infusion cannula or AC maintainer was subsequently removed. The limbal wound was closed with 10–0 monofilament nylon sutures. The conjunctiva was also apposed with the fibrin glue in all eyes.
Postoperative Period
All patients were prescribed topical 1% predisolone acetate and 0.3% gatifloxacin in the postoperative period (2 weeks). Mydriatic drops were instilled 3 times a day for the first 3 days.
Amblyopia Therapy
Amblyopia treatment was introduced 2 weeks after surgery. Occlusion treatment (full occlusion) was started and followed up every 3 months for evaluation. In unilateral cases, the better eye was occluded for 6 days and the operated eye for 1 day. In bilateral cases alternate-day occlusion was followed.
Statistical Analysis
Data were entered in a Microsoft Excel spreadsheet (Microsoft Corp, Redmond, Washington, USA), and was analyzed using SPSS version 16.1(SPSS Inc, Chicago, Illinois, USA). Differences were considered statistically significant at P < .05.
Results
Forty-one eyes (25 unilateral and 8 bilateral) of 33 children underwent glued intrascleral fixation of posterior chamber IOL in the described period ( Table 1 ). The mean follow-up was 17.5 ± 8.5 months (range 12–36) and the mean age was 10.7 ± 3.6 years (range 5–15). The indications were aphakia (n = 15), subluxated cataract (n = 14), ectopia lentis (n = 9), traumatic subluxation (n = 2) and decentered IOL (n = 1). The indication for PC IOL implantation was primary in 25 eyes and secondary in16 eyes. The mean preoperative and postoperative UCVA was 0.04 ± 0.05 and 0.25 ± 0.21 respectively. There was significant improvement in UCVA (Wilcoxon test, P < 0.001). The mean postoperative best spectacle-corrected visual acuity was 0.43 ± 0.33 and there was significant change in BCVA ( P < 0.001). There was no significant correlation between the age of the children and postoperative UCVA ( P = .407, R 2 = 0.018) and BCVA ( P = .303, R 2 = 0.027) ( Figure 1 ) .
| Patient | Age (Years) | Sex | Indication | Preoperative UCVA | Postoperative UCVA | Postoperative BCVA | Specular Loss % | Follow-up (Months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 11 | F | A | 0.01 | 0.5 | 1 | 4.29 | 14 |
| 2 | 15 | M | A | 0.01 | 0.5 | 1 | 2.86 | 12 |
| 3 | 9 | M | TS | 0.25 | 0.33 | 1 | 5.36 | 12 |
| 4 | 15 | M | SC | 0.25 | 0.33 | 1 | 4.93 | 16 |
| 15 | M | SC | 0.1 | 0.66 | 1 | 3.21 | 24 | |
| 5 | 13 | M | TS | 0.01 | 0.25 | 1 | 4.7 | 24 |
| 6 | 8 | F | SC | 0.01 | 0.1 | 0.33 | 3.78 | 12 |
| 7 | 5 | M | EL | 0.01 | 0.33 | 0.66 | 4.32 | 28 |
| 5 | M | EL | 0.03 | 0.33 | 0.66 | 3.88 | 24 | |
| 8 | 12 | F | A | 0.01 | 1 | 1 | 3.88 | 16 |
| 9 | 15 | F | A | 0.01 | 0.16 | 0.33 | 2.69 | 12 |
| 15 | F | A | 0.01 | 0.16 | 0.33 | 5.94 | 12 | |
| 10 | 13 | M | SC | 0.01 | 0.01 | 0.1 | 4.35 | 12 |
| 11 | 9 | M | SC | 0.03 | 0.25 | 0.33 | 4.71 | 12 |
| 12 | 15 | M | SC | 0.08 | 0.25 | 0.5 | 1.72 | 12 |
| 13 | 12 | M | SC | 0.05 | 0.06 | 0.1 | 2.53 | 13 |
| 24 | 15 | M | SC | 0.03 | 0.03 | 0.03 | 5.15 | 12 |
| 15 | M | SC | 0.1 | 0.33 | 0.5 | 4.26 | 12 | |
| 15 | 15 | M | A | 0.1 | 0.33 | 0.5 | 4.43 | 12 |
| 16 | 5 | M | A | 0.01 | 0.25 | 0.66 | 3.9 | 24 |
| 17 | 13 | M | A | 0.01 | 0.03 | 0.03 | 4.01 | 12 |
| 18 | 5 | M | A | 0.01 | 0.25 | 0.25 | 5.18 | 12 |
| 19 | 10 | M | SC | 0.1 | 0.16 | 0.16 | 4.76 | 12 |
| 20 | 5 | F | DI | 0.01 | 0.03 | 0.1 | 1.3 | 36 |
| 21 | 8 | M | SC | 0.01 | 0.01 | 0.16 | 5.18 | 12 |
| 22 | 12 | M | EL | 0.06 | 0.25 | 0.33 | 3.9 | 36 |
| 12 | M | EL | 0.06 | 0.1 | 0.1 | 4.59 | 36 | |
| 23 | 10 | M | SC | 0.03 | 0.03 | 0.03 | 4.33 | 12 |
| 24 | 6 | M | SC | 0.05 | 0.33 | 0.5 | 3.08 | 12 |
| 25 | 11 | F | A | 0.05 | 0.06 | 0.06 | 5.41 | 14 |
| 26 | 6 | M | SC | 0.05 | 0.66 | 0.66 | 3.08 | 12 |
| 27 | 14 | F | A | 0.01 | 0.01 | 0.01 | 4.46 | 13 |
| 28 | 8 | F | A | 0.01 | 0.16 | 0.33 | 3.14 | 12 |
| 29 | 14 | F | A | 0.03 | 0.66 | 0.66 | 3.03 | 12 |
| 30 | 12 | F | EL | 0.16 | 0.33 | 0.33 | 5.63 | 12 |
| 31 | 7 | F | A | 0.01 | 0.1 | 0.1 | 5.37 | 12 |
| 7 | F | A | 0.01 | 0.1 | 0.1 | 4.55 | 12 | |
| 32 | 7 | M | EL | 0.01 | 0.16 | 0.33 | 5.65 | 24 |
| 7 | M | EL | 0.01 | 0.16 | 0.33 | 2.6 | 30 | |
| 33 | 15 | F | EL | 0.03 | 0.33 | 0.66 | 5.19 | 36 |
| 15 | F | EL | 0.03 | 0.33 | 0.66 | 4.24 | 36 |
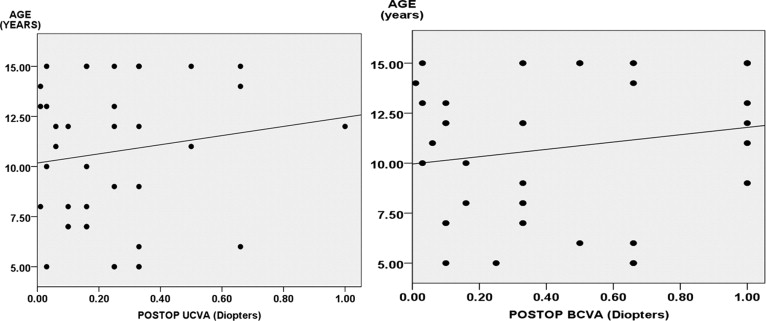
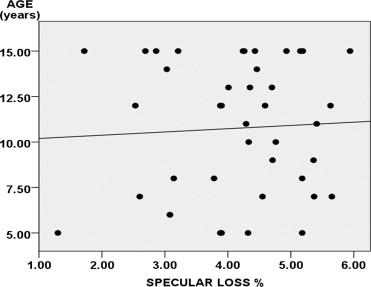
The mean preoperative and postoperative endothelial density was 2411.9 ± 355.6 cells/mm 2 and 2311.8 ± 345.4 cells/mm 2 respectively. There was significant reduction ( P < 0.001) in the endothelial cells in the postoperative period. The mean corneal endothelial cell loss was 4.13% (range 1.3%-5.94%). There was no significant correlation ( P = .742, R 2 = 0.003) between percentage loss of specular count and age of the children ( Figure 2 ) .
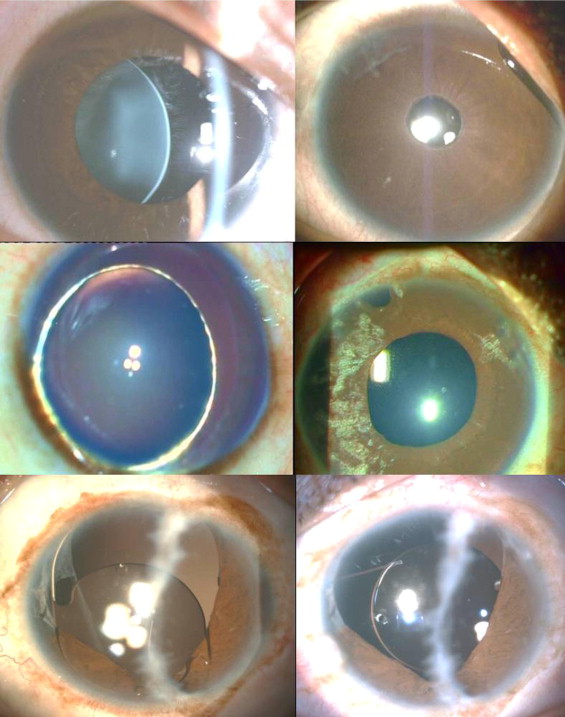
There were no intraoperative complications seen in our case series. However, postoperatively, 1 of the 41 eyes (2.4%) had optic capture and 2 (4.8%) had clinical decentration. IOL was repositioned surgically in the 2 eyes with decentration. Postoperative macular edema was seen in 2 out of 41 eyes (4.8%). There was no significant rise ( P = .127) in IOP and no uveitis or retinal detachment reported in the subsequent follow-up. There was no wound leak or hypotony seen in any of the eyes in the early (<2 months) or late (>2 months) postoperative period ( Figure 3 ) . Good corneal clarity was noted in the immediate postoperative follow-up ( Figure 4 ) . There was no clinically significant pupil distortion or pigment deposition on the IOL optic surface. The mean postoperative spherical equivalent was −0.25 ± 1.1 diopters (D). The mean postoperative manifest refraction was myopic in 19 eyes and hyperopic in 22 eyes. The mean postoperative myopia was −1.19 ± 0.7 D (19 eyes) and the mean postoperative hyperopia was +1.02 ± 0.7 D (22 eyes) ( Figure 5 ) . Good IOL centration was clinically seen in all eyes in the last follow-ups. There was no loss of BCVA in any of the eyes in the subsequent follow-up.