Glaucoma
Deborah Pavan-Langston
Stacey C. Brauner
Cynthia L. Grosskreutz
I. Definition, Incidence, and Risk Factors
Glaucoma is a condition in which there is damage to the optic nerve and loss of retinal ganglion cells that result in visual field loss. Intraocular pressure (IOP) is the major modifiable risk factor in glaucoma, and treatment strategies for the disease include medications, lasers, and surgery to decreased the pressure and preserve functional vision throughout the patient’s lifetime. Glaucoma is the third leading cause of blindness worldwide behind cataract and trachoma, and in the United States, it is the third leading cause of blindness behind cataract and macular degeneration. Approximately 1.25 million Americans have the diagnosed condition, but another 1 million Americans have glaucoma and are unaware of it. Nearly 120,000 are bilaterally blind, and 1.6 million have visual field defects. It is the single most frequent irreversible cause of blindness among African Americans, and it affects more than 2% of all whites. Detection of glaucoma patients is, therefore, an important public health problem. There are more than 40 types of glaucoma. Glaucoma can also affect younger people, and measurement of eye pressure is an important part of a routine eye examination. Risk factors for glaucoma include high IOP, old age, African American race, family history of glaucoma, myopia, diabetes, and high blood pressure. The disease in primary form is hereditary by a yet-undefined polygenic mechanism.
II. Physiologic Mechanisms of Various Glaucomas
Aqueous humor is produced by the ciliary body and flows into the posterior chamber, then between the posterior iris surface and lens, around the pupil edge, into the anterior chamber. It exits from the anterior chamber via trabecular and nontrabecular routes. The trabecular route is at the angle of the anterior chamber, formed by the iris base and peripheral cornea, flowing through the trabecular meshwork (TM) of the sclera, into Schlemm’s canal. Via the collector channels in the sclera, the aqueous is carried to the episcleral vessels, where aqueous mixes with blood. On slitlamp examination, clear limbal aqueous veins can often be observed carrying aqueous into blood-filled episcleral veins. The latter can be identified by a laminated appearance of the blood–aqueous mixture. The level of IOP at any time represents a balance between the rate of formation of aqueous humor and the amount of resistance to its flow out of the anterior chamber. In almost every case of glaucoma, increased IOP is due to an abnormality in outflow from the anterior chamber, rather than to above-normal rates of aqueous humor formation. The nontrabecular aqueous route occurs through uveoscleral outflow via the supraciliary and suprachoroidal spaces and out along nerves and vessels coursing through the sclera. This route may be as important as the TM exit.
In open-angle glaucoma, the aqueous humor has unimpeded access to the TM in the angle of the anterior chamber, but there is abnormally high resistance to the fluid flow through the TM (uveal, corneoscleral, and juxtacanalicular—the last being the site of primary outflow resistance), into Schlemm’s canal, and then into the scleral venous plexus. The peripheral iris does not interfere with the access of aqueous humor to the draining angle structures.
Primary open-angle glaucoma (POAG) is the most common form of glaucoma. The underlying abnormality in the trabecular angle tissue causing
abnormal resistance to fluid flow is not known. The disease is not secondary to another eye disease or condition. POAG is a silent, surreptitious process. Usually there are no symptoms. Gradual loss of peripheral vision occurs. Loss of central vision is usually the last to occur. Only actual measurement of the IOP, inspection of the optic nerve head, and visual field testing can detect POAG in its early stages.
Secondary open-angle glaucoma occurs as a result of or in association with another eye disease or condition such as uveitis or trauma, resulting in secondary blockage or damage to the canals and collector channels.
In angle-closure glaucoma, the peripheral iris tissue covers the TM, preventing access of the aqueous humor to the TM. This type of glaucoma is often intermittent, with acute symptoms that are reversible when the peripheral iris is moved away from draining angle structures. In pure angle-closure glaucoma, the TM and Schlemm’s canal angle tissue have inherently normal resistance to fluid flow. The IOP is elevated only when the peripheral iris covers the TM, preventing egress of the aqueous.
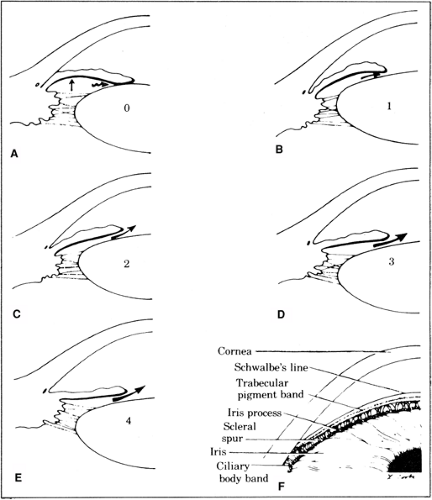
In primary angle-closure glaucoma, relative pupillary block is the mechanism of angle closure. This means that there is relative resistance to fluid flow of aqueous humor between the posterior iris surface and lens due to an abnormally close approximation at the pupil. This tends to occur in eyes with small anterior segments or short axial length. Relative pupillary block increases the pressure of aqueous in the posterior chamber, forcing the peripheral iris forward over the TM (Fig. 10.1). The state of relative pupillary block depends greatly on pupillary size and rigidity of the peripheral iris. For example, relative pupillary block may be increased and angle-closure glaucoma produced by putting a patient in a dark room or by using dilating medications that move the pupil into a mid-dilated state. Drug-induced miosis may produce a very small pupil, blocking posterior chamber aqueous passage and thus pushing the iris forward to close the angle. Most eyes subject to possible angle-closure glaucoma can be recognized by the shallowness of their axial anterior chamber depth.
Secondary angle-closure glaucoma occurs as a result of or in association with another eye disease or condition, such as a swollen cataract or neovascularization pushing or pulling the iris over the TM.
III. Methods of Examination
Flashlight. After examining pupillary light reactions, the physician should direct the flashlight to the temporal side of each eye, perpendicular to the corneal limbus, and note the shadow produced by the nasal peripheral iris against the cornea. In eyes with shallow anterior chambers that might be subject to angle-closure glaucoma, the relatively forward position of the iris will cause the nasal side to be in shadow. This flashlight examination should be performed in all patients before routine pupillary dilation. In eyes with shallow anterior chambers, the pupil should not be dilated until IOP is checked and gonioscopy is performed.
Slitlamp examination
The axial and peripheral anterior chamber depth may be measured and expressed in terms of corneal thickness. Direct a narrow slit beam onto the cornea at 60° just anterior to the limbus (Van Herick method). If the distance between the posterior corneal surface and the anterior iris surface is less than one-fourth the corneal thickness, the chamber is shallow. Anterior chamber depths less than three corneal thicknesses axially are also suspect, and gonioscopy should be performed to assess angle narrowing.
Other diagnostic signs during slitlamp examination may be noted—for example, the presence of inflammatory cell deposits (keratic precipitates [KPs]) on the corneal epithelium, anterior chamber cells and flare, Krukenberg pigmented spindle on corneal endothelium, dandrufflike dusting on the lens capsule, iris heterochromia and transillumination (by placing the vertically
narrowed beam coaxially in the pupil to create a red reflex back through the pupil), and abnormal iris vessels.
Measurement of IOP may be taken by Goldmann slitlamp or handheld applanation tonometry, other electronic or pneumotonometry, finger tension (estimate), Schiötz tonometry, or air-puff noncontact tonometry (see Chapter 1). Mean normal IOP is 16± mm Hg, although some eyes may sustain damage with IOP in the teens and others have no damage with IOP in the 30s. An IOP greater than 22 mm Hg should be considered suspicious, and the patient should be followed for ocular hypertension. Schiötz readings are falsely low in
high myopes and in thyroidopathy due to low scleral rigidity. Considerable diurnal variation of IOP occurs normally (2 to 6 mm Hg), with greater variation in IOP in patients with glaucoma. Therefore, inspection of the optic disk and neural rim is just as important as the actual measurement of the IOP.
Ophthalmoscopy of the optic nerve cup. Atrophy of connective tissue associated with the hyaloid artery during embryogenesis results in a depression of the internal (vitreous) surface of the optic disk termed the cup.
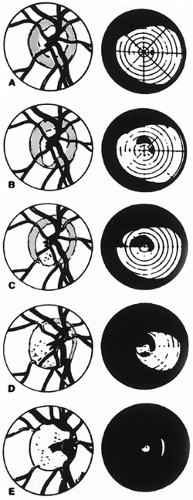
The normal physiologic disk cup varies considerably. Large physiologic cups are usually round in shape, unlike the vertical elongation that occurs in glaucoma. The amount and the contour of disk tissue present in the rim of the optic disk between the end of the cup and the edge of the disk proper are important (Fig. 10.2). Not until the cup extends toward the edge of the disk does frank glaucomatous field loss occur. It is important to recognize that many glaucomatous and normal patients have a circular halo around the optic disk in which the retinal pigment epithelium and choroidal pigment is deficient, so the physician is actually viewing the sclera underneath. The end of this peripapillary halo should not be misinterpreted as the edge of the disk in assessing the disk rim tissue. Statistically, patients with large, round physiologic cups with a cup-to-disk ratio exceeding 0.6 are more at risk of developing glaucoma, and they should be followed carefully. Round cups with intact disk rim tissue, however, are not necessarily abnormal in the absence of other changes.
The glaucomatous disk (nerve head) may be recognized by certain changes in contour of the optic nerve cup. Cupping appears to be the result of faulty autoregulation of blood flow to the optic disk in the face of IOP. Early signs of glaucomatous optic neuropathy include generalized or focal enlargement of the cup (vertical elongation or rim notching), asymmetry of cupping between the two eyes, superficial splinter hemorrhages, loss of nerve fiber layer (NFL), neuroretinal rim translucency, and nasalization of vessels.
Parallax should be used in monocular (direct ophthalmoscope) examination of the optic disk to assess the contour of the disk tissue. Stereo viewing through a dilated pupil with a fundus contact lens, a +78 or +90 diopter (D) handheld lens, or Hruby lens at the slitlamp is critical. With glaucomatous damage to the nerve, actual loss of nerve tissue and its vascular and glial supporting tissue occurs. Such atrophy results in both contour (cupping) and color (pallor) changes in disk appearance. The optic disk rim is made up of ganglion cell nerve fibers and is best evaluated by viewing the fundus with a green light (red-free). The nerve fiber bundles appear as radiating striations toward the disk and may be best documented with high-contrast black and white photos. Their loss may be diffuse or focal. Decreased visibility or white-out areas of the NFL at the rim and entering the retina are detectable in 90% of glaucomatous nerves before or during early visual field loss. In elderly people, however, nuclear sclerotic changes (early cataracts) often impart a rosy color to the disk and may be confusing. In primary optic atrophy, not due to glaucoma, change in pallor of the disk occurs with no change in contour.
In glaucoma, the cup usually enlarges vertically. The increased cupping commonly progresses first toward the inferior pole of the disk and then enlarges superiorly, but there is considerable variation. Very rarely, the optic cup may extend straight temporally first rather than vertically. In such cases, macular fibers may be affected early in the course of the disease, with resulting loss of central vision. Cupping close to or at the inferior pole of the disk will, of course, result in superior field loss; cupping close to the superior pole of the disk will result in inferior field loss. Occasionally, glaucomatous damage to the optic disk produces a shallower background bowing of disk tissue rather than excavation. The latter is called saucerization. Temporal pallor is rarely seen in glaucoma and, if noted, should raise the suspicion of an intracranial compressive lesion, arteritic ischemia or old trauma.
Asymmetry in the appearance of the right and left optic disk cups may be an early sign of glaucoma, even though each is within normal limits.
Enlargement in the size of the cup occurs before visual field loss results. Inspection of the appearance of the optic disk cup is an important part of glaucoma screening procedures. During long-term follow-up, the size and shape of the cup are noted in addition to the IOP and visual field. If enlargement of the cup occurs during follow-up, then, regardless of the absolute level of IOP, that pressure level is too high and additional glaucoma therapy is initiated. It is useful to record the appearance of the cup size and shape on a diagram (Fig. 10.2).
Visual fields
Techniques include confrontation (usually bedside examination) and various forms of automated static and kinetic perimetry (see Chapter 1, Section II.F. and Chapter 13, Figs 13.3,13.4,13.5). Glaucoma patients are followed with visual field examinations every 6 to 12 months as a routine; the latter time period is reasonable if the optic nerves are healthy, if no known field defect is present, and if the pressure is well controlled.
If visual field loss progression occurs while the patient is being followed, then, regardless of the level of IOP, the pressure is too high and glaucoma therapy should be adjusted. Similar considerations apply to progression of optic disk cupping. Except in myopes or in glaucoma patients with episodes of extremely high pressure elevation, visual field changes should correspond with optic disk cupping. For example, superior field loss does not occur unless the disk shows increased cupping to the inferior pole.
Follow-up field examination should be done with the pupil at the same size as in baseline examinations, so that a similar condition of retinal test object illumination exists for the follow-up fields added. Miotic glaucoma therapy may need to be reversed by dilation for field examinations with 2.5% phenylephrine or 1% tropicamide. Should the patient develop lens opacities, continued examination with the smaller test objects may produce artifactual field defects. The size of the test object should be graded to the visual acuity.
Glaucoma field defects characteristically respect the horizontal meridian (unlike chiasmal lesions, which respect the vertical) (Fig 10.2). This is because glaucoma characteristically produces a nerve fiber bundle defect—an arcuate defect or Bjerrum scotoma, or a variant of these, such as a nasal step. The temporal nerve fibers in the retina sweep either superiorly or inferiorly around the macula and do not cross the horizontal raphe. Because it would be purely chance that exactly symmetric nerve fibers in the superior and inferior fields would be similarly affected, glaucoma defects characteristically show some discontinuity at the horizontal meridian, such as a nasal step. The papillomacular fibers are usually relatively resistant to chronic pressure effects until late in the disease, and visual acuity changes do not occur early. After central vision is lost from glaucoma, typically all that is left is a temporal island of vision. Automated perimetry or Goldmann fields may be the first to detect early defects. Patterns of glaucomatous field loss include:
Paracentral scotoma—an island of relative or absolute loss within 10 degrees of fixation.
Arcuate scotoma—arc-shaped loss 10 degrees to 20 degrees above or below fixation (nerve fiber bundle damage).
Nasal step—relative depression of one horizontal hemifield compared to the other (damage to superior or inferior nerve fibers outside paracentral area).
Temporal wedge or step—a wedge-shaped defect from blind spot toward the periphery (damage to nerve fibers serving retina above or below optic nerve head blind spot).
Loss of all but small central and temporal islands of vision.
Gonioscopy. The angle is viewed by indirect slitlamp gonioscopy with a Goldmann two- to three-mirror lens using a viscous contact gel, or a Zeiss four-mirror lens with an Unger handle and no gel. Direct gonioscopy is done with the patient recumbent with use of a Koeppe-type dome lens and handheld microscope (see Chapter 1). The angle is assessed for shallowness and possible susceptibility to angle-closure glaucoma, as well as for other abnormalities such as pigment, synechiae, exfoliation, new blood vessels, inflammatory deposits, and evidence of old injury such as angle recession. Generally, if the scleral spur can be seen through the entire circumference and the iris is not excessively convex, the eye is not likely to be susceptible to angle closure and the pupil can be safely dilated. One commonly used angle rating system adapted from Schaeffer is depicted in Fig. 10.1. The Spaeth system expands this to include description of the peripheral iris contour, insertion of the iris root, and the effects of indentation gonioscopy on the angle configuration. It should be noted that narrow-angle eyes can look distinctly different at different examinations, perhaps reflecting different rates of aqueous production and differing relative pupillary block. Repeat examination in such narrow-angle eyes is usually indicated. The Zeiss gonioscopic lens is useful for rapidly viewing the angle, although it readily causes indentation of the eye and artificial deepening of the anterior chamber. The latter is deliberately utilized to differentiate appositional from synechial angle closure in the Spaeth system.
Optic nerve head and NFL imaging. The most common method of imaging the optic nerve is by conventional stereo photography. This is a useful means by which to document optic nerve head appearance and to perform longitudinal comparison to look for onset or progression of optic nerve cupping. Newer methods for imaging the nerve head and NFL include optical coherence tomography (OCT, NFL), scanning laser polarimetry (NFL), and confocal laser scanning ophthalmoscopy (three-dimensional imaging of optic nerve head and NFL using tomography) (see Chapter 1). NFL imaging takes advantage of the fact that the loss of retinal ganglion cells, and hence their axons, will result in a thinning of the NFL in the peripapillary region. Because the density of nerve fibers is less in the peripapillary region than at the optic nerve head itself, NFL imaging is likely to pick up earlier changes in thickness. The Nerve Fiber Analyzer (I and II) and the Gdx (Laser Diagnostic Technologies) combine polarimetry with scanning laser ophthalmoscopy to quantitate the thickness of the NFL. It is hoped that the use and development of NFL imaging will allow earlier detection of damage and progression before functional changes have occurred. These methods should be considered as adjunctive to visual field testing, however, and will likely not replace the visual field as a method for evaluating and diagnosing glaucoma. In the end, the visual field is the only means by which the physician can truly determine what the patient sees.
IV. Principles of Therapy
In all cases of glaucoma it is essential to establish whether the glaucoma is open or closed angle. This is accomplished by placing a gonioscopic contact lens on the eye and actually viewing the angle structures.
In the therapy of open-angle glaucoma, the physician usually first treats the condition medically to lower the IOP. This pressure may be lowered by increasing
the facility of aqueous outflow from the anterior chamber through the angle tissues, or by decreasing the rate of aqueous humor formation by the ciliary body, or both. Laser trabeculoplasty (LTP) is usually used alone or in conjunction with medical therapy to control IOP, nerve cupping, or progressive visual loss. Studies have shown that LTP is as effective as primary medical therapy or can be used to minimize medical treatments. Surgery is used when all other methods have failed.
Angle-closure glaucoma may initially be treated medically, but it is primarily a surgical (laser) disease, requiring peripheral iridotomy (placing a hole through the peripheral iris) to relieve pupillary block permanently. Posterior chamber aqueous pressure is thus relieved by aqueous flowing through this extra opening, and the peripheral iris falls away from the meshwork.
V. Medical Treatments and Side Effects
Studies indicate that most ocular hypotensive drugs may achieve maximal effect with less frequent administration and lower concentrations if nasolacrimal occlusion is applied (finger pressure) for 3 minutes during and after drug instillation. This may also result in fewer side effects. (See Appendix A for listings of drugs, dosages, and commercial names.)
Beta-adrenergic blockers (timolol, betaxolol, carteolol, levobunolol, metipranolol)
Mechanism of action. Timolol, levobunolol, carteolol, and metipranolol are nonselective beta1– (cardiac) and beta2– (smooth muscle, pulmonary) receptor blocking agents. Betaxolol has 100 times more affinity for beta1– than beta2-receptors.
Physiologic effects. The nonselective drugs decrease IOP by blockade of beta2-receptors in the ciliary processes, resulting in decreased aqueous production. The mechanism for betaxolol is unknown because there are so few beta1-receptors in the eye, but there may be “spill over” to bind beta2-receptors as well. There is no effect on facility of outflow. The drug molecule timolol (and probably betaxolol and levobunolol) releases from the beta-receptor site as early as 3 hours after topical administration, yet clinical effect may last up to 2 weeks. This prolonged effect may result from re-release of beta-blocker from depots in the iris pigment epithelial melanin. Carteolol, unlike the other beta-blockers, has intrinsic sympathomimetic activity, possibly resulting in fewer side effects. It also lacks timolol’s tendency to increase serum cholesterol and decrease high-density lipoproteins, a factor to consider in cardiovascular patients.
Indications are primary and secondary open-angle glaucomas, including inflammatory glaucomas, acute and chronic primary and secondary angle-closure glaucomas, ocular hypertension, and childhood glaucomas.
Precautions and contraindications include known drug allergy. These drugs should be used with caution or not at all, depending on severity of disease, in patients with asthma, emphysema, chronic obstructive pulmonary disease, bronchitis, heart block, congestive heart failure, cardiovascular disease, or cardiomyopathy. Although betaxolol is the blocker of choice in patients at risk for pulmonary reaction because of its greater beta1 (cardiac) selectivity, the drug may induce bronchospasm in some patients.
Available preparations. Timolol (Timoptic, Betimol), 0.25% to 0.50%; betaxolol (Betoptic-S) and levobunolol (Betagan), 0.25% to 0.50%; metipranolol (OptiPranolol), 0.3%; carteolol (Ocupress), 1% eye drops. Once-a-day dosing with drops or a gel formulation of timolol is also available as Timoptic XE 0.25% or 0.50% and Istalol 0.50%.
Recommended dosage is qd or q12h topically. All beta-blockers may be used with significant additive effect in combination with miotic agents, alpha2-agonists, prostaglandin analogs, or carbonic anhydrase inhibitors (CAIs).
Side effects
Bradycardia, cardiac arrest, acute asthma, and pulmonary edema have all been reported in susceptible individuals and result from systemic absorption of topical drug. Lacrimal canalicular compression should be practiced by patients at any risk, and the drug used with caution or not at all in those patients with moderate to severe cardiac or pulmonary disease.
Full adult dosage should be avoided in children because apnea may result; 0.25% qd to bid with canalicular compression is the advisable dosage.
Nursing mothers will excrete the drugs in breast milk; beta-blocker treatment of the mother should be considered carefully if she is breast-feeding.
Other side effects are lethargy, depression, impotence, hallucinations, and gastrointestinal (GI) symptoms.
Ocular effects include allergy, punctate keratitis, and diplopia. Corneal anesthesia may result from the membrane-stabilizing effects of timolol but is less with the other beta-blockers.
Alpha2-adrenergic agonists (apraclonidine and brimonidine).
The mechanism of action and physiologic effects are unclear but appear to be alpha2-receptor stimulation that results in decreased aqueous humor formation and increased uveoscleral outflow. Brimonidine may also have a neuroprotective effect on the optic nerve.
Indications are to control increases in IOP after anterior segment laser surgery (U.S. Food and Drug Administration [FDA] approved), acute short-term pressure spikes, and in chronic primary or secondary glaucomas.
Contraindications include known allergy to the drug and cardiac disease with untreated arteriovenous block or bradycardia.
Available preparations. Apraclonidine (Iopidine) is available as a 0.5% and 1% solution, and brimonidine (Alphagan) is available as a 0.2% solution. Newer preparations of brimonidine, Alphagan-P, are available in lower concentrations, 0.1% and 0.15%, and have been shown to have comparable efficacy with decreased allergic side effects.
Usual dosage. One drop 1 hour before laser surgery and one drop immediately after the procedure or just one drop immediately postlaser appears equally effective and superior to any other glaucoma drug. This dose decreases the incidence of postlaser pressure spikes of 10 mm Hg or more to less than 2% and lasts 12 hours. Chronic glaucoma treatment is one drop of 0.5% apraclonidine or one drop of brimonidine bid to tid. There is a 30% allergic response to the 0.50% apraclonidine and approximately 10% to 15% allergy rate for brimonidine. A new preparation of brimonidine, Alphagan-P, utilizes a different preservative, and has a lower allergy rate. Apraclonidine is associated with tachyphylaxis within 3 months in up to 48% of patients and therefore is useful for more short-term therapy. Beta-adrenergic blockers are the usual concomitant drugs, but prostaglandin analogs, miotics, epinephrine, and CAIs may be added as well for additive effect.
Side effects include possible transient upper lid retraction, conjunctival blanching, mydriasis, burning or itching sensation, and subconjunctival hemorrhage. Systemically, there may be GI reaction and cardiovascular effect, such as bradycardia, vasovagal attack, palpitations, or orthostatic hypotension. Central nervous system disturbances include somnolence, insomnia, irritability, and decreased libido, all of which are transient. Brimonidine should be avoided in children younger than 5 years, due to the risk of central nervous system depression.
Prostaglandin analogs (latanoprost, bimatoprost, travoprost, and unoprostone)
Mechanism of action. Lowering of IOP by increasing uveoscleral outflow through a prostaglandin F2 α-mediated mechanism.
Indications. First-line or additive therapy for lowering of high IOP.
Preparation and dosage. Latanoprost (Xalatan) 0.005%, bimatoprost (Lumigan) 0.03%, and travoprost (Travatan) 0.004% are each given once daily, usually at bedtime. Unoprostone (Rescula) 0.15% is given twice daily. Latanoprost is temperature sensitive and needs to be refrigerated prior to and after opening.
Side effects include increased iris pigmentation, darkening of the eyelid skin, increased thickness and number of eyelashes, ocular irritation (redness, itching, etc.), uveitis, cystoid macular edema, and probable reactivation of herpes simplex virus.
Carbonic anhydrase inhibitors (CAIs). Acetazolamide and methazolamide are oral agents. Acetazolamide is also available as an intravenous (i.v.) agent. Topical CAIs are dorzolamide and brinzolamide.
Mechanism of action. CAIs inhibit the enzyme carbonic anhydrase.
Physiologic effects. The ciliary body enzyme, carbonic anhydrase, is related to the process of aqueous humor formation, most likely via active secretion of bicarbonate. CAIs decrease the rate of aqueous humor formation.
Indications. CAIs are additive therapy in the management of various acute glaucomas as well as in the chronic management of primary and secondary open-angle and angle-closure glaucomas not adequately controlled by topical medication.
Contraindications. Because of the metabolic and possible respiratory acidosis effects, patients with significant respiratory disease should be given oral CAIs cautiously and in lower dosages. Patients with a history of calcium phosphate kidney stone formation should be given the oral medication cautiously and only after consultation with their primary care provider. Known allergy is a contraindication. Patients with allergies to other sulfonamides should be given these agents with caution.
Available preparations include acetazolamide (Diamox, generic) 125 mg and 250 mg tablets, 500 mg sequels, 500 mg per 5 mL i.v.; methazolamide tablets (Neptazane, GlaucTabs, MZM, generic) 25 mg and 50 mg tablets; dorzolamide (Trusopt) 2% drops; and brinzolamide (Azopt) 1% drops.
Recommended dosage. Established dosages for near-maximum effect are acetazolamide tablets 250 mg q6h; methazolamide tablets 50 to 100 mg bid to tid; acetazolamide sustained-release capsules 500 mg q12h. Because acetazolamide is excreted unchanged by the kidneys, patients with renal disease such as diabetic nephropathy should be started on lower than standard dosages. Methazolamide may be used more safely in this situation. Dorzolamide 2% drops and brinzolamide 1% tid decrease IOP by about 20%.
Side effects. Unfortunately, 40% to 50% of glaucoma patients are unable to tolerate systemic CAIs long term because of various disabling side effects. A symptom complex of malaise, fatigue, depression, anorexia, and weight loss is the most frequent side effect. Loss of libido, especially in young males, may also occur. These symptoms show some correlation with the degree of systemic metabolic acidosis on therapy. They may have a gradual, insidious onset over several months. Often neither the patient nor the physician relates these symptoms to the systemic CAI therapy. Frequently, patients erroneously undergo extensive medical evaluations searching for occult malignancies.
Simultaneous CAI and chlorothiazide systemic hypertensive therapy may produce frank hypokalemia, and the patient should have potassium supplementation. In the absence of this concomitant chlorothiazide therapy, changes in serum potassium tend to be small and there is no symptomatic benefit from potassium supplementation.
GI side effects occurring with oral CAI therapy tend to behave as local irritative phenomena, sometimes responding to administering the CAI with food, switching to a sustained-release preparation, or simultaneous mild alkali therapy.
Malaise symptoms occur in some patients. Decreasing the dosage will sometimes improve tolerance. In particular, using one 500-mg acetazolamide capsule a day (which has an effect for more than 18 hours) is very useful. In many of these patients this dosage will result in an undertreatment of their glaucoma, but in others, near-maximum effects will be maintained.
Kidney stones developing during oral CAI therapy are believed to be a result of calcium precipitation secondary to a decrease of citrate or magnesium excretion or both in the urine. The former is believed to be a direct consequence of the drugs making normally acid urine alkaline, which, with reduced citrate, induces calcium carbonate stone formation. There is a far lower incidence of kidney stone formation with methazolamide than with acetazolamide. Methazolamide has minimal action on citrate concentration or on the kidney. Management of kidney stone patients involves use of methazolamide in as low a dosage as the severity of the glaucoma permits, restriction of dietary calcium, and possibly concomitant use of chlorothiazide diuretics to alter the calcium–magnesium ratio in the urine. Electrolyte imbalance should be watched for in patients taking diuretics. Nephrologic consultation and measurement of urinary pH, calcium, and citrate should be obtained if stone formation is suspected.
Blood dyscrasias are rare. Thrombocytopenia, agranulocytosis, and aplastic anemia may occur as idiosyncratic reactions. Periodic blood tests would not be expected to anticipate these reactions and are not routinely performed. A history of a mouth or body sore that does not heal may be a clue to the occurrence of a blood dyscrasia.
Myopia occurs rarely as an idiosyncratic acute reversible phenomenon. It is believed to be due to choroidal effusions, which cause forward rotation of the lens iris diaphragm and result in shallowing of the anterior chamber.
Miotics
Pilocarpine
Mechanism of action. Pilocarpine is a direct-acting parasympathomimetic (muscarinic) cholinergic drug.
Physiologic effects. The drug is used in chronic open-angle glaucoma to increase the facility of aqueous outflow. The mechanism of action is probably exclusively mechanical, via ciliary muscle contraction and pull on the scleral spur and TM. It is used in acute angle-closure glaucoma to move the iris away from the angle. Miosis is a side effect and is of no therapeutic benefit.
Indications are chronic open-angle glaucoma, acute angle-closure glaucoma, chronic synechial angle-closure glaucoma (following peripheral iridectomy), and following cyclodialysis surgery.
Contraindications are inflammatory glaucoma, malignant glaucoma, or known allergy.
Available preparations are pilocarpine 0.5% to 8% eye drops (Isopto Carpine, Pilocar, Piloptic), and 4% gel (Pilopine-HS gel).
Recommended dosage
Eye drops. Except in very darkly pigmented irides, maximum effect is probably obtained with a 4% solution. In milder open-angle glaucoma, therapy is usually initiated with a 1% concentration. Duration of effect is 4 to 6 hours. It is usually prescribed for use every 6 hours.
The gel can be used alone at bedtime or as an adjunct to daytime medication.
Combination. Pilocarpine can be used in conjunction with other glaucoma medications and, in most instances, confers additional pressure-lowering effects.
Side effects
Ocular
Contact allergy is fairly rare.
Contraction of the ciliary muscle results in accommodation and ensuing fluctuating myopia. In younger patients, this is usually a disabling visual side effect that prevents use of pilocarpine. Most patients above the age of 50 years do not develop such pilocarpine-induced myopia, presumably because of an inelasticity of their lens that is also responsible for their presbyopia.
Pupillary miosis is a definite side effect of pilocarpine, which again exerts its antiglaucoma effect via ciliary muscle traction on the angle structures. This miosis results in diminished night vision and often some contraction in peripheral visual field. If the patient has early axial lens opacities, this miosis may result in diminished visual acuity. On the other hand, the miosis may result in a pinhole effect and an actual improvement in visual acuity.
Shallowing of the anterior chamber may occur with higher doses of pilocarpine by forward movement of the lens–iris diaphragm subsequent to ciliary muscle contraction and relaxation of zonular tension. This shallowing may result in an increase in relative pupillary block, and it may convert an open-angle glaucoma with narrow angles into partial angle-closure glaucoma. This is true for all the standard miotic glaucoma therapies (carbachol, echothiophate iodide). In susceptible individuals, it seems to be dose related. There may be varying amounts of anterior chamber shallowing on miotic therapy. Similarly, in angle-closure glaucoma, lower concentrations of pilocarpine are used initially to minimize this axial shallowing and possible increase in relative pupillary block.
Systemic side effects. Occasional patients are particularly sensitive and may develop sweating and GI overactivity with usual dosages. Sweating, salivation, nausea, tremor, headache, brow pain, bradycardia, and hypotension have sometimes been observed as results of too vigorous treatment of angle-closure glaucoma with pilocarpine.
Carbachol
Mechanism of action. A cholinergic similar to pilocarpine.
Physiologic effects. Similar to pilocarpine.
Indications. Carbachol eye drops are longer acting than pilocarpine, thus having a greater stabilizing effect on diurnal pressure and myopia fluctuation. It may also be used in patients allergic to pilocarpine; otherwise, the indications are similar to pilocarpine. An intracameral preparation for intraoperative use induces miosis and inhibits postoperative pressure increase.
Contraindications. Similar to pilocarpine.
Available preparations are carbachol (Isopto Carbachol) 1.5%, and 3% eye drops and 0.01% for intraocular use.
Recommended dosage. Carbachol 3% is approximately equivalent to pilocarpine 4%, and 1.5% carbachol is roughly equivalent to 2% pilocarpine. The effect is reported to last up to 8 hours. Dosage tid (compared to qid with pilocarpine) may be a distinct advantage in certain patients.
Side effects. Similar to pilocarpine.
Anticholinesterase agents (echothiophate iodide).
Mechanism of action. Indirect-acting parasympathomimetic activity by virtue of binding to the enzyme, acetylcholinesterase, allows endogenous acetylcholine to accumulate.
Physiologic effects. Ciliary muscle and iris sphincter muscle contraction occur similar to and possibly more marked than that occurring with other miotics (e.g., pilocarpine and carbachol). Miosis is a side effect of no therapeutic benefit.