Over the past 20 years, development of minimally invasive therapies has led to the use of extracorporeal shock wave lithotripsy (ESWL) to treat salivary stones. The two main energy sources are piezoelectric and electromagnetic extracorporeal lithotripsy. Both have the aim of fragmenting the stones. ESWL is considered the treatment of choice for all parotid calculi and submandibular perihilar or intraparenchymal stones of less than 7 mm. Continuous ultrasonographic monitoring during the procedure reduces the number of untoward effects. The main limitations are the need for multiple sessions and residual stone fragments inside the duct system.
Sialolithiasis accounts for approximately 50% of major salivary gland disease. It is the most common cause of salivary obstruction and its estimated prevalence in the general population is 1.2%. More frequently, and mainly unilaterally, it affects the submandibular gland (80%–90%), with most of the stones located in the distal third of the duct or at the glandular hilum, whereas intraparenchymal sites are infrequent. Only 5% to 10% of salivary stones involve the parotid gland. Sublingual and minor salivary glands are involvement is unusual.
Ultrasonography (US) has an accuracy of 99% for stones with a diameter of more than 1.5 mm in experienced hands. It can detect stones, whether or not they are radiopaque or nonradiopaque, and evaluate their size and relationship with the surrounding tissues. The opportunity of distinguishing parenchymal and ductal locations by means of US makes it feasible to plan the best therapeutic option for each patient. Moreover, US examination together with color Doppler monitoring provides useful information about the structural features of the affected gland; it detects the possible concomitance of inflammation and can differentiate vascular and ductal structures. It is an operator-dependent procedure, however, which may lead to difficulties in identifying the distal portion of Wharton’s duct inside the floor of the mouth and may be responsible for undetected stones; in this case, the use of endoral radiographs and standard dental radiographs is diagnostically helpful.
The traditional therapeutic approach to stones is surgical duct dissection in the case of salivary stones located in the distal and middle portion of the ductal system and sialadenectomy in the case of proximal, hilar, and intraparenchymal stones.
Over the past 20 years, new minimally invasive gland-preserving techniques have been introduced in the management of sialolithiasis, including shock wave lithotripsy, sialoendoscopy, interventional radiology, and endoscopic video-assisted transoral and transcervical stone retrieval.
Shock wave lithotripsy fragments stones so that they can be flushed out by physiologic saliva flowing out the duct. The shock waves may be produced by extracorporeal (electromagnetic or piezoelectric) sources ( Fig. 1 ) or intracorporeal (electrohydraulic, pneumatic, or laser endoscopic) sources. The former are performed under US control, which allows stone identification and targeted administration of the shock wave with real-time visualization of the fragmentation process, avoiding any iatrogenic lesions of the surrounding tissue; the latter mainly uses a laser beam brought to the stone by means of an endoscope and fiberoptics.
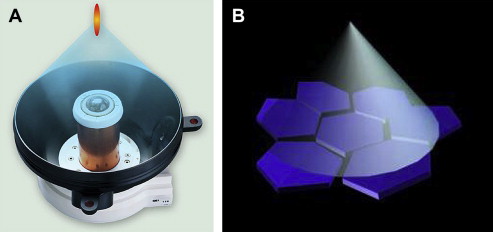
The most frequently used extracorporeal shock wave lithotripsy (ESWL) energy source is electromagnetic as it is minimally invasive and can be used on an outpatient basis without anesthesia. It was introduced in the 1980s for treatment of renal calculi and gallstones. Electromagnetic and piezoelectric sources exploit the compressive and expansive waves generated by the difference in impedance at the stone-water interface and cause stone cavitation. After encouraging results with multiple animal and in vitro experiments, the first successful ESWL for human sialolithiasis was performed by Iro and colleagues in 1989 using a device designed for renal lithotripsy. Since then, dedicated instruments have been designed and the use of ESWL has become increasingly widespread ( Tables 1 and 2 ).
| Author | Year | Site | Number | Complete Stone Clearance (%) |
|---|---|---|---|---|
| Wehrmann et al | 1994 | P | 29 | |
| SM | 44 | |||
| All | 73 | 38 (52) | ||
| Kater et al | 1994 | P | 29 | 14 (48) |
| SM | 75 | 26 (35) | ||
| All | 104 | 40 (38) | ||
| Ottaviani et al | 1996 | P | 16 | 9 (56) |
| SM | 36 | 15 (42) | ||
| All | 52 | 24 (46) | ||
| Ottaviani et al | 1997 | P | 24 | 14 (58) |
| SM | 56 | 23 (41) | ||
| All | 80 | 37 (46) | ||
| Escudier et al | 2003 | P | 32 | 13 (40) |
| SM | 84 | 27 (32) | ||
| All | 122 | 40 (33) | ||
| Capaccio et al | 2004 | P | 88 | 61 (69) |
| SM | 234 | 84 (36) | ||
| All | 322 | 145 (45) | ||
| McGurk et al | 2005 | P | 88 | 42 (48) |
| SM | 130 | 42 (32) | ||
| All | 218 | 84 (38) | ||
| Schmitz et al | 2008 | P | 59 | 18 (39) |
| SM | 126 | 33 (26) | ||
| All | 167 | 51 (30) |
| Author | Year | Site | Number | Complete Stone Clearance (%) |
|---|---|---|---|---|
| Iro et al | 1992 | P | 16 | 9 (56) a ; 13 (81) b |
| SM | 35 | 13 (37) a ; 14 (40) b | ||
| All | 51 | 22 (43) a ; 27 (53) b | ||
| Aïdan et al | 1996 | P | 3 | 1 (33) |
| SM | 12 | 4 (33) | ||
| All | 15 | 5 (33) | ||
| Iro et al | 1998 | P | 76 | 38 (50) |
| Külkens et al | 2003 | P | 42 | 26 (62) |
| Zenk et al | 2004 | SM | 197 | 58 (29) |
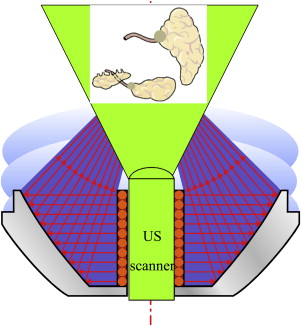
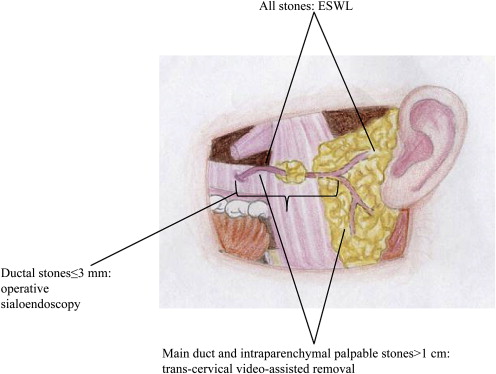
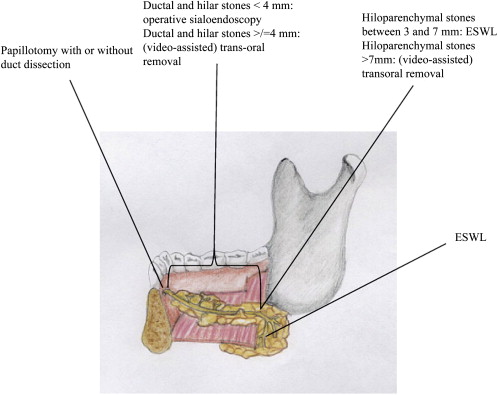
US is used to focus the shock waves on the stone ( Fig. 2 ). All of the stones that can be identified ultrasonographically and have a diameter of at least 2.4 mm are potentially amenable to treatment. The minimal size of the electromagnetic focus is 2.4 mm. In the case of proximal locations or mobile intraductal stones, however, other therapeutic procedures should be preferred, such as dilatation/dissection of the proximal duct tract and retrieval by means of sialoendoscopy or interventional radiology techniques ( Figs. 3 and 4 ). The contraindications for ESWL are complete distal duct stenosis, pregnancy, and the presence of a cardiac pacemaker. Relative contraindications include acute sialadenitis or other acute inflammatory processes of the head and neck; treatment should be postponed in these cases.
With regard to the effectiveness of electromagnetic ESWL of salivary stones, it is difficult to compare the published results directly because of criteria differences used to define outcomes: definition of complete or partial success (≤2 and >2 mm, respectively) or symptom status after lithotripsy. On the basis of the published findings, the success rate is higher in the case of parotid than in the case of submandibular stones: complete stone clearance has been reported in 39% to 69% of parotid stones but only 26% to 42% in submandibular stones (see Table 1 ) treated electromagnetically, and, respectively, 33% to 81% and 29% to –40%, of those treated piezoelectrically (see Table 2 ).
ESWL is safe, and only minor and self-limiting untoward effects have generally been reported, including pain over the treated area, glandular swelling, ductal bleeding, and cutaneous petechiae ( Table 3 ).
| Untoward Effects | Author | Year | Technique | Total Treated | Number (%) |
|---|---|---|---|---|---|
| Pain | Iro et al | 1992 | P | 51 | 51 (100) |
| Wehrmann et al | 1994 | E | 56 | 56 (100) | |
| Ottaviani et al | 1996 | E | 52 | 8 (15) | |
| Yoshizaki et al | 1996 | P | 18 | 17 (94) | |
| Iro et al | 1998 | P | 76 | 53 (70) | |
| Capaccio et al | 2004 | E | 322 | 254 (79) | |
| Swelling | Iro et al | 1992 | P | 51 | 1 (3) |
| Ottaviani et al | 1996 | E | 52 | 5 (10) | |
| Capaccio et al | 2004 | E | 322 | 113 (35) | |
| Zenk et al | 2004 | P | 197 | 4 (2) | |
| Ductal bleeding | Wehrmann et al | 1994 | E | 56 | 4 (71) |
| Ottaviani et al | 1996 | E | 52 | 9 (17) | |
| Iro et al | 1998 | P | 76 | 30 (40) | |
| Escudier et al | 2003 | E | 122 | 49 (40) | |
| Capaccio et al | 2004 | E | 322 | 126 (39) | |
| Zenk et al | 2004 | P | 197 | 108 (55) | |
| Cutaneous petechiae | Iro et al | 1992 | P | 51 | 7 (14) |
| Wehrmann et al | 1994 | E | 56 | 11 (20) | |
| Ottaviani et al | 1996 | E | 52 | 3 (6) | |
| Yoshizaki et al | 1996 | P | 18 | 4 (22) | |
| Iro et al | 1998 | P | 76 | 30 (40) | |
| Capaccio et al | 2004 | E | 322 | 74 (23) | |
| Zenk et al | 2004 | P | 197 | 108 (55) | |
| Acute sialadenitis | Escudier et al | 2003 | E | 122 | 7 (6) |
| Zenk et al | 2004 | P | 197 | 4 (2) | |
| Schmitz et al | 2008 | E | 167 | 5 (3) | |
| Temporary hearing | Kater et al | 1994 | E | 104 | 2 (2) |
| impairment | Iro et al | 1998 | P | 76 | 2 (3) |
| Temporary tinnitus | Kater et al | 1994 | E | 104 | 2 (2) |
| Capaccio et al | 2004 | E | 322 | 2 (1) | |
| Schmitz et al | 2008 | E | 167 | 1 (1) | |
| Tooth filling loss | Schmitz et al | 2008 | E | 167 | 2 (1) |
Personal experience
Population and Setting
Between December 1993 and December 2002, 322 consecutive patients (group A) with single or multiple symptomatic submandibular (234) or parotid (88) salivary stones were enrolled at the ear, nose, and throat department of University of Milan and underwent a complete cycle of extracorporeal lithotripsy ESWL. The exclusion criteria were distal stones amenable to surgical duct dilatation and dissection or mobile intraductal stones that could be removed by means of a Dormia basket. Univariate and multivariate statistical analysis of this cohort showed that a favorable treatment result was significantly associated with parotid duct location and diameter of the stone (<7 mm). Based on the results of the previous study, between January 2004 and December 2008 a further 93 patients with parotid (48) or submandibular stones (45) with diameters of 3 to 7 mm were selectively recruited and treated with ESWL (group B). The demographic and clinical data of the two groups are compared in Table 4 .
| Group A | Group B | ||||
|---|---|---|---|---|---|
| First level: demographic and clinical data | Number: 322 | Number: 93 | |||
| Males (%): 172 (53.4) | Males (%): 43 (46.2) | ||||
| Mean age ± SD: 6.6 ± 0.9 | Mean age ±SD: 5.1 ± 0.4 | ||||
| Submandibular (%): 234 (72.7) | Submandibular (%): 45 (48.4) | ||||
| Intraductal (%): 112 (47.9) | Intraductal (%): 19 (42.2) | ||||
| Hiloparenchymal (%): 122 (52.1) | Hiloparenchymal (%): 26 (57.8) | ||||
| Parotid (%): 88 (27.3) | Parotid (%): 48 (51.6) | ||||
| Intraductal: 58 (65.9) | Intraductal: 27 (56.2) | ||||
| Hiloparenchymal: 30 (34.1) | Hiloparenchymal: 21 (43.8) | ||||
| Second level: treatment | Mean duration ±SD: 30 minutes ± 2.3 | Mean duration ±SD: 31 min ± 2.7 | |||
| Mean number of shock waves ± SD: 1779 ± 3.4 | Mean number of shock waves ± SD: 1829 ± 2.9 | ||||
| Mean number of treatments ± SD: 6 ± 0.4 | Mean number of treatments ± SD: 6 ± 0.8 | ||||
| Third level: outcomes | Submandibular | Submandibular | |||
| D (%) | HP (%) | D (%) | HP (%) | ||
| Complete stone clearance | 52 (64.4) | 32 (26.2) | 12 (63.1) | 10 (38.5) | |
| Residual fragments ≤2 mm | 30 (26.8) | 34 (27.9) | 4 (21.1) | 6 (23.0) | |
| Residual fragments >2 mm | 30 (26.8) | 56 (45.9) | 3 (15.8) | 10 (38.5) | |
| Total | 112 | 122 | 19 | 26 | |
| Parotid | Parotid | ||||
| D (%) | HP (%) | D (%) | HP (%) | ||
| Complete stone clearance | 41 (70.7) | 20 (66.7) | 19 (70.4) | 14 (66.7) | |
| Residual fragments ≤2 mm | 15 (25.9) | 9 (30) | 7 (25.9) | 4 (19.0) | |
| Residual fragments >2 mm | 2 (3.4) | 1 (3.3) | 1 (3.7) | 3 (14.3) | |
| Total | 58 | 30 | 27 | 21 | |
| Fourth level: untoward effects | Local pain (%): 256 (79.5) | Local pain (%): 75 (80.6) | |||
| Glandular swelling (%): 113 (35.2) | Glandular swelling (%): 30 (32.2) | ||||
| Ductal hemorrhage (%): 124 (38.6) | Ductal hemorrhage (%): 32 (34.4) | ||||
| Cutaneous petechiae (%): 73 (22.7) | Cutaneous petechiae (%): 22 (23.6) | ||||
| Tinnitus (%): 2 (0.6) | Tinnitus (%): 0 (0.0) | ||||
| Fifth level: other required treatments | Recurrence (%): 4 (1.2) | Recurrence (%): 2 (2.1) | |||
| Papillotomy procedure (%): 26 (8.1) | Papillotomy procedure (%): 9 (9.7) | ||||
| Sialadenectomy (%): 10 (3.1) | Sialadenectomy (%): 1 (1.1) | ||||
| — | Sialoendoscopy (%): 9 (9.7) | ||||
| — | Transoral removal (%): 8 (8.6) | ||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


