Purpose
To report the effect of nepafenac (0.1%) eye drops on intraocular pressure in eyes with cataract.
Design
Prospective randomized clinical trial.
Methods
Three hundred and twenty-seven patients with bilateral cataracts in an institutional setting were included. All patients had a baseline intraocular pressure (IOP) ≤21 mm Hg without a history of intraocular surgery in the past 3 months. One eye of each individual was randomized to the treatment group, with the other eye acting as a control. Nepafenac (0.1%) eye drops were instilled 3 times a day in the eye that received treatment. Intraocular pressure (IOP) with Goldmann applanation tonometer (GAT) was measured at baseline and at 4 and 8 weeks. Proportion of eyes with an IOP elevation of >4 mm Hg was the main outcome measure.
Results
The mean age of the participants was 45.7 ± 4.4 years. Participants included 192 female and 135 male patients. The mean IOP at baseline in the treated and control eyes was, respectively, 13.8 ± 2.5 mm Hg and 13.4 ± 3.0 mm Hg, which reduced to 12.0 ± 2.0 mm Hg and 12.1 ± 1.5 mm Hg, respectively, at the end of 8 weeks. This reduction in IOP in both groups was significant ( P < .01). The difference between the IOP in the treated and control eyes at 8 weeks was not statistically significant ( P = .34). One eye in the treated group and 2 eyes in the control group had an IOP elevation of >4 mm Hg.
Conclusion
Nepafenac eye drops do not increase the IOP. They can possibly be used as an alternative to steroid medications where steroid responsiveness is a concern.
Nepafenac 0.1% (Nevanac; Alcon Labs, Fort Worth, Texas, USA) is an ocular nonsteroidal anti-inflammatory drug (NSAID) with a prodrug structure. Intraocular hydrolases convert nepafenac to the more active metabolite amfenac. These hydrolases are present in ocular tissues such as the cornea, iris, ciliary body, retina, and choroid, with their highest concentrations being in the retina and choroid. Nepafenac has excellent penetration of the cornea and scleral tissues and rapid bioactivation by the iris, ciliary body, retina, and choroid.
Topical nepafenac has been used previously to treat cystoid macular edema in steroid-responsive patients without its causing a rise in the intraocular pressure (IOP). The nepafenac product information insert says that it can cause increase in IOP in 5%-10% of patients. There is very little published literature on the effect of topical nepafenac eye drops on IOP in normal eyes. The purpose of our study is to report its effect on the IOP in otherwise normal eyes with a working hypothesis that there is no increase in IOP following use of nepafenac eye drops.
Methods
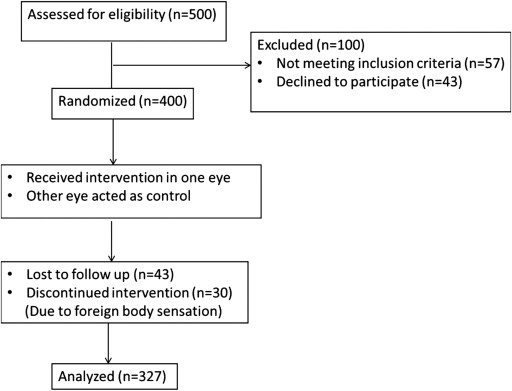
This was a prospective, open-label, single-center, single-masked randomized controlled study, and an informed consent was obtained from all subjects. The study protocol was prospectively approved by the institutional review board and health research ethics committee (Dr TV Patel Eye Institute Ethics Committee). The trial was registered with http://www.clinical trials.gov (identifier: NCT01995890 , registration location: Vadodara, Gujarat, India). The rise in IOP with nepafenac eye drops is reported in up to 10 in 100 patients. Keeping a confidence interval of 95% and an alpha error of 5%, a sample size of 276 in each group was thought to be adequate to have 80% power to demonstrate this effect. The primary outcome measure was proportion of eyes with IOP elevation more than 4 mm Hg from baseline. The minimum level of significance was set at P < .05. From December 3, 2012 to February 28, 2013, 2 authors (P.D. and K.S.) initially enrolled 500 consecutive bilateral cataract patients with best-corrected visual acuity better than 20/80 in both eyes, who were otherwise normal for the study, from the outpatient department of a tertiary care hospital. We excluded 100 patients who either did not fit the inclusion criteria or declined to take part in the study. Randomization and allocation concealment was done by one of the authors (B.R.). We used a random number table to randomize 1 eye of each patient to the treatment group while the other eye acted as control. The allocation concealment was done with a sealed envelope technique. The envelope was received and opened (by P.D.) just after the first examination of the patient and the treatment eye was noted, with the same being explained to the patient. If the envelope seal was broken, the patient was excluded from the study.
Inclusion criteria were best-corrected visual acuity better than 20/80 in both eyes, IOP (measured with Goldmann applanation tonometer [GAT], mean of 4 daytime readings) ≤21 mm Hg in both eyes, open angles on 4-mirror gonioscopy without indentation, and a normal optic disc on stereoscopic examination and photographs. All treated eyes received nepafenac 0.1% eye drops 3 times a day (1 drop at 8 AM, 12 PM [noon], and 4 PM). The adverse effects of the medication were clearly stated to all the participants, who were given the option to withdraw at any point in the study. Thirty patients stopped medications owing to foreign body sensation. Forty-three patients did not complete the full 8-week follow-up. These patients were excluded from the study. Three hundred and twenty-seven patients finally completed the study ( Figure 1 ).
The exclusion criteria were change in the systemic medication profile during the course of the study (if any), allergy to the nepafenac molecule, corneal thinning/corneal infections, any intraocular surgery in past 3 months, pregnancy or those planning to conceive, breastfeeding patients, unwillingness to participate in the trial, and concomitant use of any other ocular drug (except artificial tears). The compliance was self-reported by the patients to one of the authors (P.D.) and tested by actively asking for missed doses as well as checking the amount of medication used from the drop bottle at each follow-up before the examination. All patients were given 2 bottles of nepafenac 0.1% (3 mL) drops at each visit. One bottle was expected to last for about 15-20 days. Patients not finishing at least 1 bottle on subsequent follow-up were considered to be noncompliant and excluded from the study. Patients were sent for examination at least 30 minutes after the last instillation of the drop to avoid identification of the treatment eye by the yellow color of the nepafenac eye drops.
A complete ophthalmic examination included best-corrected visual acuity, IOP measurement with GAT, gonioscopy, indirect ophthalmoscopy, and slit-lamp biomicroscopy. All examinations were performed by one of the authors (K.S.). The examiner was masked with regard to the eye receiving the treatment. After measuring the IOP, the reading was recorded by another author (R.J.), who was present at the time of examination and was also masked. The IOP was measured on the same GAT instrument and at approximately the same time of the day. The IOP measurements were then repeated after 4 and 8 weeks.
Statistical Analysis
Descriptive and inferential statistics were performed using STATA version 12 for Windows (StataCorp LP; College Station, Texas, USA). Paired t test was used to compare the IOP changes in the treated and the control eyes. A 2-tailed t test was used to compare the IOP between the treated and the control eyes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


