Purpose
To report a series of dislocations of the donor graft into the posterior segment associated with Descemet stripping endothelial keratoplasty (DSAEK) and to identify possible risk factors for dislocation and clinical outcomes.
Design
Retrospective case series.
Methods
Cases of donor graft dislocation into the posterior segment associated with endothelial keratoplasty were identified from the clinical experience of 7 surgeons. Observations included the preoperative surgical history of each eye, preoperative and postoperative visual acuity, management of the complication, and the postoperative clinical course. No identified cases were excluded from this series.
Results
Eight posterior graft dislocations were associated with DSAEK surgery. Each eye had a history of vitrectomy. Five eyes had sutured posterior chamber intraocular lenses, 1 eye had a sulcus intraocular lens, and 2 eyes were aphakic. Each eye required repeat grafting, and in 6 of 8 eyes, pars plana vitrectomy was used to remove the dislocated graft. Final visual acuities ranged from 20/30 to no light perception.
Conclusions
Graft dislocation into the posterior segment is a rare complication of DSAEK surgery that can lead to permanent vision loss. It has occurred in eyes that have undergone previous vitrectomy and complicated intraocular lens placement or were aphakic. As is the case with a dropped lens nucleus during cataract extraction, visual acuities after a dropped DSAEK graft range from very good to no light perception. Better postoperative results seem to be associated with prompt removal of the posteriorly dislocated graft.
Descemet stripping automated endothelial keratoplasty (DSAEK) is a form of partial thickness corneal transplantation for the treatment of diseases of the corneal endothelium. This procedure involves adhering a donor button consisting of corneal stroma, Descemet membrane, and endothelium to the posterior surface of a host cornea that has been stripped of its own Descemet membrane and endothelium. DSAEK quickly has become the preferred alternative to full-thickness corneal transplantation for patients with diseases of the corneal endothelium because it offers faster visual recovery and minimal induced astigmatism.
With the increasingly widespread use of DSAEK, it has been offered to a wide variety of patients. The procedure has been completed successfully in children as well as in patients who have had multiple prior intraocular procedures, including vitrectomy, sutured posterior chamber intraocular lens placement, and glaucoma surgery. The most common complication of DSAEK is graft dislocation within the anterior chamber. In addition to this and other possible complications of DSAEK, eyes that have undergone vitrectomy also share the risk of graft dislocation into the posterior segment. Posterior segment dislocation of DSAEK grafts is rare, with only a few reported cases in the literature, one of which was reported in a series of 118 eyes that underwent DSAEK surgery. We present 8 cases of DSAEK graft dislocation into the posterior segment. The surgical management of each incident and the interval outcome of each graft and eye are reported.
Methods
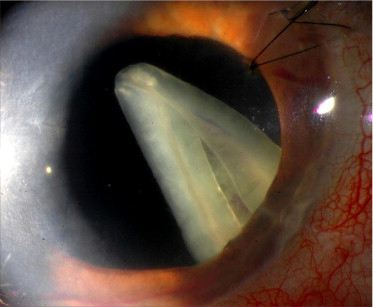
This was a retrospective, multicenter case series. Examination of the operative reports of the more than 1,300 DSAEK procedures completed at the Duke Eye Center between January 2005 and January 2011 revealed 2 intraoperative cases and 1 postoperative case ( Figure ) wherein DSAEK grafts dislocated to the posterior segment. In addition to 3 cases that were managed at the Duke Eye Center, 5 cases from the combined experience of 5 surgeons were included in this study. One of these cases was reported previously and is included in this series. One of the other included cases was referred for management by another surgeon. The average age of patients at the time of complication was 69 ± 9.7 years, with a male-to-female ratio of 1:1. Four eyes required DSAEK for a failed corneal graft, whereas 3 had pseudophakic bullous keratopathy and 1 had Fuchs dystrophy. There were no criteria for exclusion from this study.
The clinical history of each eye was reviewed to identify the following preoperative factors hypothesized to increase the risk of posterior segment dislocation of grafts: history of vitrectomy or traumatic globe injury, status of the lens, status of the iris, and prior glaucoma surgery. Preoperative and postoperative visual acuities were collected, as well as the occurrence of any postoperative complications, including cystoid macular edema, epiretinal membrane formation, and retinal detachment. The period between graft dislocation and graft retrieval was recorded for each case, as was the final surgical outcome of the cornea (repeat DSAEK surgery, penetrating keratoplasty, or both).
Results
Patient Factors
Table 1 shows the clinical features of eyes with posteriorly dislocated DSAEK grafts. All eyes had undergone vitrectomy between 2 months and several years before DSAEK surgery. Two eyes (25%) were aphakic. Four eyes (50%) had undergone prior penetrating keratoplasty. Five eyes (62.5%) had abnormal irides, ranging from traumatic aniridia to extensive anterior synechiae. All 8 eyes had undergone complicated intraocular lens placement or were aphakic before DSAEK surgery; all intraocular lenses were in the posterior chamber. Four (50%) were sutured intraocular lenses, 1 (12.5%) was a sulcus-based intraocular lens, and 1 (12.5%) was an artificial iris (Ophtec 311 Aniridia lens; Ophtec BV, Groningen, The Netherlands) also sutured into the sulcus—this eye was referred to one of the authors for management after posterior dislocation occurred elsewhere. Two eyes were aphakic at the time of this complication. All but 2 of the detachments occurred during surgery; in 2 detachments, the lenticule was observed in the vitreous at a follow-up visit.
| Case No. | Lens Status | Prior Penetrating Keratoplasty | Prior Vitrectomy | Iris Status | Presence of Glaucoma Tube | History of Traumatic Globe Injury | Visual Acuity before Descemet Stripping Automated Endothelial Keratoplasty |
|---|---|---|---|---|---|---|---|
| 1 | Sulcus IOL | No | Anterior vitrectomy | Normal | No | No | 20/100 |
| 2 | Sutured PCIOL | Yes | PPV | Iris rim remnants only | No | No | 20/400 |
| 3 | Sutured PCIOL | Yes | Anterior vitrectomy | Peripheral iris–cornea synechiae | No | No | Counting fingers at 3 feet |
| 4 | Sutured PCIOL | Yes | PPV | Surgical changes | Yes | Yes | Hand movements |
| 5 | Aphakic | No | PPV | Normal | No | No | Hand movements |
| 6 | Sutured PCIOL | No | Anterior vitrectomy | Extensive synechiae | Yes | No | 20/100 |
| 7 | Aphakic | Yes | Anterior vitrectomy | Large superior sector iridectomy | No | Yes | Counting fingers at 6 inches |
| 8 | Sutured sulcus artificial iris (Ophtec model 300) | No | Anterior vitrectomy | Traumatic aniridia with artificial iris (Ophtec model 300) | No | Yes | 20/60 –1 |
Surgical Management
Table 2 summarizes the timing and method of removal of each graft, the final outcome of each cornea, posterior segment sequelae (including macular edema and retinal detachment), and the final visual acuity of each eye as recorded at the most recent postoperative visit. In the 8 cases reported, 4 eyes (50%) were treated successfully with repeat DSAEK and the other 4 eyes (50%) underwent penetrating keratoplasty after graft removal. In 3 cases (Cases 1, 2, and 5), the misplaced graft subsequently was adhered to the host cornea and remained at least partially attached after surgery; however, all of the grafts failed and were replaced within 2 months of the first surgery. Histopathologic examination of one retrieved graft showed inflammatory cells around the tissue and a paucity of endothelial cells. In 6 of the 8 cases (75%), the graft was removed via pars plana vitrectomy; in 2 instances (25%), the corneal surgeon retrieved the graft with the irrigation-and-aspiration handpiece either at the time of complication or at the time of repeat DSAEK surgery.
| Patient No. | Method of DSAEK Graft Removal | Timing of DSAEK Graft Removal | Outcome of Host Cornea | Posterior Segment Outcomes of Recipient Eyes | Final Visual Acuity |
|---|---|---|---|---|---|
| 1 | PPV | Time of dislocation | Graft reattachment, failure, and repeat DSAEK 2 mos later | Cystoid macular edema and epiretinal membrane requiring PPV with membrane peeling | 20/40 |
| 2 | I/A handpiece | Time of dislocation | PK at POW 2 | No sequelae reported | 20/400 |
| 3 | PPV | 7 d | PK at time of PPV | No sequelae reported | 20/126 |
| 4 | PPV | 9 d | PK at POM 2 | No sequelae reported | 20/30 |
| 5 | PPV | 6 wks | PK at POW 6 | Total retinal detachment | No light perception |
| 6 | I/A handpiece | 4 wks | Repeat DSAEK | Epiretinal membrane, rhegmatogenous retinal detachment | Hand movements |
| 7 | PPV | Time of dislocation | Repeat DSAEK | No sequelae reported | 20/400 |
| 8 | PPV | 9 wks | Repeat DSAEK | No sequelae reported | 20/60 −2 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


