Surgical approaches to the craniovertebral junction (CVJ) can result in dysfunction of the upper aerodigestive tract. However, few data are available regarding the incidence of complications after such surgery. Evaluation of a CVJ lesion for treatment must establish the biology, transverse and longitudinal extent of the lesion, and the preoperative and postoperative stability of the spine. Endoscopic approaches to the CVJ, which should reduce the expected morbidity of an open transoral approach, have been described recently. This article reviews common pathologies of the CVJ and surgical approaches, and provides an evidence-based analysis of whether endoscopic approaches reduce velopharyngeal insufficiency.
Diseases of the odontoid and craniocervical junction
Anatomy
| EBM Question | Level of Evidence | Grade of Recommendation |
|---|---|---|
| Is endoscopic surgery associated with decreased velopharyngeal insufficency? | 3b | D |
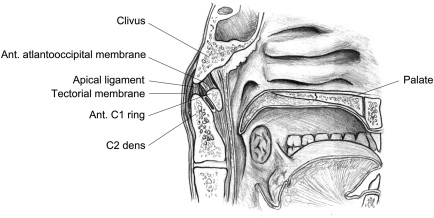
The anterior longitudinal ligament extends along the ventral vertebral surface, attaching to the anterior arch of the atlas, and forms the anterior atlanto-occipital membrane, which connects the clivus. The posterior longitudinal ligament extends cephalad along the posterior vertebral surface and forms the tectorial membrane at the foramen magnum. The posterior atlanto-occipital membrane is the anatomic equivalent of the interspinous ligament of the subaxial spine, and connects the posterior margin of the foramen magnum to the posterior arch of the atlas. The alar ligaments connect the odontoid to the occipital condyles and the lateral masses of the atlas bilaterally. The apical ligament connects the odontoid tip to the lower end of the clivus. The transverse ligament, dorsal to the odontoid process, forms a strong connection between the two lateral masses of the atlas and holds the odontoid pressed anteriorly.
The foramen magnum is formed within the occipital bone, which is composed anteriorly of the clivus and laterally of the occipital condyles. The clivus is a midline bone that joins the sphenoid bone superiorly and forms a portion of the posterior and inferior walls of the sphenoid sinus. Cranial nerve 12 emerges lateral to the clivus, at the anterior edge of the occipital condyle extracranially through the hypoglossal canal. The vertebral arteries course within the transverse process of the cervical vertebrae to the level of C1 and then project posteriorly across the posterior arch of the atlas. The vertebral arteries enter the foramen magnum laterally and join to form the basilar artery along the anterior face of the brainstem. The angle of the clivus in relation to the skull base can vary, and normally averages 134° to 137°. Angles greater than 143° are associated with the diagnosis of platybasia, a flattened skull base. Anomalies of the occiput, including condylar hypoplasia, basiocciput hypoplasia, and atlanto-occipital assimilation, are often associated with decreased skull base height and basilar invagination.
Pathology of craniocervical junction
A wide range of pathology occurs at the craniocervical junction, such as congenital malformation, trauma, malignancy, benign neoplasms, and autoimmune diseases. Tumors can arise primarily in the region of the craniocervical junction, or secondarily as hematologic, lymphatic, or metastatic deposits. Goals of care should be tailored to the tumor pathology.
Anatomic Disorders Affecting the Craniocervical Junction
In general, congenital or acquired anatomic lesions causing defects that need surgical intervention all cause their effect through basilar impression of the odontoid onto the brainstem and spinal cord. The pressure results in neurologic dysfunction experienced by the patient as early numbness and tingling in the limbs, and later as motor nerve weakness and anesthesia. Surgical intervention is necessary to relieve pressure and preserve neuronal function.
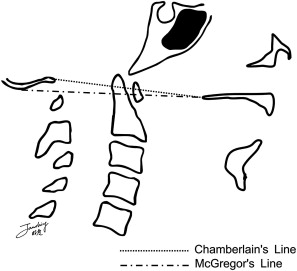
A range of malformations can affect the craniocervical junction, such as odontoid malformations, primary basilar invagination syndromes, secondary acquired basilar impression syndromes due to softening of the bone, and several anomalies of the skull base. Whereas primary lesions can cause basilar invagination, secondary lesions are considered to cause basilar impression. McGregor’s line is drawn from the posterior hard palate to the base of the occiput. Chamberlain’s line is drawn from the posterior hard palate to the anterior lip of the foramen magnum. In about 50% of individuals the tip of the odontoid is at or below this line. Basilar invagination or impression is considered present when the tip of the dens is more than 4.5 mm above McGregor’s line and 6 mm above Chamberlain’s line ( Fig. 2 ).
Several congenital lesions are associated with pathology of the craniocervical junction, such as Klippel-Feil syndrome, Down syndrome, osteogenesis imperfecta, achondroplasia, and mucopolysaccharide diseases. Rare disorders can also cause basilar impression including cloverleaf skull, Hajdu-Cheney syndrome, bathrocephaly (an unusual protuberance of the occipital bone), basilar invagination with unusual facial and extremity abnormalities, Sjögren-Larsson syndrome, and pyknodysostosis ( Fig. 3 ).

Acquired cranial disorders can result in bone softening with resultant basilar invagination, and can occur in diseases such as osteomalacia, osteogenesis imperfecta, cretinism, parathyroid disorder, and rickets. The weight of the head over time may result in inferior displacement of the skull and apparent odontoid elevation.
Odontoid malformation can result from a few diseases such as Aarskog syndrome, Morquio syndrome (mucopolysaccharide type IVB), Dyggve-Melchior-Clausen syndrome, spondylometaphyseal dysplasia, congenital spondyloepiphyseal dysplasia, and cartilage-hair hypoplasia.
Trauma
Trauma of the craniocervical junction requiring surgical management is rare. Odontoid fractures account for 9% to 15% of cervical spine fractures, and are the most common cervical spine fracture in individuals older than 70 years. Such fractures result from overextension or hyperflexion of the neck. Three types of odontoid fracture can occur depending on the location: at the tip (Type I), between the inferior aspect of the anterior C1 ring and lacking extension into the superior articular facets (Type II), and at the junction with the body of C2 with extension into the superior articular facets of C2 (Type III). In general, Types I and III are considered stable and can be treated with collar immobilization. If a Type III fracture is combined with a C2-C3 fracture dislocation, it may be very unstable. Type II factures are generally less stable, and immobilization with a halo vest still results in a 26% to 80% nonunion rate. Stabilization may be achieved through a posterior approach, or at times through an anterior approach with screw fixation.
Infectious Disease
Infections can afflict the spine and require surgery for culture and/or debridement. Infections typically occur through direct extension or hematologic seeding and cause prevertebral, intraspinal, and epidural abscess. Retropharyngeal abscess, a well-known otolaryngic infection, rarely causes an intraspinal infection. Of the 14 cases reported in the literature due to retropharyngeal origin, all were due to Staphylococcus aureus .
Spinal epidural abscess can be associated with intravenous drug use, a history of diabetes mellitus or human immunodeficiency virus (HIV) infection, multiple medical illnesses, trauma, prior spine surgery, morbid obesity, prior spinal nerve block, and end-stage renal disease. Other sources include hematogenous spread associated with dental extractions or endocarditis. The traditionally defined classic triad of clinical manifestations is localized pain, progressive neurologic deficit, and fever, but has been reported to occur concurrently in as low as 40% of patients. The most common organisms cultured are S aureus or Streptococcus , while tuberculosis is a rare but known entity. Infections can progress to a spinal epidural abscess, which can be associated with a rapid decline and high morbidity. Clinical findings include developing neurologic deficits with decreased motor strength, and an elevated white blood cell count and erythrocyte sedimentation rate. Imaging with computed tomography (CT) and enhanced magnetic resonance imaging can accurately diagnose these entities, but culture and surgical decompression may be required. Surgical management consists of decompression with drainage of pus, removal of granulation tissue, and irrigation. In the cervical region, lesions are addressed aggressively because of the relatively small space within the spinal cord.
Autoimmune: Rheumatoid Pannus
Rheumatoid arthritis incites an inflammatory condition known as a rheumatoid pannus that requires surgical decompression. The developing pannus causes ligamentous laxity, bone erosion, and brainstem compression due to either direct pressure from the pannus, or a static or dynamic subluxation of the cervical spine. These patients also typically have advanced rheumatoid conditions with many peripheral joints severally afflicted. Access via the transoral route may be impeded if the temporal mandibular joint is involved, causing trismus of the oral cavity (inability to open jaw more than 4 cm), and creating the need for a mandibulotomy. Preliminary reports suggest infliximab, a monoclonal antibody against tumor necrosis factor α and a successful a medical therapy, may reduce the inflammatory pannus size and avoid surgery.
Neoplasms
A range of hematologic, lymphatic, and solid malignancies have been found in the craniocervical junction, which can arise primarily or seed it secondarily from a distant source. Surgical intervention may be necessary to obtain an adequate biopsy, for extirpation, or for decompression. A CT-guided fine-needle aspiration can be considered for soft-tissue lesions in this region. However, lesions occurring within the bone cannot be accessed by the needle and require a surgical approach. When in doubt, it is reasonable to attempt a fine-needle aspiration first.
Hematologic spread of tumor can seed the craniocervical junction with lymphoma, myeloma, or metastatic tumors, which can produce lytic lesions of the bone or infiltrate the marrow. Radiographic evaluation of the osseous skeleton can be performed to identify the easiest site for biopsy.
Solid tumors may arise from the overlying epithelium, such as nasopharyngeal carcinoma, salivary gland tissue such as adenocarcinoma or adenoid cystic carcinoma, mesenchymal tissue such hemangiomas and sarcomas, or cartilaginous/osseous tissue of the spine. A range of tumors of the bone can affect the cervical spine, including chordoma, chondroma, chondrosarcoma, osteosarcoma, and fibrous dysplasia. Other lesions can involve the CVJ including eosinophilic granuloma, aneurysmal bone cyst, schwannoma, neurenteric cyst, meningioma, and neurofibromas. In one series a single vertebra was affected in 75% of benign and 40% of malignant lesions, with more than one vertebra affected in 25% of benign and 60% of malignant lesions.
Nasopharyngeal Carcinoma
The most common tumor of the nasopharynx is nasopharyngeal squamous cell carcinoma (NPC). NPC is a rare tumor with an incidence of 0.2 to 1 per 100,000 in North America and Europe, and 25 per 100,000 in South-East Asia. NPC is classified into World Health Organization Type I (keratinizing), Type II (differentiated), and Type III (undifferentiated). In endemic areas Type III is associated with Epstein-Barr virus, infection, a genetic predisposition, and dietary intake of preserved food. The tumor starts in the epithelial lining of the nasopharynx and can spread laterally via the Eustachian tube, intracranially via cranial foramen, or posteriorly into the CVJ. Erosion into the spine is delayed until the late stages due to the dense fibrous tissue of the pharyngobasilar fascia. Given the need to manage the lymphatic spread in the neck and the excellent response rates, these lesions are typically managed with combined cisplatin-based chemotherapy and radiation regimens. The 5-year overall survival rate is 90% and 84% for stage I and IIA disease, respectively. Stage IIB has an increased rate for distant disease. However, recurrences isolated to the nasopharynx may be appropriate for surgery in selected cases. Long-term effects of radiation may result in osteoradionecrosis that may require surgical debridement.
Osseous Lesions: Chordoma
Chordomas, the most common tumor of the mobile spine, are rare tumors that arise from the remnants of the notochord, a structure that induces formation of the vertebral column. While chordomas do not usually metastasize, they are locally aggressive, causing local bone erosion and neurologic dysfunction. In the largest current series over a 25-year period, 5-year and 10-year survival rates are reported at 55% and 36%, respectively.
En bloc resection of chordoma is considered the key to long-term survival in patients with chordoma to prevent tumor seeding and dissemination. Survival rates in patients with chordoma of the thoracolumbar spine and appendicular musculoskeletal system demonstrate improved survival when an en bloc resection with wide margins is achieved. However, to date only 6 cases have been published describing an en bloc resection of the C2 vertebra, only one of which included the C1 vertebra. Due to the intricate anatomic relations of the vertebral arteries, basilar artery, brainstem, and important cervical rootlets of the upper extremities, and limited exposure in this region, few cases are amenable to an en bloc resection. Thus resection of the craniocervical junction is often performed as a piecemeal resection, with high recurrence rates ( Fig. 4 ).
Osseous Lesions: Chondrosarcoma
Chondrosarcomas are a heterogeneous group of malignant tumors of cartilaginous origin, comprising rare and usually slow-growing malignancies of cartilage. In the skull base a chondrosarcoma may arise from remnant cartilage elements after ossification. It can rarely metastasize. The most common cause of death is due to local invasion of the base of skull. The diagnosis and treatment is similar to chordoma based on its origin, location, and growth. Both lesions are similar on radiographic imaging, and histopathology and may require immune-histochemical staining to distinguish them. In the skull base the most common tumor site is in the petroclival junction, but it is also found to occur in the jugular foramen, clivus, sphenoid bone, and retro-orbital region. The primary treatment paradigm is surgical resection when possible, followed by postoperative radiation. In a meta-analysis of the American College of Surgeons National Cancer database of 400 patients with chondrosarcoma of the head and neck, there was a 70% 10-year survival rate.
Pathology of craniocervical junction
A wide range of pathology occurs at the craniocervical junction, such as congenital malformation, trauma, malignancy, benign neoplasms, and autoimmune diseases. Tumors can arise primarily in the region of the craniocervical junction, or secondarily as hematologic, lymphatic, or metastatic deposits. Goals of care should be tailored to the tumor pathology.
Anatomic Disorders Affecting the Craniocervical Junction
In general, congenital or acquired anatomic lesions causing defects that need surgical intervention all cause their effect through basilar impression of the odontoid onto the brainstem and spinal cord. The pressure results in neurologic dysfunction experienced by the patient as early numbness and tingling in the limbs, and later as motor nerve weakness and anesthesia. Surgical intervention is necessary to relieve pressure and preserve neuronal function.
A range of malformations can affect the craniocervical junction, such as odontoid malformations, primary basilar invagination syndromes, secondary acquired basilar impression syndromes due to softening of the bone, and several anomalies of the skull base. Whereas primary lesions can cause basilar invagination, secondary lesions are considered to cause basilar impression. McGregor’s line is drawn from the posterior hard palate to the base of the occiput. Chamberlain’s line is drawn from the posterior hard palate to the anterior lip of the foramen magnum. In about 50% of individuals the tip of the odontoid is at or below this line. Basilar invagination or impression is considered present when the tip of the dens is more than 4.5 mm above McGregor’s line and 6 mm above Chamberlain’s line ( Fig. 2 ).
Several congenital lesions are associated with pathology of the craniocervical junction, such as Klippel-Feil syndrome, Down syndrome, osteogenesis imperfecta, achondroplasia, and mucopolysaccharide diseases. Rare disorders can also cause basilar impression including cloverleaf skull, Hajdu-Cheney syndrome, bathrocephaly (an unusual protuberance of the occipital bone), basilar invagination with unusual facial and extremity abnormalities, Sjögren-Larsson syndrome, and pyknodysostosis ( Fig. 3 ).
Acquired cranial disorders can result in bone softening with resultant basilar invagination, and can occur in diseases such as osteomalacia, osteogenesis imperfecta, cretinism, parathyroid disorder, and rickets. The weight of the head over time may result in inferior displacement of the skull and apparent odontoid elevation.
Odontoid malformation can result from a few diseases such as Aarskog syndrome, Morquio syndrome (mucopolysaccharide type IVB), Dyggve-Melchior-Clausen syndrome, spondylometaphyseal dysplasia, congenital spondyloepiphyseal dysplasia, and cartilage-hair hypoplasia.
Trauma
Trauma of the craniocervical junction requiring surgical management is rare. Odontoid fractures account for 9% to 15% of cervical spine fractures, and are the most common cervical spine fracture in individuals older than 70 years. Such fractures result from overextension or hyperflexion of the neck. Three types of odontoid fracture can occur depending on the location: at the tip (Type I), between the inferior aspect of the anterior C1 ring and lacking extension into the superior articular facets (Type II), and at the junction with the body of C2 with extension into the superior articular facets of C2 (Type III). In general, Types I and III are considered stable and can be treated with collar immobilization. If a Type III fracture is combined with a C2-C3 fracture dislocation, it may be very unstable. Type II factures are generally less stable, and immobilization with a halo vest still results in a 26% to 80% nonunion rate. Stabilization may be achieved through a posterior approach, or at times through an anterior approach with screw fixation.
Infectious Disease
Infections can afflict the spine and require surgery for culture and/or debridement. Infections typically occur through direct extension or hematologic seeding and cause prevertebral, intraspinal, and epidural abscess. Retropharyngeal abscess, a well-known otolaryngic infection, rarely causes an intraspinal infection. Of the 14 cases reported in the literature due to retropharyngeal origin, all were due to Staphylococcus aureus .
Spinal epidural abscess can be associated with intravenous drug use, a history of diabetes mellitus or human immunodeficiency virus (HIV) infection, multiple medical illnesses, trauma, prior spine surgery, morbid obesity, prior spinal nerve block, and end-stage renal disease. Other sources include hematogenous spread associated with dental extractions or endocarditis. The traditionally defined classic triad of clinical manifestations is localized pain, progressive neurologic deficit, and fever, but has been reported to occur concurrently in as low as 40% of patients. The most common organisms cultured are S aureus or Streptococcus , while tuberculosis is a rare but known entity. Infections can progress to a spinal epidural abscess, which can be associated with a rapid decline and high morbidity. Clinical findings include developing neurologic deficits with decreased motor strength, and an elevated white blood cell count and erythrocyte sedimentation rate. Imaging with computed tomography (CT) and enhanced magnetic resonance imaging can accurately diagnose these entities, but culture and surgical decompression may be required. Surgical management consists of decompression with drainage of pus, removal of granulation tissue, and irrigation. In the cervical region, lesions are addressed aggressively because of the relatively small space within the spinal cord.
Autoimmune: Rheumatoid Pannus
Rheumatoid arthritis incites an inflammatory condition known as a rheumatoid pannus that requires surgical decompression. The developing pannus causes ligamentous laxity, bone erosion, and brainstem compression due to either direct pressure from the pannus, or a static or dynamic subluxation of the cervical spine. These patients also typically have advanced rheumatoid conditions with many peripheral joints severally afflicted. Access via the transoral route may be impeded if the temporal mandibular joint is involved, causing trismus of the oral cavity (inability to open jaw more than 4 cm), and creating the need for a mandibulotomy. Preliminary reports suggest infliximab, a monoclonal antibody against tumor necrosis factor α and a successful a medical therapy, may reduce the inflammatory pannus size and avoid surgery.
Neoplasms
A range of hematologic, lymphatic, and solid malignancies have been found in the craniocervical junction, which can arise primarily or seed it secondarily from a distant source. Surgical intervention may be necessary to obtain an adequate biopsy, for extirpation, or for decompression. A CT-guided fine-needle aspiration can be considered for soft-tissue lesions in this region. However, lesions occurring within the bone cannot be accessed by the needle and require a surgical approach. When in doubt, it is reasonable to attempt a fine-needle aspiration first.
Hematologic spread of tumor can seed the craniocervical junction with lymphoma, myeloma, or metastatic tumors, which can produce lytic lesions of the bone or infiltrate the marrow. Radiographic evaluation of the osseous skeleton can be performed to identify the easiest site for biopsy.
Solid tumors may arise from the overlying epithelium, such as nasopharyngeal carcinoma, salivary gland tissue such as adenocarcinoma or adenoid cystic carcinoma, mesenchymal tissue such hemangiomas and sarcomas, or cartilaginous/osseous tissue of the spine. A range of tumors of the bone can affect the cervical spine, including chordoma, chondroma, chondrosarcoma, osteosarcoma, and fibrous dysplasia. Other lesions can involve the CVJ including eosinophilic granuloma, aneurysmal bone cyst, schwannoma, neurenteric cyst, meningioma, and neurofibromas. In one series a single vertebra was affected in 75% of benign and 40% of malignant lesions, with more than one vertebra affected in 25% of benign and 60% of malignant lesions.
Nasopharyngeal Carcinoma
The most common tumor of the nasopharynx is nasopharyngeal squamous cell carcinoma (NPC). NPC is a rare tumor with an incidence of 0.2 to 1 per 100,000 in North America and Europe, and 25 per 100,000 in South-East Asia. NPC is classified into World Health Organization Type I (keratinizing), Type II (differentiated), and Type III (undifferentiated). In endemic areas Type III is associated with Epstein-Barr virus, infection, a genetic predisposition, and dietary intake of preserved food. The tumor starts in the epithelial lining of the nasopharynx and can spread laterally via the Eustachian tube, intracranially via cranial foramen, or posteriorly into the CVJ. Erosion into the spine is delayed until the late stages due to the dense fibrous tissue of the pharyngobasilar fascia. Given the need to manage the lymphatic spread in the neck and the excellent response rates, these lesions are typically managed with combined cisplatin-based chemotherapy and radiation regimens. The 5-year overall survival rate is 90% and 84% for stage I and IIA disease, respectively. Stage IIB has an increased rate for distant disease. However, recurrences isolated to the nasopharynx may be appropriate for surgery in selected cases. Long-term effects of radiation may result in osteoradionecrosis that may require surgical debridement.
Osseous Lesions: Chordoma
Chordomas, the most common tumor of the mobile spine, are rare tumors that arise from the remnants of the notochord, a structure that induces formation of the vertebral column. While chordomas do not usually metastasize, they are locally aggressive, causing local bone erosion and neurologic dysfunction. In the largest current series over a 25-year period, 5-year and 10-year survival rates are reported at 55% and 36%, respectively.
En bloc resection of chordoma is considered the key to long-term survival in patients with chordoma to prevent tumor seeding and dissemination. Survival rates in patients with chordoma of the thoracolumbar spine and appendicular musculoskeletal system demonstrate improved survival when an en bloc resection with wide margins is achieved. However, to date only 6 cases have been published describing an en bloc resection of the C2 vertebra, only one of which included the C1 vertebra. Due to the intricate anatomic relations of the vertebral arteries, basilar artery, brainstem, and important cervical rootlets of the upper extremities, and limited exposure in this region, few cases are amenable to an en bloc resection. Thus resection of the craniocervical junction is often performed as a piecemeal resection, with high recurrence rates ( Fig. 4 ).




