Abstract
Purpose
To report the first known case of Descemet’s Membrane Endothelial Keratoplasty (DMEK) graft rejection following COVID19 infection.
Observation
A 60-year-old woman with a history of DMEK for Fuch’s dystrophy, presented with redness and vision loss in her operated eye 18 months after surgery. Further clinical history revealed systemic symptoms consistent with COVID19, which had started 3 weeks prior to the onset of ocular symptoms. Examination revealed graft rejection, despite patient compliance with maintenance topical corticosteroid therapy. Serological testing was positive for SARS-CoV-2 IgG. The patient responded well to intensive treatment with systemic, periocular and topical corticosteroids, and reversal of graft rejection was achieved. Two months later, there was a recurrence of graft rejection while on maintenance therapy with cyclosporin 2% and topical corticosteroids. The same intensive immunosuppressive treatment protocol was followed, and reversal of graft rejection was again achieved.
Conclusion and Importance
We believe that COVID-19 infection was a causative factor in this patient DMEK rejection. By highlighting this case, we hope to raise awareness amongst ophthalmologists of potential graft complications following COVID19 infection.
1
Introduction
The COVID-19 pandemic is a global health crisis that has seen patients presenting with clinical features ranging from asymptomatic, to severe acute respiratory syndrome and multiorgan manifestations. Various ocular manifestations of SARS-Cov-2 have been described, such as conjunctivitis, anterior uveitis, and episcleritis.
More severe ocular manifestations such as retinitis, and optic neuritis have been only documented in animal models.
We report the first known case of a Descemet’s membrane endothelial keratoplasty (DMEK) rejection following COVID19 infection.
2
Case report
A 60-year-old woman, who worked as an intensive care unit nurse, underwent DMEK in her right eye in November 2018 with a final BCVA of 20/32, and a post operative central corneal thickness of 502μm. She presented to the eye emergency department in April 2020, 18 months after DMEK surgery, with a red eye and reduced vision. She reported anosmia, fever and arthralgia three weeks prior to the onset of ocular symptoms. The patient had been compliant with her ocular treatment regimen, which consisted of once daily dexamethasone drops (DEXAFREE 1 mg/mL) and artificial tears.
On examination, the best corrected visual acuity (BCVA) was 20/80. The intraocular pressure (IOP) was 10 mmHg. Slit lamp examination revealed mild conjunctival hyperemia, multiple granulomatous keratic precipitates (KP) confined to the posterior surface of the graft, and a deep anterior chamber (AC) with 1+ cells. Fundoscopy was normal. Specular endothelial microscopy revealed a cell count of 2055 cells/mm 3 . The central corneal thickness (CCT) was raised at 593μm, and KP’s were noted on optical coherence tomography (OCT) examination of the cornea ( Fig. 1 ). The patient was diagnosed with graft rejection, and urgently treated with intravenous corticosteroids (Methylprednisolone 500mg/day for 3 days), hourly topical dexamethasone 0.1% and daily subconjunctival dexamethasone injection (4mg/mL). A PCR nasopharyngeal swab was negative for SARS-Cov-2. In addition, HSV1 and HSV2 serology were negative. We noted a significant and rapid clinical improvement on treatment. The BCVA improved to 20/40, with a clear cornea, and reversal of graft rejection. The treatment with topical corticosteroids was slowly tapered and cyclosporin 2% added twice daily. In view of the patient’s high-risk profession, and previous symptoms suggestive of COVID19, we performed a SARS-CoV-2 serology test, which returned IgG positive.
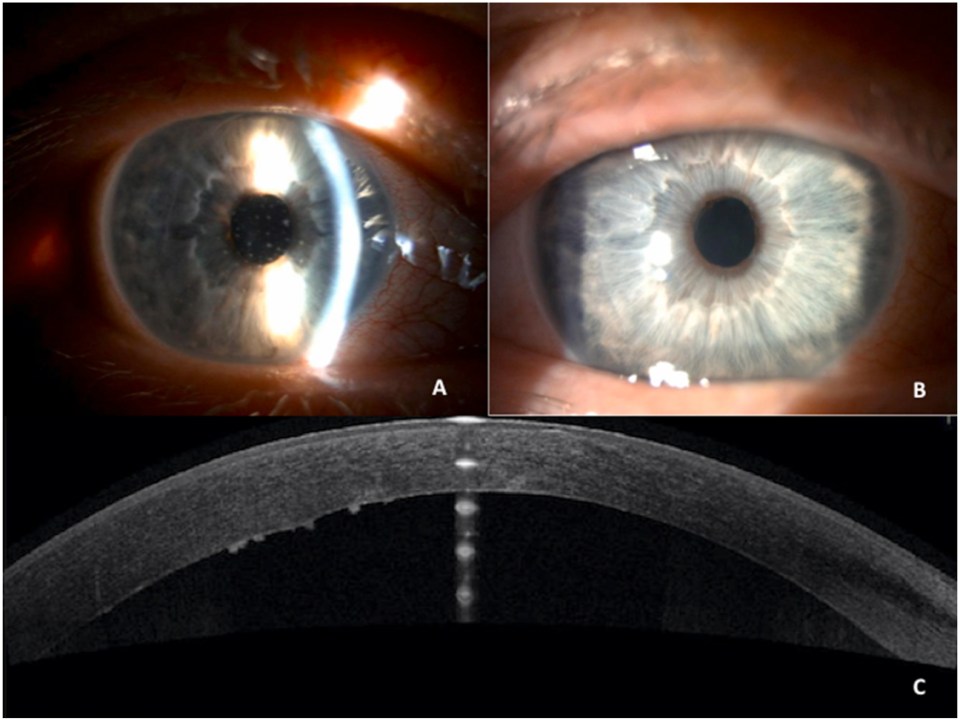
Two months later, she re-presented with a similar clinical appearance while on topical treatment with dexamethasone 0.1% 4 times daily and cyclosporin 2% twice daily. She had no systemic symptoms suggestive of COVID infection. An OCT of the cornea revealed corneal folds and increased CCT of 711μm. Specular endothelial microscopy showed a cell count of 1209 cells/mm. The same graft rejection treatment protocol was commenced, and again reversal of rejection was achieved. The final BCVA was 20/63, with a clear cornea and reduction in CCT to 495μm.
3
Discussion and conclusion
DMEK continues to increase in popularity, due to the advantages of rapid visual recovery, more predictable refractive outcomes, and increased structural integrity compared to traditional penetrating keratoplasty. The AC is an area of high immunological tolerance based on several features. There is an absence of blood and lymphatic circulation, reduced expression of MHC-encoded alloantigen’s on graft cells, existence of an immunosuppressive local microenvironment, eye-derived immunological tolerance called anterior chamber-associated immune deviation (ACAID) which is a down-regulation of delayed-type cellular immunity. The blood-ocular barrier composed of both blood aqueous and blood retinal barriers, is the only gateway in case of inflammation. Corneal grafts, in particular DMEK grafts, are rejected less frequently than any other tissue. To the best of our knowledge, this is the first reported case of DMEK rejection associated with COVID 19 infection. We suggest a causal link given the chronology of events.
DMEK graft rejection is uncommon. In the largest retrospective series of 905 cases, Hos D et al. reported a rejection rate of 1.3% during the first year. This rejection rate remains low even at extended time intervals from graft surgery. DMEK has a significantly lower risk of immunologic rejection than DSEK within the first 5 years (2,6% vs. 7,9% respectively). Vasiliauskaitè et al. showed that up to 10 years postoperatively the cumulative DMEK rejection rate increased to 4%, but was still lower than the 5-year rejection rates for DSAEK.
We acknowledge that although it is not possible to confirm a causative link between COVID and graft rejection, the timing is suggestive of causality. Indeed, this rejection occurred during the classical postoperative period described in studies (between 12 and 18 months). However, this period often coincides with discontinuation of topical corticosteroids, or a change to a weaker topical treatment, which may explain the increased rate of rejection in this timeframe. Continued topical corticosteroid use (once-daily, often fluorometholone 0,1%) is protective against rejection episodes during the second year after DMEK. In our view, the fact that this uncommon event occurred concomitantly with COVID19 infection despite the daily use of topical corticosteroid is a strong argument for a causal relationship.
The SARS-CoV2 RNA test by RT-PCR has been detected in tears and in conjunctival swab samples from infected patients, raising concerns regarding the eye both as a portal of entry, and carrier of the virus. SARS-CoV2 has been known to infect cells via angiotensin-converting enzyme 2 receptors (ACE2) for entry and transmembrane serine protease 2 (TMPRESS2) for the viral spike S protein priming. ACE2 and TMPRSS2 receptors have been identified in the ocular surface, but also in retina and choroid. The stress induced by the virus may encourage the corneal antigen-presenting cells activation and immune response. This has also been suggested in a recent case of acute endothelial rejection in penetrating keratoplasty coinciding with COVID-19 infection.
There are a number of possible explanations for the negative nasopharyngeal swab result. It may be explained by the moderate sensitivity of the test; Yicheng et al. reported a sensitivity of 71% for the RT PCR in comparison to the CT SCAN (98%). In addition however, it is known that the duration of viable virus is relatively short-lived, and SARS-CoV-2 titres in the upper respiratory tract peak in the first week of illness.
This patient was tested 3 weeks after symptoms onset, and it has been shown that sampling 10 days or more after symptoms onset greatly reduces the chance of a positive result.
We also speculate that there is immunological cross reactivity once seroconversion is achieved. DMEK rejection occurred 3 weeks after the onset of COVID19 symptoms, coinciding with the time of seroconversion. Delayed immunological responses to COVID19 have been described such as Kawasaki-like disease in children, acrosyndrome as a possible expression of immune vasculitis, or bilateral anterior uveitis after a Kawasaki-like syndrome in an adult infected. Recurrence may be associated with re-exposure to the virus in our patient’s workplace.
In conclusion, we report a case of DMEK graft rejection associated with COVID infection. We report this case to highlight the potential for graft complications following COVID19 infection.
Patient consent
Written consent to publish this case was obtained from the patient.
Funding sources
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors thank Dr Sarah Moran for her contribution to the review of the pre-publication report.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


