Purpose
To compare objective and subjective outcomes after Descemet membrane endothelial keratoplasty (DMEK) and Descemet stripping automated endothelial keratoplasty (DSAEK) in the fellow eye of the same patients.
Study Design
Single-center, retrospective case series.
Methods
Seventeen patients with bilateral Fuchs endothelial dystrophy who underwent DSAEK earlier in 1 eye, and later underwent DMEK in the contralateral eye, composed study population. A chart review was completed to obtain follow-up data for at least 6 months after each surgery. Outcome measures included best spectacle-corrected visual acuity (BSCVA) and endothelial cell density (ECD). Subjective questionnaires were used to assess patients’ satisfaction.
Results
Preoperative BSCVA (logMAR) was similar in both groups, 0.66 ± 0.4 in DMEK and 0.59 ± 0.4 in DSAEK ( P = .6). The DMEK group showed better BSCVA than the DSAEK group at the 6-month time point (0.25 ± 0.1 and 0.39 ± 0.1, for DMEK and DSAEK, respectively, P = .02). Preoperative ECD (cells/mm 2 ) was similar in both groups (2647 ± 249 and 2768 ± 404, P = .3) in DMEK and DSAEK, respectively. There was statistically significant difference found in ECD at 6 months (2227 ± 565 for DMEK and 1780 ± 433 for DSAEK, P = .049). Subjective level of average satisfaction after DMEK was 6 and after DSAEK was 4.87 ± 1.19 ( P = .002).
Conclusions
DMEK provided better visual outcome and lower endothelial cell loss than DSAEK and a higher level of patient satisfaction when assessed at 6 months after surgery. Our results comparing the 2 procedures in the same patients support the benefits of DMEK, and suggest the need for long-term studies observing this new surgical procedure.
Fuchs corneal endothelial dystrophy is a common disease requiring corneal transplantation. The pathology is localized to the Descemet membrane and endothelial layer and performing posterior lamellar corneal transplants has become the surgical treatment of choice for these patients. The treatment aims to replace diseased host endothelium with a lamellar donor graft bearing healthy endothelial cells. Various techniques of endothelial keratoplasty vary in the way to prepare donor tissue and result in disparate thickness of tissue, and vary in the way the tissue is introduced and handled inside the recipient eye.
Descemet stripping automated endothelial keratoplasty (DSAEK) uses an automated microkeratome to prepare donor disc consisting of endothelial layer, Descemet membrane, and thin layer of posterior stroma. The newer procedure, Descemet membrane endothelial keratoplasty (DMEK), involves manual preparation of donor graft consisting only of endothelium and Descemet membrane. Differences in handling of donor tissue and in ways of introducing the DSAEK and DMEK grafts into a recipient’s anterior chamber, as well as different thicknesses of these grafts, may result in different postoperative outcomes in rate of healing and endothelial cell survival.
The aim of our study is to report the objective (visual acuity and endothelial cell density) and subjective (patient satisfaction questionnaires) outcomes in a cohort of patients that underwent DSAEK in 1 eye and DMEK surgery in their other eye.
Methods
A retrospective medical chart review of patients who underwent a DSAEK in 1 eye and DMEK in the fellow eye secondary to Fuchs corneal endothelial dystrophy at Toronto Western Hospital was performed between 2012 and 2013. Only patients who had at least 6 months postoperative follow-up were included. This retrospective observational case series received Research Ethics Board approval by the University Health Network (Toronto Western Hospital, Toronto, Ontario, Canada) and was conducted in compliance with the tenets of the Declaration of Helsinki.
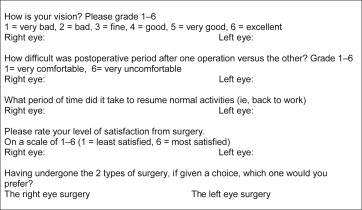
The data collected in this study included demographic characteristics, best spectacle-corrected visual acuity (BSCVA), associated operative procedures, intraoperative and postoperative complications, corneal donor characteristics, and endothelial cell density (ECD) using noncontact specular microscope (Robo, KSS 300; Konan Medical, Hyogo, Japan). Patients completed questionnaires on their last follow-up visit, grading their recovery rate, symptoms, and satisfaction with both surgeries on a scale of 1–6 ( Figure ).
Surgical Techniques
All donor tissue we used were stored in corneal storage solution (Optisol; Bausch & Lomb, Rochester, New York, USA) and received from the Eye Bank of Canada, Ontario division.
The DSAEK lenticule was prepared immediately before transplantation as previously described. Briefly, the donor disc was cut with the Moria ALTK microkeratome system equipped with a 300 mm head and associated artificial anterior chamber (AC) (Moria, Antony, France). After dissection and 8.5 mm punch with a corneal trephine, an anchoring 10/0 Prolene stitch on a long curved needle (CIF-4; Ethicon, New Jersey, USA) was placed on the donor disc at the 6-o’clock position. Then, the donor was placed on the Busin glide and inserted into the AC. The AC was filled with air for 10 minutes and then part of the air was removed and replaced with balanced salt solution (BSS).
DMEK grafts were prepared as previously described. After preparation, the 8.5 mm donor Descemet membrane was loaded into the Emerald IOL cartridge (Abbott Medical Optics, Santa Ana, California, USA) and inserted into the anterior chamber through clear corneal (2.8 mm) incision. Tapping technique together with intracameral short bursts of BSS were used to unfold and position the graft. The AC was then filled with air and 1 drop of cyclopentolate hydrochloride 1% (MINIMS Cyc 1.0; Chauvin Pharmaceuticals Ltd, UK) and of phenylephrine hydrochloride 10% (MINIMS PHNL 10; Chauvin Pharmaceuticals Ltd) were instilled to prevent pupillary block.
All patients stayed strictly supine for 2 hours and then “as much as possible” at home until the next morning. All patients were examined 2 hours after surgery and, if necessary, some of the air was released if the bubble was completely filling the AC and pupillary block was deemed to be likely. All eyes underwent pressure-patching overnight. The following day, 0.1% dexamethasone sodium phosphate and 0.3% tobramycin antibiotic (Tobradex; Alcon, Mississauga, Ontario, Canada) eye drops were administered 4 times daily for 1 month. Then, antibiotic drops were discontinued and 0.1% dexamethasone sodium phosphate (Maxidex; Alcon) eye drops were tapered down to once daily during a 3-month period.
Statistical Analysis
The data are presented as mean ± standard deviation (SD). Paired 2-tailed Student t test and the Wilcoxon rank-sum test were used to assess differences in respective parameters. The distributions of values within each data set were evaluated graphically. A P value of .05 was selected for the threshold of statistical significance. Analyses were performed using Excel (Microsoft Corp, Redmond, Washington, USA) and SAS 9.3 (SAS Institute Inc, Cary, North Carolina, USA).
Results
Thirty-four eyes of 17 patients (9 female and 8 male) aged 72.6 ± 11.3 years (range 42–87 years) were included. All patients were previously diagnosed with Fuchs endothelial dystrophy. Seven eyes that underwent DMEK and 6 eyes that had DSAEK were pseudophakic with posterior chamber intraocular lenses. Nine eyes from the DMEK group and 10 eyes from the DSAEK group underwent phacoemulsification with posterior chamber intraocular lens implantation concurrent with the keratoplasty. One eye from each group was phakic without cataract at time of keratoplasty.
There were no differences between the groups in terms of complications types and rates. Three eyes from each group showed partial dehiscence of the posterior lamellar graft and required air reinjection during the early postoperative period. Two eyes from each group had high intraocular pressure on the first postoperative day and required reopening of corneal incisions for decompression. None of the eyes had acute rejection.
Table 1 presents donor characteristics in both groups. The mean age of the donors was older and the time from death to keratoplasty was longer in the DMEK group than in the DSAEK group; both findings were statistically significant. Time from death to corneal processing and ECD, as was evaluated by the eye bank, were similar in both groups.
| DMEK (Mean ± SD) | DSAEK (Mean ± SD) | P | |
|---|---|---|---|
| Donor age (y) | 67.8 ± 4.9 | 55.3 ± 14.8 | .007 |
| Time from death to preservation (h) | 19.2 ± 5.2 | 20.5 ± 7.0 | .9 |
| Time from death to use (d) | 7.0 ± 2.1 | 4.9 ± 3.1 | .01 |
| ECD (cells/mm 2 ) | 2647 ± 249 | 2768 ± 404 | .3 |
Visual acuity before the keratoplasty, at the 3-month time point, and at the 6-month time point after the surgery, is presented in Table 2 . Mean preoperative BSCVA was similar in DMEK and DSAEK groups (0.66 ± 0.4 logMAR and 0.59 ± 0.4 logMAR, respectively [ P = .6]). Both groups showed improvement in visual outcomes with statistically significantly better BSCVA in the DMEK group than in the DSAEK group (0.25 ± 0.1 logMAR and 0.39 ± 0.1 logMAR, respectively [ P = .02]) at the 6-month time point.



