This article discusses the mechanisms of aging and future areas of exploration, and addresses strategies to achieve successful aging given the current state of medical knowledge. The authors begin at the beginning, with mitochondrial function and cell growth and decline, then continue to present aspects over which humans have control over their health: nutrition, body posture, exercise, lifestyle choices, and Traditional Eastern medicine. The discussion concludes with the role of the physician in offering patient education regarding behaviors for a healthy life.
Key points
- •
Complementary and integrative medicine (CIM) is generally described as any practice that can be used for the prevention and treatment of diseases, but which is not taught widely in medical schools, generally available in hospitals, or usually covered by health insurance.
- •
The mission of the Center for Integrative Medicine and the Henry Ford Health System West Bloomfield (HFWB) Hospital is to provide an environment in which patients resolve all health challenges and achieve optimal health.
- •
The average health status of the US population is steadily declining, while the use of increasingly higher-cost technology and pharmaceuticals in conventional medicine is not producing better health.
- •
Ultimately, success requires multiple “champions” from the medical and administrative sides, strong support from the leaders in the system, and a clear vision and strategy that embraces the importance of integrative care for our patients.
- •
The most successful systems seem to have secured significant funding, in the range or $10 million or more.
- •
It is paramount that the health system partner with many nearby community groups to address social, economic, and educational issues affecting people in the communities it serves.
Overview
The development of integrative care centers and hospitals is worth pursuing, and frankly, is no longer an option, but a requirement. Our existing paradigm of “health care” is nothing more than “sick care.” Providing a more holistic and preventive approach is challenging, but a change we must implement. The Centers for Disease Control and Prevention estimates that two-thirds to three-fourths of all medical disorders are preventable. In 2013, “sick care” spending is estimated to approach $2.7 trillion and make up approximately 18% of the gross domestic product. This is not sustainable. Since 1998 at the Henry Ford Health System (HFHS), we have been implementing wellness initiatives designed to target many health care issues, with the goal of preventing disease, improving outcomes, and reducing health care expenditures. Some of these strategies involve complementary and integrative medicine (CIM).
CIM, perhaps better known as complementary and alternative medicine (CAM), can be defined in a variety of ways. CIM is generally described as any practice that can be used for the prevention and treatment of diseases, but which is not taught widely in medical schools, generally available in hospitals, or usually covered by health insurance. There are many widely accepted therapies that fall under the guise of CIM. Many of these practices had their inception in Asia thousands of years ago, whereas others originated in Europe or America. Box 1 provides a partial list of CIM therapies.
Acupuncture
Alexander technique
Ayurveda
Biofeedback
Chiropractic
Energy healing
Feldenkrais technique
Folk remedies
Healing touch
Herbal supplements
Homeopathy
Hypnotherapy
Imagery
Magnet therapy
Massage therapy
Meditation
Megavitamin therapy
Naturopathy
Neuromuscular therapy
Prayer
Qigong
Reflexology
Reiki
Relaxation
Remote healing
Rolfing
Self-help groups
Spiritual healing by others
Tai chi
Therapeutic touch
Yoga
History
The origins of what we now consider conventional medicine started approximately 200 years ago. The roots of complementary and integrative therapies have been present since civilization began. There are references, for example, to the healing applications of aloe vera in the Bible. During the mid-twentieth century there was a rapid elimination of CIM, as it was often considered to be quackery or charlatanism and was not validated by double-blind, randomized, placebo-controlled studies. It is difficult, if not impossible, to randomize and placebo control every type of therapeutic intervention, but the lack of strong, evidence-based research does not necessarily mean that a therapy is ineffective.
Clearly many clinicians with strong science backgrounds, coupled with the increasing demand for evidence-based medicine, find the following quotes or care model heretical on some level, and perhaps feel that these methodologies were germane only in the era of leeches and prayer. The authors of this article wholeheartedly endorse the concept that was adroitly articulated by Rich Rosenfeld: “the best care is likely to emerge from a skillful blend of best evidence with caring, humility, and behavior that engenders a placebo response.” Additionally, and in many ways not too dissimilar, in 1694 Voltaire is credited with saying, “the art of medicine consists in amusing the patient while nature cures the disease.” Last, Thomas Adams (English clergyman,1618) said, “Prevention is so much better than healing because it saves the labor of being sick.” Although some might consider these comments visionary for the times, cynics will argue that there was nothing else available, so all we could do was hold the hands of our patients and pray for them. The power of the body to heal itself is grossly underused in medicine today; the best physicians understand this and find ways to facilitate this healing.
Modern trends
CIM therapies are continuing to penetrate conventional Western medical health care. In 1997, the number of CIM visits to alternative practitioners was 629 million (a growing trend), whereas there were 386 million visits to primary care physicians (a declining trend). The US Department of Health and Human Services issued a report dated May 27, 2004, regarding “Complementary and Alternative Medicine Use Among Adults: United States, 2002.” It showed that 62% of adults had used some form of CIM in the preceding 12 months. Interestingly, they included prayer (specifically for health reasons); when prayer was excluded, that number dropped to 36%. CIM was most often used for:
- •
Back pain
- •
Upper respiratory infections
- •
Neck problems
- •
Anxiety
- •
Depression
It is evident that there continues to be a significant increase in both use and acceptance of CIM therapies by Americans.
There are many reasons cited for considering CIM, including peoples’ dissatisfaction with conventional medicine, which is perceived to be authoritative, expensive, ineffective, and too intent on managing disease rather than focusing on wellness and prevention of disease. Other reasons include the following:
- •
Market forces
- •
The desire of patients to have a more active role in their medical care
- •
The impression that conventional medicine fails to satisfactorily treat chronic ailments, such as chronic headache, back pain, fibromyalgia, cancer, and tinnitus and vertigo, among many others.
Thus, there are many patients who are engaging in alternative strategies. It is becoming clear that many CIM users are not necessarily dissatisfied with conventional care, but that they are developing a more holistic approach to their health and they want more health care options. A matter of concern to health providers is that, according to a report in the Journal of the American Medical Association, 70% of CIM users do not inform their physicians about their use. This statistic is alarming, as some of the herbal and nutritional supplements can interfere with common medications, at times with potentially life-threatening effects. Nondisclosure also minimizes the ability of the conventional physician to participate in the total care of the patient.
It is becoming increasingly apparent that patients are interested in being treated by a physician who is at least open to considering CIM therapies, particularly when conventional therapies may be less effective. Currently, approximately 75% of medical schools are offering courses on alternative medicine. Physicians must learn about CIM. In the best circumstances, we should use expertise from a variety of practitioners, and collaborations between physicians and people who practice CIM should become routine. Although CIM was conceived thousands of years ago, it exists as “frontier territory.” However, we remain convinced that in certain situations, it might be and should be just what the doctor ordered.
Blending Conventional Medicine with CIM
It is important for medical practitioners to very seriously consider the integration of conventional medicine with CIM. Not only is there an increase of public interest in complementary and integrative therapies, but there is also a growing awareness of the effectiveness of CIM therapies, both on the part of consumers as well as the scientific community.
Generally speaking, chronic health problems respond well to a holistic approach based on state-of-the-art conventional medicine combined with CIM modalities to address suboptimal nutrition, emotional imbalances, structural abnormalities, blocked energy flow, and unsupportive belief systems, among other problems. There are many chronic diseases that simply do not respond well to conventional therapeutic intervention. These include such conditions as the following:
- •
Tinnitus and vertigo
- •
Chronic back pain
- •
Arthritis
- •
Headache
- •
Fibromyalgia
- •
Cancer
It is becoming increasingly clear that the best practices involve providing patients with a wide array of potential healing options. It is difficult for even the most open-minded provider to be an expert in all therapies, or be aware of everything that is available, what the research supports, and where to refer people. Providers must be honest with patients, especially if they do not know about a treatment modality. A lack of knowledge about a CIM modality does not provide a license to speak in a disparaging way about the modality.
The HFHS Center for Integrative Medicine ( Fig. 1 ) and Vita Wellness Center provide excellent examples of integration of conventional medicine and CIM. These centers were conceived as a state-of-the-art program to provide optimal care for chronic illness and to support health and wellness. They provide integrative care with a strong research-based orientation to ensure the safe and effective blending of conventional and complementary medicine. CIM practitioners address patients as a whole in mind, body, and spirit. CIM professionals attempt to mobilize and enhance the healing ability inherent in each person, and they recognize that they are in partnership with their patients; treatment is directed toward the unique goals and values of each individual. Practitioners at the Center enter treatment notes in the patients’ electronic records. We have collected data for more than 10 years on more than 5000 patients who have visited the center and received more than 35,000 treatments, including the following:
- •
Acupuncture
- •
Chiropractic
- •
Massage
- •
St. John neuromuscular therapy
- •
Feldenkrais movement reeducation
- •
Hypnotherapy.

Most patients treated at the center have failed all conventional medical options. In spite of this, our data show that pain levels in patients are reduced consistently by at least 50%, and some patients have eliminated their pain completely. Collecting data at centers is vital for identifying various alternative treatment strategies that are worthwhile.
In March 2009, HFHS opened a $370 million hospital based on the concept of health and wellness ( Figs. 2 and 3 ). A critical part of the vision began with the very basic building blocks of food for our patients and employees. Henry Ford West Bloomfield (HFWB) Hospital does not use freezers or fryers, and serves organic and local food whenever possible. Every recipe is evaluated by a team of clinicians, ensuring that the meals are as healthy as possible. Because of these efforts, our patients and guests always enjoy fresh, delicious, and nutritious food. HFWB also offers a state-of-the-art greenhouse, which offers organic produce through hydroponics. The produce is used in our kitchens, and also used to educate community members about the importance of sustainable, healthy food sources. Additionally the Demonstration Kitchen, an educational facility located within the hospital, impacts patients and guests through cooking classes aimed at improving health.
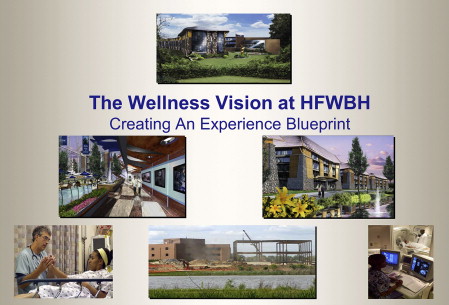
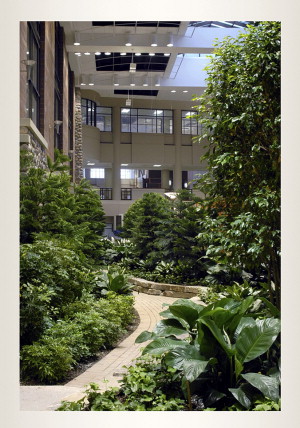
The path to wellness at HFWB Hospital continues to the Vita Wellness center. Vita offers patients integrative therapy services in addition to conventional medical treatments. We offer mind-body therapies, acupuncture, chiropractic, traditional Chinese medicine, health coaching, and use of nutraceuticals, yoga studios, massage, and more within the same building. The health system built walking paths and an outdoor basketball court on our 160-acre property with the ultimate aim of improving the health and wellness of those who choose to visit our system. This innovative hospital design was greatly influenced by the president and CEO, Gerard van Grinsven. Gerard van Grinsven is a former executive in the hospitality industry, and led for the vision for distinction and innovation. This has led to further progress; through the direction of our in-house “think tank” of experts, we are creating a center of excellence based on wellness and prevention of disease. The model is supported by the CEO of our health system and other system leaders. We are driving a model that, when fully implemented, is predicted to significantly enhance the wellness of our patients, community, and state, and when disseminated throughout the country will likely have staggering positive effects on health care expenditures.
It is becoming clear that dramatic changes in our health care system are needed. Health care costs are rising more rapidly than ever, and our country is being held hostage by these high costs. Integrative medicine is one relatively inexpensive approach that is helpful for many chronic, difficult-to- manage diseases. By incorporating the best of conventional and complementary medicine, health care professionals can work together to create an effective integrative health care system. Only in this way may we succeed at producing the best health of our population at the lowest cost.
Mission and Vision
The mission of the Center for Integrative Medicine and the HFWB Hospital is to provide an environment in which patients resolve all health challenges and achieve optimal health.
“To administer medicine to diseases which have already developed and thereby suppress bodily chaos which has already occurred is comparable to the behavior of those who begin to dig a well after they had grown thirsty, or those who would begin to cast weapons after they have engaged in battle. Would these actions not be too late?” (The Yellow Emperor’s Classic of Internal Medicine Circa 400 BC)
HFWB Hospital and the Center for Integrative Medicine are the world’s leader in pioneering unique, effective integrative care and wellness programs that propel patients to achieve optimal health and wellness. Patients are provided state-of-the-art integrative care, combining the high-technology sophistication of conventional care with world-leading, novel, and innovative holistic approaches that, together, take health and healing beyond what has previously been possible.
Cutting-edge research supports the implementation of the most proven-effective healing and wellness programs. All patients and their families have access to wellness programs that support them in taking full control of their lives to achieve optimal health. The paradigm of long-term management and maintenance of chronic illnesses gives way to the eventual resolution of chronic disease.
As the clinical population of HFHS and the Center for Integrative Medicine grows out of our successes, a higher percentage of patient visits are to support achieving optimal health through participation in wellness programs. These programs are disseminated throughout health care to produce unprecedented cost savings and improvement of the health of the global population.
Health status in America
The cost of health care is increasing rapidly, which is having an adverse effect on our national economy, corporations, and individuals. Stress is a major contributor to the exacerbation of acute and chronic illness, maintenance of suboptimal health, loss of employee productivity and job satisfaction, and difficulties in interpersonal relationships. The average health status of the US population is steadily declining, whereas the use of increasingly higher-cost technology and pharmaceuticals in conventional medicine is not producing better health. The United States currently spends $2.7 trillion each year or 18% of gross domestic product on health care, more than $6000 per individual and more than any other country in the world. Despite these expenditures, our infant mortality is 6.37/1000, which is higher than almost all other developed nations. Our life expectancy is 78 years (45th overall), well behind Switzerland, Germany, Bosnia, and Jordan to name a few. Americans should have the best health status in the world; unfortunately, we are ranked 37th. As noted in the Wall Street Journal editorial of March 19, 2007, “The health system isn’t healthy. There’s no denying it. A system that was designed to make you feel better often just makes things worse.”
Declining health status is likely to be the most significant event underlying the rising cost of health care. That, coupled with the escalating cost of pharmaceuticals and diagnostic testing, gives rise to a view of the future that is even bleaker than the present if nothing were to change. In spite of all the successes of conventional medicine, we have not delivered reliable ways of resolving chronic illness. The HFHS and the Center for Integrative Medicine has now proven in clinical trials for chronic back pain that complementary therapies are significantly more effective than the conventional care for resolving pain. Other research activities include completed clinical trials to evaluate the efficacy of complementary therapies to reduce or eliminate hot flashes in women with breast cancer, as well as migraine headaches.
The excellent research activities are limited only by resources to fund more groundbreaking work. Our centers are seeking philanthropic partners to provide funding to obtain the evidence that is critical for accelerating the integration of proven-effective complementary therapies into mainstream medicine.
Background on Our Center for Integrative Medicine
In December of 2001, HFHS began helping people with chronic back pain, persistent headaches, uncontrolled allergies, digestive problems, and a long list of other conditions to find permanent relief through treatments such as chiropractic, acupuncture, St. John neuromuscular therapy, Feldenkrais, mind-body therapies, and nutritional counseling. HFHS operates the free-standing Center for Integrative Medicine, headquartered in Novi, Michigan, which formally opened in June of 2002. The center represents one of the few that has a direct-care component in addition to research, and that is integrated with a nationally known medical center, such as HFHS.
Many of these therapies, which have been around for thousands of years, have been routinely rejected by mainstream Western medicine on the grounds of being unproven. Despite this resistance, our center sees nearly 1000 patients each month and more than 25% are referred to us from their physicians. Although this is exciting on the surface, we are usually seeing patients who have failed all forms of conventional options. Patients will benefit and health care costs will diminish when the paradigm of care provides patients concurrent access to complementary and conventional therapies; this is precisely what HFWB wellness hospital is providing. For example, the current paradigm for the patient with a cancer is to have a multidisciplinary conventional approach that includes the oncologist, the radiation therapist, and the surgeon. Our CIM philosophy supports the inclusion of the mind-body therapist, the acupuncturist, and the holistic nutritionist to the team to allow best practices from all vantage points to facilitate healing. This has yet to be implemented because of scant resources, but it is part of our vision and ultimate plan.
Current approaches
At HFHS, we employ practitioners that offer a variety of therapeutic approaches, both individual and combined, to support the total health and well-being of each person. Services offered include the following:
- •
Acupuncture
- •
Chiropractic
- •
Feldenkrais movement reeducation
- •
Herbal and nutritional counseling
- •
Holistic support for patients with cancer
- •
Health coaching
- •
Massage therapy
- •
Mind-body therapies (eg, hypnosis)
- •
Neuromuscular therapy.
The therapies are designed to compliment and integrate with conventional medicine for the treatment of many conditions including the following:
- •
Chronic pain (such as back, neck, hip, shoulder)
- •
Headaches (including migraines)
- •
Postural problems (scoliosis and “dowager’s hump”)
- •
Cancer
- •
Anxiety, depression, and stress
- •
Gynecologic and fertility problems
- •
Autoimmune diseases, such as rheumatoid arthritis
- •
Respiratory problems
- •
Wellness (smoking cessation, nutrition, weight management)
- •
Chronic fatigue
- •
Arthritis
- •
Digestive problems
- •
Vertigo and tinnitus
- •
Sports injuries
- •
Fibromyalgia
- •
Mobility problems
- •
Circulatory problems.
Our system offers these complementary therapies to patients both within and outside the HFHS, and works closely with Henry Ford specialties and centers, including the Josephine Ford Cancer Center, the Vattikuti Urology Institute, neurology, obstetrics and gynecology, otolaryngology, and orthopedics.
The HFHS Center for Wellness and the Center for Integrative Medicine research teams have already generated exciting research that has convinced the medical community and general public of the effectiveness of complementary therapies. A major example of the innovative, high-impact research conducted by Center for Integrative Medicine personnel is the recent successful group intervention program at Chrysler Corporation for employees with chronic back pain. Initial research has compared one-on-one conventional physical therapy to a hands-off group treatment approach with up to 48 Chrysler employees at a time. Although conventional physical therapy for people with chronic back pain provided a 5% resolution to zero pain, the group intervention produced a 55% resolution to zero pain (none of the control patients resolved to zero pain). The group intervention reduced the time of treating patients by more than 98% compared with typical one-on-one care. These remarkable results in resolving back pain at such high percentages using an efficient group intervention have never before been accomplished. Additional funding is paramount to validate this approach and apply it to other chronic conditions such as cancer, cardiovascular disease, diabetes, obesity, and others (Robert Levine, PhD, personal communication, 2012).
The Philosophy of CIM
The philosophy behind integrative medicine is that optimal health occurs when an individual has balance in mind, body, and spirit. When imbalances occur, they cause dysfunctions that can lead to organ and structural problems, as well as disease. Holistic practitioners recognize that people possess their own healing ability, so they work in partnership with patients to mobilize and enhance that ability in a way that takes into account each patient’s unique background and make-up.
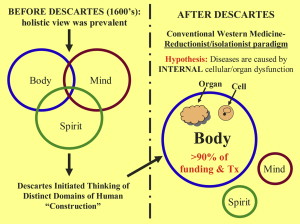
Before the 1600s, this holistic view of the individual was prevalent. René Descartes was the first to divide the human into separate and distinct entities. He proposed that the body could be treated for medical conditions independently, without considering other domains, such as mind or spirit. In Fig. 4 , the left panel provides a pictorial of the holistic view. The right panel shows that the Western medical paradigm, or way of thinking, developed as an outgrowth of Descartes’ philosophy. The predominant hypothesis of conventional medicine is that diseases are caused by dysfunctions within cells. This reductionist, or isolationist philosophy has permeated Western medicine. Long-term use of expensive medicines that only manage symptoms rather than correct problems is why chronic diseases are so prevalent and very costly to treat. Thus, chronic conditions are managed, but not cured. Most funding for basic research and clinical trials is focused on discovering and reversing dysfunction at the cellular level. There is minimal funding for any other approaches, which has limited most patients’ choices to conventional medicine options covered by health insurance.