Purpose
To compare the efficacy of topical umbilical cord serum drops (UCS) and amniotic membrane transplantation (AMT) in acute ocular chemical burns.
Design
Randomized controlled trial.
Methods
setting : Tertiary care hospital. study population : Forty-five eyes with acute chemical burns of grade III, IV, and V (Dua’s classification) presenting within the first week of injury were randomized into 3 groups (15 each). Patients with perforation/impending corneal perforation were excluded from the study. intervention : Groups 1, 2, and 3 received UCS with medical therapy (MT), AMT with MT, and MT alone, respectively. main outcome measure : Time to complete epithelialization.
Results
The mean time to complete epithelialization was 56.7 ± 14.9, 22.0 ± 10.2, and 22.9 ± 10.1 days in MT, AMT, and UCS groups, respectively, with a significant difference between MT and AMT ( P = .001) and between MT and UCS ( P = .001), but not between UCS and AMT ( P = .9). Improvement in pain score was better with UCS than AMT ( P value: .012, .002, and .012 on days 7, 14, and 21, respectively). Corneal clarity was better in the UCS group at 21 ( P = .008) and 30 days ( P = .002), but not at 3 months ( P = .9). By month 3, visual outcome, symblepharon, tear film status, and lid abnormalities were comparable between the 3 groups.
Conclusions
UCS and AMT, as an adjuvant to standard medical therapy in acute chemical injury, are equally efficacious. UCS has the advantage of faster improvement in corneal clarity, better pain control, and avoidance of surgery in an inflamed eye.
Ocular chemical burns are true emergencies that require rapid assessment and initiation of treatment. Chemical injuries of the eyes cause damage to the ocular surface epithelium, cornea, and anterior segment. Thus, immediate and effective treatment influences the final outcome favorably. The primary goals of therapy in ocular chemical burns include restoration of an intact ocular epithelium, control of inflammatory reaction, prevention of infection, support of reparative processes, and prevention of complications.
Standard medical therapy comprises topical steroids, topical antibiotics, mydriatics and cycloplegics, topical or oral antiglaucoma therapy, and topical citrate and ascorbate. Various newer treatment modalities have been tried during the acute phase to minimize the damage to the ocular surface, enhance the ongoing healing process, and prevent long-term sequelae. These newer modalities include oxygen therapy, amniotic membrane extract, amniotic membrane transplantation (AMT), and umbilical cord serum (UCS) eye drops. Both UCS and amniotic membrane are rich in growth factors, including EGF, NGF, FGF, TGF-β, vitamin A, fibronectin, and serum antiproteases such as α2-macroglobulin. Both have shown efficacy in acute ocular thermal burns. In this prospective randomized study, we compared the efficacy of AMT with UCS drops in the management of acute ocular chemical burns.
Materials and Methods
A prospective randomized controlled clinical trial was planned and approval from the institutional review board (IRB)/Ethics Committee of Dr Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi, India was taken. The research adhered to the tenets of the Declaration of Helsinki. The study has been registered under the Clinical Trials Registry, India (CTRI/2014/09/005067), National Institute of Medical Statistics, ICMR New Delhi ( www.ctri.nic.in ).
We included patients who presented with acute ocular chemical burns (grade III, IV, and V) according to Dua’s classification presenting within one week of injury and willing to participate in the study between the period from January 6, 2013 to January 10, 2014. So we evaluated both the limbal involvement and the conjunctival involvement and later calculated the analog score, as has been described by Dua’s classification. Hence, no separate mention has been made about the perilimbal ischemia in concordance with Dua’s classification. Informed consent was obtained from all the patients. Patients with grade I, II, and VI injury; those with perforation/impending corneal perforation; and those not willing to participate in the study were excluded from the study. A total of 51 eyes (30 patients, with 21 bilateral and 9 unilateral involvement) were recruited for the study. Three patients (with bilateral involvement) refused to participate in the study and hence were excluded. A written informed consent was obtained, and the patients were randomized into 3 groups using a random numbers table. Group I (n = 15) received conventional medical therapy (control group), Group II (n = 15) received AMT with conventional medical therapy, and Group III (n = 15) received 20% UCS drops along with conventional medical therapy. In bilateral cases, each eye was randomized separately. Appropriate first-aid therapy in the form of irrigation with normal saline to achieve a neutral pH and removal of any particulate matter from the ocular surface was done in all cases.
Group I (medical therapy [MT]) cases received conventional medical therapy, which included topical moxifloxacin hydrochloride 0.5% (Vigamox; Alcon, Fort Worth, Texas, USA) 4 times per day; sodium ascorbate (10%) and sodium citrate (10%) every 2 hours; preservative-free lubricants and topical prednisolone acetate 1% (Predforte; Allergan, Bangalore, India) every 2 hours; homatropine sulphate (2%) 4 times per day; and oral vitamin C (500 mg) 4 times a day, for 2–4 weeks. Antiglaucoma therapy in the form of timolol maleate (0.5%) 2 times per day and oral acetazolamide (250 mg) 3 times per day was given, when required.
Group II cases received AMT with conventional therapy. Amniotic membrane was collected from seronegative donors (human immunodeficiency virus [HIV], hepatitis B, hepatitis C, and syphilis) with uncomplicated caesarean section after obtaining informed consent. The amniotic membrane preparation was done using the standard technique, which has been previously described. AMT was done using the onlay technique. Surgery was performed under peribulbar or general anesthesia (if required) in adults and general anesthesia in children. After transferring the amniotic membrane onto the operative field, peeling off of the nitrocellulose membrane was done and the amniotic membrane was spread to cover the entire ocular surface, with the stromal side touching the ocular surface. Interrupted 8-0 Vicryl sutures (Ethicon; Johnson & Johnson, Ahmedabad, India) were used to anchor the underlying conjunctiva and the episclera to the amniotic membrane around the limbus. A symblepharon ring was then placed to uniformly spread the membrane and to flatten it against the ocular surface, especially in the fornices and along the palpebral conjunctiva. Additionally, interrupted Vicryl sutures were also applied to anchor the membrane along the lid margins. The eyes were bandaged after the surgery and the topical medications were continued in the postoperative period.
Group III cases received 20% UCS drops along with conventional medical therapy. The umbilical cord blood was collected from seronegative donors (hepatitis B, hepatitis C, HIV, and syphilis) with uncomplicated caesarean deliveries after obtaining informed consent. Screening for parenterally transmitted diseases was done at the time of antenatal care registration and further repeated at the time of cord blood collection and 3 months after the cord blood collection. Cord blood serum was prepared according to the standard technique, which has been previously described. Serum bottles were stored at −20 C before opening and at 4 C after opening. Patients were instructed to use serum vials within 7 days and to come back for a fresh vial after that. The patients were also instructed to look for the presence of any threadlike floating objects in the serum before instilling the drops and to discard the same vial if such contaminants were seen. The UCS eye drops (20%) were instilled 10 times per day until complete epithelialization was noted.
Baseline evaluation included a comprehensive history with reference to the nature of the chemical causing the damage to the ocular surface, duration of exposure to the chemical causing the injury, initial treatment received, and the time elapsed between exposure to the chemical and presentation at our centre. Best-corrected visual acuity (BCVA) was recorded using the logarithm of the minimal angle of resolution (logMAR) chart. Slit-lamp (Haag-Streit AG, Koeniz, Switzerland) examination was done. Other parameters noted at the initial visit included grade of chemical injury, corneal clarity, pain score, epithelial defect diameter (EDD), and the extent of limbal involvement. Additionally, epithelial defect area (EDA) was calculated as the product of the largest diameter and the diameter perpendicular to it. Tear film status was assessed using the Schirmer test and tear breakup time (TBUT), intraocular pressure, and any other anterior segment or fundus abnormalities were noted. Patients were followed up on days 3, 7, 14, and 21 and at the end of 1, 2, and 3 months. The parameters evaluated were time to epithelialization, size of the epithelial defect, corneal clarity grading, corneal vascularization, symblepharon formation, tear film status, lid abnormalities, limbal involvement, pain score, and visual acuity. Clinical photographs were recorded at each visit. The pain scoring was done using a numeric pain rating scale as summarized in Table 1 .
| Grade | Severity |
|---|---|
| 0 | No pain |
| 1 2 3 | Mild pain |
| 4 5 6 | Moderate pain |
| 7 8 9 10 | Severe pain |
Statistical Analysis
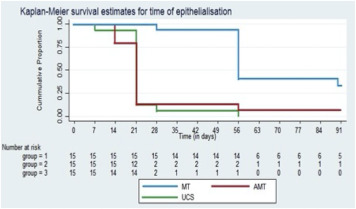
Keeping the power of the study as 0.8 and the level of significance at 0.05, with the primary outcome measure being the mean time for complete epithelialization, a minimum sample size of 15 eyes was required in each group. All patients completed the scheduled follow-up. The statistical analysis was done using SPSS software (International Business Machines Corp., New York, United States) for Windows. Time of epithelial healing was analyzed using Kaplan-Meier analysis. The χ 2 test and Fisher exact test were used for comparing qualitative data; for parametric quantitative data, 1-way analysis of variance (ANOVA) was used to compare intergroup means and Bonferroni correction was used to analyze post-test results; Kruskal-Wallis and Mann-Whitney tests were used for nonparametric quantitative data. For descriptive purposes, nonparametric data have been expressed as median (range), parametric qualitative data have been expressed as a percentage, and quantitative data have been expressed as mean ± standard deviation (SD).
Results
A total of 45 eyes with acute chemical burns were included and followed up for a period of 3 months. All patients completed the follow-up. The baseline characteristics, such as age, time between exposure and presentation, nature of chemical causing injury, treatment received initially, and Dua’s grading at presentation were comparable between the 3 groups ( Table 2 ).
| Baseline Variables | Standard Treatment Group (n = 15) | Amniotic Membrane Group (n = 15) | Cord Blood Serum Group (n = 15) | P Value |
|---|---|---|---|---|
| Age in years, mean ± SD | 21.9 ± 13.9 | 18.1 ± 11.3 | 22.9 ± 17.4 | .739 |
| Time between exposure and presentation in days, mean ± SD | 4.2 ± 1.4 | 3.9 ± 1.5 | 4.0 ± 1.2 | .953 |
| Nature of chemical | ||||
| Acid | 8 (53.3%) | 7 (46.7%) | 6 (40.0%) | .765 |
| Alkali | 7 (46.7%) | 8 (53.3%) | 9 (60.0%) | |
| Initial treatment received | ||||
| Yes | 8 (53.3%) | 8 (53.3%) | 6 (40.0%) | .701 |
| No | 7 (46.7%) | 7 (46.7%) | 9 (60.0%) | |
| Dua’s grading | ||||
| Grade III | 10 (66.7%) | 5 (33.3%) | 8 (53.3%) | .548 |
| Grade IV | 2 (13.3%) | 4 (26.7%) | 3 (20.0%) | |
| Grade V | 3 (20.0%) | 6 (40.0%) | 4 (26.7%) | |
Alkali burns were the most common, occurring in 24 eyes (53.3%), and acid burns occurred in 21 eyes (46.7%). The groups were comparable with regard to the nature of chemical exposure ( P = .765). According to Dua’s classification, 23 eyes had a grade III injury, 9 eyes had a grade IV injury, and 13 eyes had a grade V injury. The distribution was comparable across the groups ( P = .548) ( Table 2 ).
The epithelial defect had healed in all eyes in the UCS group, 14 of 15 eyes in AMT group, and 10 of 15 eyes in the MT group at 3 months follow-up. The mean time to complete epithelialization was 56.7 ± 14.9, 22.0 ± 10.2, and 22.9 ± 10.1 days in the MT, AMT, and UCS groups, respectively. The mean time for complete absorption of the amniotic membrane was 21 ± 3 days. The minimum and maximum times of healing were 28 and 91 days in the MT group, 14 and 56 days in the AMT group, and 7 and 56 days in the UCS group. The difference was statistically significant between the MT and AMT groups ( P = .001) and also between the MT and UCS groups ( P = .001), but no difference was found between the UCS and AMT groups ( P = .9). Kaplan-Meier survival analysis revealed that the differences in time of corneal epithelialization between the 3 groups were statistically significant ( Figure , P = .001).