Purpose
To investigate visual outcomes of Visian implantable Collamer lens (ICL) implantation in eyes with a shallow anterior chamber depth (ACD).
Design
Retrospective, noncomparative, interventional case series.
Methods
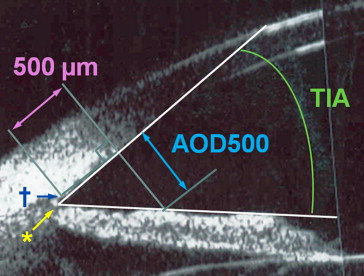
Medical charts of the patients with a low ACD of 2.8 mm or less who underwent implantable Collamer lens implantation were reviewed. To evaluate efficacy and safety, preoperative and postoperative uncorrected visual acuity, manifest refractive spherical equivalent (MRSE), endothelial cell count, intraocular pressure, angle opening distance at 500 μm from the scleral spur, trabecular–iris angle, and postoperative central vault were analyzed.
Results
The mean follow-up period for 18 eyes of 10 patients was 24.67 ± 15.09 months (range, 10 to 51 months). The preoperative ACD was 2.71 ± 0.08 mm (range, 2.42 to 2.79 mm). There was no postoperative endothelial cell count reduction to less than 2000 cells/mm 2 or intraocular pressure elevation to more than 21 mm Hg. The differences between preoperative and postoperative angle opening distance at 500 μm from the scleral spur and trabecular–iris angle were statistically significant ( P = .000, both). The mean postoperative central vault was 331.83 ± 181.28 μm (range, 174 to 811 μm), which was significantly less than expected ( P = .000). Anterior subcapsular cataract was observed in 2 eyes (11.1%).
Conclusions
Implantable Collamer lens implantation in shallow ACD eyes exhibited good visual outcomes. Severe complications did not develop over relatively long periods. Two cases of anterior subcapsular cataract developed in older aged patients, suggesting the need for thorough preoperative warning about the risk of cataract. In addition, a postoperative vault less than expected should be taken into account when determining implantable Collamer lens size in lower ACD eyes.
The Visian implantable Collamer lens (ICL; STAAR Surgical AG, Nidau, Switzerland) is a sulcus-placed posterior chamber phakic intraocular lens. Implantable Collamer lens implantation has several advantages, including faster visual recovery, more stable refraction, and better visual quality over keratorefractive surgeries; however, there are several possible complications associated with ICL position in the sulcus. The most common concerns regarding postoperative ICL complications are related to vault value (the distance between the back surface of the ICL and the anterior crystalline lens pole). An insufficient vault increases the risk of cataract formation, whereas excessive vault may cause secondary glaucoma resulting from angle closure, pupillary block, or pigment dispersion. Alfonso and associates reported that eyes with acute increase in intraocular pressure (IOP) are significantly more myopic and have a shallower anterior chamber depth (ACD). Therefore, obtaining the appropriate ACD required for posterior chamber phakic intraocular lens implantation is considered a major concern. The Communaut’ Europeen mark was obtained in Europe in 1997 for the Visian ICL model, which indicated an ACD requirement of more than 2.8 mm for myopia and more than 3.0 mm for hyperopia. However, in the United States, the Food and Drug Administration (FDA) suggests contraindications in patients with an ACD of less than 3.0 mm. Interestingly, the 2.8- or 3.0-mm criterion on ACD for posterior chamber phakic intraocular lens implantation is not based on concrete evidence, and thus is more of a suggestion than a result verified by clinical data. Further, there have been no previous studies on the safety or efficacy of ICL implantation in eyes with shallow anterior chamber, although based on the phakic refractive lens (Carl Zeiss Meditec, Dublin, California, USA) posterior chamber phakic intraocular lens models, Hoyos and associates reported a window defect of the iris and increased angular pigmentation without increased IOP in eyes with an ACD of 2.8 mm. The present study was undertaken to determine whether ICL implantation in eyes with a shallow ACD could be considered both clinically acceptable and safe.
Methods
This retrospective, noncomparative, interventional case series was approved by the Institutional Review Board of the Samsung Medical Center, and the work was carried out in accordance with the Declaration of Helsinki. This study included all patients with an ACD of less than 2.8 mm who underwent Visian ICL (model V4) implantation at the Samsung Medical Center between September 2007 and March 2012. Anterior chamber depth was measured from the corneal endothelium to the anterior surface of the crystalline lens using preoperative ultrasound biomicroscopy (UBM). Additional inclusion criteria were a postoperative follow-up period of at least 6 months, availability of preoperative and postoperative UBM data, and no abnormal sulcus structures such as an iridociliary cyst. This is an off-label use of ICL, and implanting in a shallow anterior chamber carries extra risk in it. The possibility of increased risk of complications related to a shallow ACD was explained and understood by all patients, and both oral and written informed consent was obtained before the surgery.
The medical charts of enrolled patients were reviewed to obtain patient demographics, clinical examination details, procedures, and complications. Indications for ICL implantation included myopia of at least −5.0 diopters (D), stable refraction for at least 1 year before surgery, 20 years of age or older, no pre-existing ocular pathologic features, no previous ocular surgery, an IOP between 10 and 21 mm Hg, corneal endothelial cell counts (ECCs) of more than 2000 cells/mm 2 , anterior chamber angle more than grade II by gonioscopy, and a clear crystalline lens. Implantable Collamer lens power calculations were performed with software provided by STAAR Surgical AG based on corneal topographic values (Orbscan IIz; Bausch & Lomb, Rochester, New York, USA). Implantable Collamer lens size was determined using the UBM-based sulcus-to-sulcus method as previously reported by the authors of this study. First, dimples that recognize the position of the limbus as a physical marker were made using a caliper at the 9-o’clock horizontal limbus. Second, the patient was reclined, and a 20-, 22-, or 24-mm open shell was inserted between the upper and lower eyelids and filled with sterile balanced salt solution. The reclined patient was asked to fixate on a target with the fellow eye maintaining fixation. Cross-sectional images were obtained through the cornea, iris, ciliary body, and lens at the 3-, 6-, 9-, and 12-o’clock positions covering 360 degrees of the anterior chamber. At the 9-o’clock cross-sectional image, an imaginary line was drawn from the limbal dimple perpendicular to the posterior surface of the iris. The distance from the intersection of the imaginary perpendicular line and posterior iris plane to the ciliary sulcus was measured from the UBM scan. Similarly, the distance was also measured 180 degrees apart at the 3-o’clock horizontal limbus. These distances (D, D′) were added to the white-to-white (WTW) horizontal corneal diameter to determine the sulcus-to-sulcus horizontal diameter (STH): STH = D + WTW horizontal corneal diameter + D′. Because the UBM gave a partial view of sulcus, the sulcus-to-sulcus horizontal diameter distance was estimated by adding sulcus to limbus distance measured on each side by UBM and WTW horizontal corneal diameter measured by Orbscan or caliper.
All surgeries were conducted in a standard fashion by 2 skilled surgeons (T.-Y.C., E.-S.C.). Two weeks before ICL implantation, all patients underwent 2 peripheral and superior iridotomies with an argon and neodymium:yytrium–aluminum–garnet laser to prevent pupillary block. Iridotomies were located superiorly and approximately 90 degrees apart. All surgeries were performed under topical anesthesia. A 3.0-mm temporal clear corneal incision and paracentesis were made with a diamond knife. If eyes had 0.50 to 1.00 D of astigmatism superiorly, we implanted a spherical ICL and adopted a superior clear corneal incision to reduce astigmatism. Viscoelastics (Hyal 2000; LG Life Sciences, Seoul, South Korea) were injected into the anterior chamber and the ICL was inserted through the incision with an injector (MicroSTAAR injector; STAAR Surgical AG) and allowed to unfold slowly. The distal and proximal footplates were tucked under the iris with a modified intraocular spatula. All spherical ICLs were intended to be implanted with a 180-degree horizontal orientation. Toric ICLs were implanted in eyes with a preoperative cylindrical power of more than 1.00 D at the spectacle plane. Any remaining viscoelastic material was aspirated meticulously by irrigation with a balanced salt solution. Levofloxacin (Cravit; Santen Pharmaceutical, Osaka, Japan) and fluorometholone (Flumetholon; Santen Pharmaceutical) eye drops were used 4 times daily for 1 month after surgery.
Data from enrolled patients included complete preoperative and postoperative ocular examinations. To evaluate visual outcomes and efficacy after ICL implantation, uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) using the Snellen chart (converted to the logarithm of the minimal angle of resolution [logMAR] scale), manifest refractions, and cycloplegic refractions were analyzed. To evaluate safety, IOP measurements obtained by pneumatic tonometry (TX-F Full Auto Tonometer; Canon, Inc, Utsunomiyashi, Tochigiken, Japan) and corneal ECC measurements obtained by specular microscopy (SP-8000; Konan Medical, Inc, Nishinomiya, Hyogo, Japan) were analyzed. Ultrasound biomicroscopy (UBM 835, Carl Zeiss Meditec) data were obtained using a 50-MHz transducer to measure the distance from sulcus-to-sulcus plane to the anterior crystalline lens surface, the preoperative and postoperative angle opening distance at 500 μm from the scleral spur (AOD500), and the trabecular–iris angle, which subsequently were exported to image analysis software (ImageJ 1.32j; developed by Wayne Rasbands, National Institutes of Health, Bethesda, MD, USA; Figure 1 ).
The postoperative central vault was compared with the expected vault value as previously described by the authors of this study. The preoperative horizontal sulcus-to-sulcus diameter was measured using a Hi-Scan UBM (Optikon 2000, Rome, Italy) with a 35 MHz-probe.
All statistical analyses were carried out using commercial software (PASW Statistics version 18; SPSS, Inc, Chicago, Illinois, USA). The data were analyzed using a paired t test or Wilcoxon signed-rank test where appropriate. The significance level was set at a P value of less than .05.
Results
The study included 18 eyes of 10 patients with a mean age of 34.22 ± 7.87 years (range, 23 to 47 years) and a mean follow-up period of 24.67 ± 15.09 months (range, 10 to 51 months). All patients were women, and the mean preoperative ACD was 2.71 ± 0.08 mm (range, 2.42 to 2.79 mm) according to UBM. The mean preoperative UCVA and BCVA were 1.56 ± 0.33 logMAR (range, 1.0 to 2.0 logMAR) and 0.07 ± 0.10 logMAR (range, 0 to 0.3 logMAR), respectively, and the mean preoperative spherical equivalent was −11.40 ± 4.65 D (range, −5.5 to −24.5 D). Table 1 shows the baseline patient characteristics and preoperative biometry.
| Characteristics | Mean ± SD (N = 18 eyes) | Range (Minimum, Maximum) |
|---|---|---|
| Age (y) | 34.22 ± 7.87 | 23, 47 |
| Follow-up (mos) | 24.67 ± 15.09 | 10, 51 |
| UCVA (logMAR) | 1.56 ± 0.33 | 1.0, 2.0 |
| BCVA (logMAR) | 0.07 ± 0.10 | 0.0, 0.3 |
| Spherical refractive error (D) | −10.68 ± 4.83 | −5.75, −24.0 |
| Cylindrical refractive error (D) | −1.47 ± 1.57 | 0.0, −4.5 |
| Spherical equivalent (D) | −11.40 ± 4.65 | −5.5, −24.5 |
| ACD (mm) | 2.71 ± 0.08 | 2.42, 2.79 |
| STS (mm) | 11.70 ± 0.55 | 10.46, 12.32 |
| ECC (cells/mm 2 ) | 2987.78 ± 232.35 | 2617, 3377 |
| STSL (mm) | 0.79 ± 0.22 | 0.33,1.17 |
A spherical ICL was implanted in 12 eyes and a toric ICL was implanted in 6 eyes. The mean postoperative UCVA and BCVA were 0.07 ± 0.14 logMAR (range, 0 to 0.5 logMAR) and 0.04 ± 0.08 logMAR (range, 0 to 0.2 logMAR), respectively, which exhibited a statistically significant improvement ( P < .001). The overall efficacy index (given by mean postoperative UCVA/mean preoperative BCVA) was 0.99 and the safety index (ratio of postoperative and preoperative BCVA) was 1.06. No eyes lost 1 or more lines of BCVA, 14 eyes retained the same BCVA, and 4 eyes gained 1 line of BCVA after surgery.
The mean postoperative spherical equivalent was −0.51 ± 1.45 D (range, −5.75 to 0.75 D). With the exception of 3 eyes that were targeted for −1.0 D, −1.75 D, and −3.0 D because of ICL unavailability for eyes with extremely high myopia, the remaining 15 eyes were targeted for emmetropia. The mean spherical equivalent of 15 eyes of 9 patients other than the 3 eyes with a myopic target as described above was 0.00 ± 0.34 D (range, −0.25 to 0.75 D), and of these 15 eyes, 13 (86.7%) exhibited a postoperative UCVA of 20/20 or better. In addition, 13 (86.7%) of the 15 eyes were within ± 0.50 D, whereas all 15 eyes (100%) were within ± 0.75 D of emmetropia. Among the 18 eyes included in this study, 16 (88.9%) were within ± 0.50 D of the desired refraction and 17 (94.4%) were within ± 1.00 D of the target refraction after surgery.
The mean IOP measured at the last follow-up visit was 15.22 ± 2.56 mm Hg (range, 10 to 21 mm Hg), and there was no IOP elevation to more than 21 mm Hg. The mean ECC at the last visit was 2717.88 ± 247.80 cells/mm 2 (range, 2352 to 3355 cells/mm 2 ). Endothelial cell count showed a significant reduction of 9.03% ( P = .003, paired t test) compared with the preoperative value; however, there was no ECC reduction to less than 2000 cells/mm 2 ( Table 2 ). The preoperative to postoperative decreases for both AOD500 and trabecular–iris angle were statistically significant ( P = .000 for both, paired t test), as shown in Table 3 . The values of AOD500 and trabecular–iris angle after ICL implantation changed from 370.56 ± 105.27 μm to 265.27 ± 112.83 μm and from 31.92 ± 6.78 μm to 23.27 ± 8.14 μm, respectively. Thus, the ratio of reduction of AOD500 and trabecular–iris angle were 27.32% and 28.41%, respectively. All of the eyes in the study had a trabecular–iris angle of more than 20 degrees on preoperative UBM; however, 4 eyes (22.2%) had a trabecular–iris angle of less than 20 degrees after surgery, which corresponds to Shaffer grade 2, and the same occludable angle on postoperative UBM.
| Mean ± SD (N = 18 eyes) | Range (Minimum, Maximum) | |
|---|---|---|
| UCVA (logMAR) | 0.07 ± 0.14 | 0.0, 0.5 |
| BCVA (logMAR) | 0.04 ± 0.08 | 0.0, 0.2 |
| Spherical equivalent (D) | −0.51 ± 1.45 | −5.75, +0.75 |
| IOP (mm Hg) | 15.22 ± 2.56 | 10, 21 |
| ECC (cells/mm 2 ) | 2717.88 ± 247.80 | 2352, 3355 |
| Implanted ICL size (mm) a | 11.92 ± 0.35 | 11.5, 12.5 |
| Vault (μm) | 331.83 ± 181.28 | 174, 811 |
a Spherical ICL and toric ICL were implanted in 12 and 6 eyes, respectively.
| Mean ± SD | % Remaining | P Value a | ||
|---|---|---|---|---|
| Preoperative | Postoperative | |||
| AOD500 (μm) | 370.56 ± 105.27 | 265.27 ± 112.83 | 72.68 | .000 |
| TIA (degree) | 31.92 ± 6.78 | 23.27 ± 8.14 | 71.59 | .000 |
The mean postoperative vault was 331.83 ± 181.28 μm (range, 174 to 811 μm). A total of 8 (44%) of the 18 eyes in the study exhibited a low vault of less than 250 μm, 9 eyes (50%) exhibited a vault between 250 and 750 μm, and 1 eye (6%) exhibited a high vault of more than 750 μm.
No adverse events were recorded during the surgery, and there were no findings of postoperative intraocular inflammation (eg, uveitis or endophthalmitis). No pupillary block, pigmentary glaucoma, or increased postoperative IOP requiring medication were noted during the follow-up period. An anterior subcapsular cataract (ASC) developed in 2 eyes (11.1%). Among the 2 cataract cases, a clinically significant cataract causing visual impairment developed in 1 eye, which was treated by ICL explantation and cataract surgery. Implantable Collamer lens exchange was performed in the other 2 eyes (11.1%) because of inadequate ICL vaulting. The clinical characteristics of the 4 complicated cases are summarized in Table 4 . Figure 2 shows postoperative UBM and anterior segment photographs of eyes in which ASC occurred.
| Patient No. | Age (y) | Preoperative Characteristics | Postoperative Characteristics | Intervention | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BCVA | SE (D) | ACD (mm) | WTW (mm) | STS (mm) | STSL (mm) | ICL (mm) a | BCVA | Vault (μm) | Clinical Findings | |||
| 1 | 47 | 20/20 | −12.75 | 2.69 | 11.5 | 11.86 | 0.96 | 12.0 | 20/20 | 198 | ASC was found at 11 mos after surgery | None |
| 2 | 45 | 20/40 | −24.0 | 2.42 | 11.4 | 11.05 | 1.17 | 11.5 | 20/32 | 197 | ASC was found at 8 mos after surgery | ICL explantation and cataract surgery was performed, resulting 20/20 vision |
| 3 | 30 | 20/20 | −8.625 | 2.65 | 11.3 | 11.63 | 0.54 | 12.0 | 20/20 | 231 b | Vault was high and peripheral angle was apposed after ICL implantation | ICL was replaced with 11.5-mm ICL at 1 wk after surgery |
| 4 | 31 | 20/20 | −8.25 | 2.72 | 11.5 | 12.14 | 1.01 | 12.0 | 20/20 | 204 b | Vault was 162 μm after initial ICL implantation | ICL was replaced with 12.5-mm ICL at 1 mo after surgery |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


