Purpose
To report changes in health-related quality of life (HRQOL) 1 year following strabismus surgery.
Design
Retrospective cohort study.
Methods
Seventy-three adults undergoing strabismus surgery in a single clinical practice completed the Adult Strabismus-20 (AS-20) HRQOL questionnaire preoperatively and at 6 weeks and 1 year postoperatively. All included adults were successfully aligned at 6 weeks postoperatively. Success was defined based on clinical criteria. Change in AS-20 psychosocial and function scores was evaluated as: 1) difference in scores between 6 weeks and 1 year postoperatively and 2) proportions exceeding previously published limits of agreement at 6 weeks and 1 year.
Results
For patients successfully aligned at both 6 weeks and 1 year (n = 51), further improvement in median scores was seen from 6 weeks to 1 year for both the psychosocial scale (83.8 vs 93.8; P < .0001) and the function scale (72.5 vs 77.5; P = .007). Also, a greater proportion exceeded limits of agreement at 1 year than at 6 weeks (psychosocial: 48% vs 30%; P = .007, function: 67% vs 51%; P = .01). For patients who became partial success (n = 18) or failure (n = 4) at 1 year there was a numerical decrease in scores at 1 year.
Conclusions
Adult strabismus patients who remain successfully aligned show continued improvement in both psychosocial and function scores from 6 weeks to 1 year postoperatively, indicating that improvement in HRQOL is long-lasting. Evaluation of HRQOL should be considered when reporting strabismus surgery outcomes in clinical trials, and may prove helpful in assessing outcomes in clinical practice.
We have previously reported the development and validation of the Adult Strabismus-20 (AS-20), a health-related quality of life (HRQOL) questionnaire for adults with strabismus. Using this questionnaire, we found initial (6-week) postoperative improvement in HRQOL following successful strabismus surgery, and also found that the AS-20 discriminated well between patients classified as surgical success, partial success, or failure. Nevertheless, it is unknown how strabismus surgery may affect HRQOL over a longer period of postoperative follow-up. In this present study, we evaluated changes in HRQOL 1 year following strabismus surgery, in patients successfully aligned at 6 weeks.
Methods
Patients
Seventy-three adult strabismus patients were prospectively recruited. Because we were interested in evaluating long-term change in HRQOL scores in patients who were initially successfully aligned postoperatively ( Table 1 ), we included only patients designated as surgical “success” at their 6-week outcome exam. All included patients completed the AS-20 preoperatively, at 6 weeks (median 7 weeks, range 4 to 14 weeks), and at 1 year (median 12 months, range 5 to 22 months) postoperatively. Fifty-six of 73 (77%) had strabismus with binocular diplopia and evidence of fusion potential and 17 (23%) had strabismus without diplopia. One of the 56 diplopia patients (1%) had visual confusion but was grouped with diplopia patients, because the aim of surgery was to relieve symptoms of visual confusion. Patients were not recruited if they could not read or understand English or if they had severe cognitive impairment, and we excluded patients with ocular myasthenia gravis because the condition may vary from day to day. Median age of our 73 included patients was 53 (range 18 to 88) years; 50 (68%) were female and 69 (95%) self-reported their race as “white.” Thirty-four (47%) had undergone previous surgery in a separate episode of care. Fifty-one of 73 patients underwent uniplanar surgery: 41 (56%) horizontal, 7 (10%) vertical, and 3 (4%) torsional. Twenty-two of 73 patients underwent multiplanar surgery: 10 (14%) horizontal and vertical, 7 (10%) vertical and torsional, 4 (5%) horizontal and torsional, and 1 (1%) combined horizontal, vertical, and torsional surgery. Median visual acuity was 20/20 (range 20/15 to 20/40) in the better eye and 20/25 (range 20/15 to count fingers) in the worse eye. Overall, 1 of the 73 subjects (1%) was in prism correction at the 6-week assessment and 10 (14%) at their 1-year outcome assessment. Preoperative AS-20 data have been reported on 54 of 73 patients (74%) in previous analyses. Six-week postoperative AS-20 data have been previously reported on 53 of 73 patients (73%). One-year data have not been previously reported.
| Success a | Partial Success a | Failure a | |
|---|---|---|---|
| Angle of deviation by SPCT | <10 prism diopters straight ahead distance and near | ≤15 prism diopters straight ahead distance and near (without prism) | >15 prism diopters straight ahead distance or near (without prism) |
| Diplopia/visual confusion | None or “rare” straight ahead distance and reading | None, “rare,” or “sometimes” straight ahead distance and reading. | “Always” or “often” straight ahead distance or reading |
| Prism | Not allowed | Allowed | Allowed |
| Bangerter foil/occlusion | Not allowed | Not allowed | Allowed |
a For classification as success or partial success, all listed criteria had to be met; for classification as failure, only 1 criterion had to be met. If the criteria for more than 1 outcome group were met, the patient was allocated to the group with the better outcome.
Clinical Assessment and Questionnaire Administration
Angle of deviation was measured preoperatively and postoperatively, at distance and near, using simultaneous prism and cover test (SPCT) and prism and alternate cover test (PACT). For 3 of 17 nondiplopic patients, Krimsky measurements were used as visual acuity did not allow accurate cover testing. Patients completed the AS-20 questionnaire at preoperative and postoperative assessments. Questionnaires were self-administered, without supervision, following simple verbal and written instructions, and were typically completed before any clinical examination procedures had been performed. Patients were instructed to respond as when wearing any habitual refractive correction, including prism if prescribed.
The AS-20 consists of 20 items in 2 subscales, 10 in a psychosocial subscale and 10 in a function subscale (full questionnaire with user instructions available at: http://publicfiles.jaeb.org/pedig/Misc/AS-20%20Questionnaire.pdf , accessed September 30, 2011). For each question a 5-point Likert-type scale is used for responses: “never” (score 100), “rarely” (score 75), “sometimes” (score 50), “often” (score 25), and “always” (score 0). A psychosocial score (10 items), and function score (10 items) is calculated as a mean of all answered items and ranges from 0 to 100 (worst to best HRQOL). One patient overlooked the psychosocial subscale questions at the preoperative examination and 1 overlooked the psychosocial subscale at the 6-week postoperative examination; therefore preoperative-to-postoperative differences on the psychosocial scale could not be calculated for these 2 patients (total 71 patients for analyses of psychosocial subscale).
Classification of Postoperative Outcomes
We defined postoperative outcome groups a priori, based on clinical criteria alone ( Table 1 ). Three postoperative outcome categories were created: success, partial success, and failure. If patients met the criteria for more than 1 group, they were allocated to the group with the better outcome. Classification as success required no diplopia/visual confusion (or only “rare”) straight ahead distance and for reading, with less than 10 prism diopters (PD) heterotropia in primary position at distance and near by SPCT. Classification as partial success required diplopia/visual confusion present “sometimes” or less straight ahead distance and for reading (with or without prism), and no more than 15 PD heterotropia. Classification as surgical failure was assigned if either diplopia/visual confusion was “often” or “always” straight ahead distance or for reading, or if there was more than 15 PD heterotropia at distance or near, or the patient was using a Bangerter foil/occlusion. Patients classified as failure at 1 year continued under clinical care for further management, but additional treatment and outcome data are not reported in the present study.
For assessment of diplopia frequency, we have increasingly used a revised diplopia questionnaire (Smith SJ, Liebermann L, Hatt SR, Leske DA, Holmes JM. Quantifying diplopia using a patient-reported outcome questionnaire. Invest Ophthalmol Vis Sci 2011;52:ARVO E-Abstract 6361), completed by the patient. Revised diplopia questionnaire data were available, and used for classification of outcomes, in 9 of 73 patients (12%) at 6 weeks and 43 of 73 (59%) at 1 year. If revised diplopia questionnaire data were not available, frequency of diplopia was ascertained using the medical history.
Analyses
AS-20 psychosocial and function scores were calculated for each patient at the preoperative assessment and at 6 weeks and 1 year postoperatively, as the mean of all answered items. Preoperative, 6-week postoperative, and 1-year postoperative AS-20 psychosocial and function scores were analyzed in 2 ways: 1) difference between scores from preoperatively to 6 weeks postoperatively and from 6 weeks to 1 year postoperatively, compared using signed rank tests, reporting medians and quartiles of the scores; 2) comparison of proportions exceeding previously published 95% limits of agreement (LOA) (psychosocial scale 17.7 points; function scale 19.5 points ), using McNemar tests. Analyses were performed across all patients, and separately for diplopic and nondiplopic patients, without regard to success status at 1 year. A secondary analysis was performed for subgroups according to success status at 1 year: 1) success at both 6 weeks and 1 year; 2) success at 6 weeks, partial success at 1 year; 3) success at 6 weeks, failure at 1 year. All statistical analyses were performed using SAS computer software version 9.1.3 (SAS Institute, Inc, Cary, North Carolina, USA).
Results
Postoperative Outcomes
By study design, all 73 included patients were classified as success at 6 weeks. Overall, 51 (70%) were successfully aligned at both 6 weeks and 1 year postoperatively, 18 (25%) become partial successes at 1 year (17 diplopic, 1 nondiplopic), and 4 (5%) became failures at 1 year (3 diplopic, 1 nondiplopic). For diplopia patients, 36 of 56 (64%) were a success at both 6 weeks and 1 year. For nondiplopic patients, 15 of 17 (88%) were a success at both 6 weeks and 1 year.
Median Change
AS-20 psychosocial score
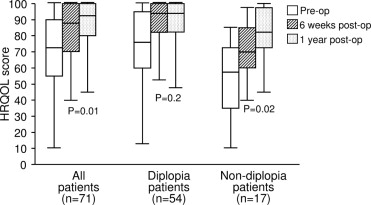
Across all patients (n = 71 with preoperative and postoperative psychosocial scores), median AS-20 psychosocial score improved from 72.5 (quartiles 55.0, 90.0) preoperatively to 87.5 (70.0, 100.0; P < .0001) 6 weeks postoperatively ( Figure 1 ) . There was further improvement in psychosocial scores at 1 year postoperatively (92.5 [80.0, 100.0]; P = .01). For nondiplopic patients, median psychosocial score improved from 57.5 (35.0, 72.5) preoperatively to 70.0 (60.0, 85.0; P = .0006) 6 weeks postoperatively, with further improvement at 1 year postoperatively (82.5 [72.5, 97.5] P = .02) ( Figure 1 ). For diplopic patients, median psychosocial scores improved from 76.3 (60.0, 95.0) preoperatively to 93.8 (82.5, 100.0; P < .0001) at 6 weeks postoperatively; however, there was no further improvement in scores at 1 year (93.8 [82.5, 100.0]; P = .2) ( Figure 1 ).
For the 50 patients classified as success at both 6 weeks and 1 year (with preoperative and postoperative psychosocial scores), median psychosocial score improved from 71.3 (50.0, 90.0) preoperatively to 83.8 (70.0, 100.0; P < .0001) at 6 weeks postoperatively ( Figure 2 ) . There was further improvement in psychosocial scores at 1 year postoperatively (93.8 [80.0, 100.0]; P < .0001) ( Figure 2 ). Both diplopia patients (n = 35) and nondiplopia patients (n = 15) who were a success at both 6 weeks and 1 year showed further improvement in scores at 1 year ( P < .03 for each comparison). For the 17 patients who became a partial success at 1 year, median psychosocial score improved from 82.5 (72.5, 90.0) preoperatively to 92.5 (85.0, 100; P = .002) 6 weeks postoperatively, but there was no further improvement in scores at 1 year (90.0 [80.0, 97.5]; P = .2) ( Figure 2 ). For the 4 patients who became failures at 1 year, there was a large numerical improvement from preoperatively (47.5 [32.5, 75.0]) to 6 weeks postoperatively (100.0 [70.0, 100.0]; P = .1), but this did not reach statistical significance because of small sample size. For these 4 failures at 1 year, there was a numerical decrease in 1-year psychosocial score (73.8 [46.3, 100.0]; P = .99) ( Figure 2 ).
AS-20 function score
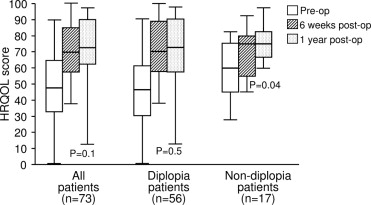
Across all patients, median AS-20 function score improved from 47.5 (quartiles 32.5, 65.0) preoperatively to 70.0 (57.5, 85.0; P < .0001) at 6 weeks postoperatively. There was no further improvement in median function score at 1 year postoperatively (72.5 [62.5, 90.0]; P = .1) ( Figure 3 ) . For diplopic patients median function score improved from 46.3 (30.0, 61.3) preoperatively to 70.0 (57.5, 88.8; P < .0001) 6 weeks postoperatively, but there was no further improvement in scores at 1 year (72.5 [57.5, 90.0]; P = .5) ( Figure 3 ). For nondiplopic patients, median function score improved from 60.0 (45.0, 75.0) preoperatively to 75.0 (55.0, 80.0; P = .04) at 6 weeks postoperatively, with further improvement in scores at 1 year postoperatively (75.0 [66.7, 82.5]; P = .04) ( Figure 3 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


