Purpose
To consider the pathogenesis and growth of cavernous hemangioma, particularly within the crowded orbital apex, in decisions regarding surgical indications, timing, and technique.
Design
A perspective based on analysis of the microanatomic relationships and growth potential of apical cavernous hemangiomas, with representative case studies illustrating management recommendations.
Methods
Analysis of microscopic findings in typical and vision-loss cases; review of tumor growth patterns as reported in observational and interventional studies; consideration of surgical approaches and reported functional outcomes.
Results
An ongoing, local hemodynamic imbalance may drive the proliferation of a cavernous hemangioma. Extension into neighboring tissue induces a fibrous capsule, which is continually reconstituted as the lesion expands, and which may incorporate visually critical structures in the confines of the apex. The extent of this microanatomic intimacy is not detectable preoperatively. The tumor’s remaining growth potential at the time of diagnosis or following incomplete resection is not predictable.
Conclusions
Patients without significant vision deficits should be observed for progression. Those with significant deficits or signs of progression should be offered timely surgery, with recognition of the risks. The surgical approach should be individualized based on macroanatomic relationships. The decision to intervene should not be a commitment to complete resection at any cost; intraoperative recognition of “inoperable” attachments may dictate modifications in order to preserve vision.
The past few decades have witnessed major strides in the field of orbital surgery. Insights into the pathogenesis of orbital disease have refined surgical indications and objectives. Appreciation of anatomic relationships, aesthetically sensitive incisions and dissection paths, respectful tissue handling, and discrete hemostatic techniques have all enhanced effectiveness while reducing collateral damage. Arguably, the most significant development has been high-resolution imaging, which effectively transformed the orbitotomy from an exploratory adventure to a precisely planned, goal-directed mission.
Despite these advances, the management of small hemangiomas lodged deep in the orbital apex has remained a challenge. Some lesions, generally those found incidentally in asymptomatic patients scanned for unrelated reasons, remain unchanged in long-term follow-up. Others cause progressive functional deficits, and even minor incremental growth can have major impact in the densely packed region. In such cases, early intercession would seem to be clearly indicated. On the other hand, because of often tenacious attachments to fixed apical structures, even careful surgical removal can imperil vision. The surgeon and patient, therefore, are faced with difficult decisions of whether, when, and how to intervene. Although no single solution may be applicable to every case, consideration of a hemangioma’s pathogenesis and growth—particularly within the orbital apex—can inform our surgical judgment regarding indications, timing, and technique.
Cavernous hemangioma is the most common benign orbital tumor in adults. Quantitative data specific to the orbital apex are lacking, but hemangiomas likely represent a major proportion of well-circumscribed, round-to-oval masses in the region. Based on their signal intensity in conventional magnetic resonance imaging (MRI) scans (isointense to muscle in T1-weighted images; hyperintense in T2-weighted images), and their contrast-enhancement spread pattern in dynamic MRI scans (starting from one point or portion, rather than a wide area), imaging usually allows their differentiation from other apical tumors, such as schwannoma, neurofibroma, or meningioma. Based on their low-flow arterial input, they can generally be distinguished from other well-circumscribed vascular lesions, such as hemangiopericytoma, with multiphase dynamic computed tomography (CT) or MRI scanning.
A cavernous hemangioma is not a neoplasm in the usual sense of the term: it does not derive from a single, proliferating progenitor cell. Rather, it consists of interconnected, endothelially lined vascular channels with stromal septa of varied thickness ( Figure 1 , Top left and Top right). The observation of “budding” of the vascular spaces into the interstitium (a finding seen in arteriovenous fistulas) led Harris and Jakobiec to speculate that a low-grade, local hemodynamic shift could open new channels and promote their extension into surrounding tissue. We might take that pathogenetic concept a bit further, and relate it to the morbidity of both apical tumor growth and apical tumor removal.
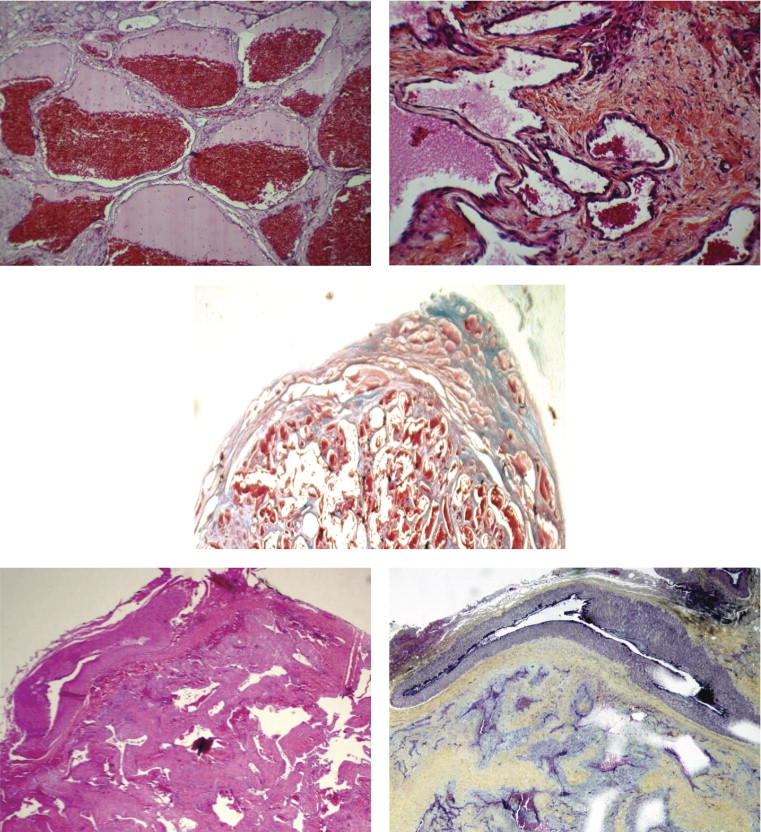
As the neovascular network slowly advances into neighboring tissue, it induces a fibrous capsule at the interface ( Figure 1 , Center). Continued growth involves further budding of vascular channels into both the internal septa and the fibrous perimeter. The capsule, therefore, is continuously reconstituted just beyond the expanding plexus. In the process, it must displace, compress, or incorporate surrounding structures. In the anterior and middle orbit, the relatively mobile muscles, nerves, vessels, and loose fibrofatty matrix can generally accommodate that slow expansion by moving aside. Compression to the point of visual impairment tends to occur only with larger tumors, and substantial infiltration by the advancing capsule is uncommon. Because adhesions are tenuous, surgical extraction can often be easily accomplished with a cryoprobe.
In the orbital apex, in contrast, visually critical vessels and nerves are tightly compacted and directly apposed, with virtually no intervening fibrofatty matrix. Without room for displacement, tumor expansion takes a toll by compression and/or incorporation. Figure 1 (Bottom left and Bottom right) demonstrates the apical tumor of a patient with dense, diffuse visual field loss and acuity of 20/800 prior to removal. At one pole of the histopathologically confirmed cavernous hemangioma is the ophthalmic artery, whose adventitia was annexed by the lesion’s advancing capsule. The tumor’s fusion with the wall of the artery and compression of its lumen, rather than direct impact on the optic nerve, may have been the primary mechanism of the vision loss. That growth pattern also precluded surgical separation of the artery and tumor. The findings suggest that although cavernous hemangiomas are grossly well circumscribed and encapsulated, rather than diffuse and infiltrative, the distinction may be less clinically relevant in the crowded apex than elsewhere in the orbit. Indeed, the degree to which visually critical structures have been expropriated by tumor growth can be crucial in the surgical outcome. Unfortunately, such microanatomic details are not detectable preoperatively.
In formulating a management scheme, we should also consider what is known about the clinical behavior of these tumors. Orcutt and associates followed 11 visually asymptomatic patients with presumed cavernous hemangiomas that were found incidentally in scans for unrelated reasons (eg, headache, vertigo). All lesions were intraconal; those that were apical were not specified. All 11 patients were observed without treatment for an average of 3 years (range, 8 months to 10 years), and no tumor enlarged. The series, which did not include symptomatic patients who underwent surgery, suggests that at least some cavernous hemangiomas will cease growing spontaneously. In our pathogenetic construct, that might imply that local hemodynamic forces have equilibrated. Other hemangiomas, however, clearly do not lose their impetus for growth—even through decades of progressive expansion ( Figure 2 ).
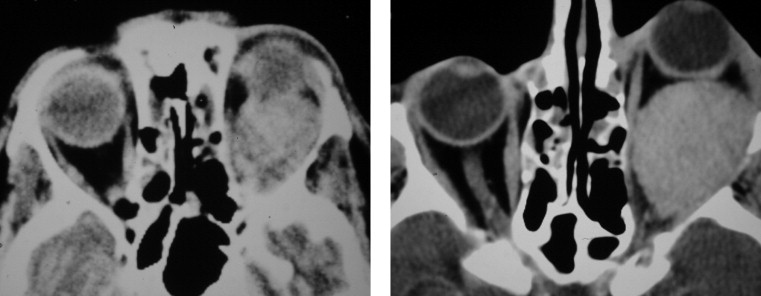
Harris and Jakobiec reviewed 66 cases of cavernous hemangioma that had been surgically removed, on average, 10 years earlier. In that archival series, almost every case antedated CT scanning, and rather than being incidental findings, the lesions had actively grown to cause proptosis or impair vision. Although several tumors among the 66 had been incompletely excised (according to the operating surgeon or the reviewing pathologist), none recurred. In those cases, partial resection and/or surrounding postoperative changes might have rebalanced hemodynamic factors. However, as with the natural history, the long-term course after incomplete resection is not uniform or predictable. Figure 3 demonstrates the slow, continued growth of a subtotally excised tumor (not detected in a scan 5 years after surgery, but clearly visible 15 years later). In yet another variation, Henderson and associates followed a patient with an incompletely excised cavernous hemangioma for 18 years. The residual tumor enlarged during the first 11 years, remained stable for 2 years, and then involuted.

Although the functional outcome may be more related to a tumor’s microanatomic relationships and remaining growth potential than to the operative approach, the various surgical options should be considered in planning management. Anterior and lateral orbitotomy approaches have been commonly used to remove cavernous hemangiomas, and an increased risk to vision associated with apical tumors in contact with the optic nerve has been duly noted. Scheuerle and associates described 14 “cavernomas” of the apex that were completely resected using a craniotomy approach. Eleven of 14 patients functionally improved or remained stable; 2 of 14 experienced severe, permanent postoperative decreases in vision; and 1 of 14 suffered a subdural hematoma and permanent frontal lobe syndrome. Tsirbas and associates reported visual improvement in a patient with an inferomedial, extraconal hemangioma that was removed through a combination of lower fornix and endoscopic transantral approaches. Almond and associates described endoscopic transethmoidal decompression of the medial orbital wall—without tumor resection—in 4 patients with presumed cavernous hemangiomas. In 3 of 4 cases, visual fields improved or did not worsen (in relatively brief postoperative intervals up to 33 months). In 1 of 4 cases, preoperative vision of 20/30 continued to deteriorate after decompression (to light perception before, and to no light perception after, craniotomy with tumor excision).
Management Recommendations
Considering the risk of unchecked tumor growth into apical structures—and the risk of tumor removal from them—each case requires thoughtful analysis.
If a lesion with imaging features typical for hemangioma is serendipitously found in a patient with normal ophthalmic findings, then continued observation is indicated. At the time of discovery, it is unknown whether the lesion is actively growing or has been stable for years, and without vision impairment, the risk of surgery outweighs any theoretical benefit. Patients can be followed with serial imaging and visual field testing. The latter may be the more sensitive indicator, since slight enlargement in the crowded apex is not easily appreciated in serial CT or magnetic resonance studies.
If there are major visual deficits at initial patient presentation, or minor deficits but evidence for active growth (eg, recent-onset or changing symptoms, deterioration in serial visual fields), then surgery should be considered. In such cases, there is no advantage to deferring the procedure, and earlier intervention may stave off more intimate fusion between the tumor and critical structures. However, there should be full disclosure of potential complications, including profound vision loss, diplopia, ptosis, corneal anesthesia, pupillary abnormality, loss of accommodation, and any risks specific to the chosen surgical pathway.
Unflagging loyalty to a particular surgical approach should be tempered by careful consideration of the tumor’s precise location. While microanatomic intimacy with the ophthalmic artery, optic nerve sheath, ciliary ganglion, and cranial nerves cannot be determined by imaging, macroanatomic relationships to the muscle cone, optic nerve, orbital fissures, paranasal sinuses, and cranial fossas all influence the approach. The desired pathway is one that will allow the most careful separation of tumor from the most critical structures.
The decision to intervene should not imply a commitment to complete resection at any price. Although intact removal is intuitively most satisfying, the intraoperative recognition of “inoperable” attachments may dictate modifications in order to preserve vision. Such decisions assume diagnostic confidence based on preoperative imaging and gross tumor appearance, and they take into account the benign nature of cavernous hemangiomas and their varied growth potential following intervention. Modifications might include subtotal resection, judicious shrinkage with bipolar cautery, and/or local decompression (eg, generous removal of bone and periorbita and relaxation of fascial septa). A few surgically inaccessible hemangiomas involving the cavernous sinus have been treated with stereotactic radiosurgery. Adjunctive use might be considered for orbital apex lesions that continue to grow despite the foregoing surgical measures.
Four representative cases demonstrate the role of tumor location in the choice of surgical approach. The fourth, in particular, emphasizes the impact of the surgical findings on intraoperative decisions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


