Purpose
To report a case of bilateral neovascular glaucoma with central retinal vein occlusions secondary to cosmetic iris implantation.
Design
Interventional case report.
Methods
setting: Tertiary care center; ophthalmology clinic. patient: A 25-year-old woman presented with persistent bilateral blurry vision after simultaneous bilateral cosmetic iris implantation. Examination showed best-corrected visual acuity of hand motion in the right and 20/400 in the left eye with intraocular pressures (IOP) of 48 mm Hg in the right and 40 mm Hg in the left eye on maximal medical therapy. She had bilateral neovascularization of the iris and angle with synechial angle closure, surgical aniridia, central retinal vein occlusion, and end-stage glaucomatous optic neuropathy. She was diagnosed with neovascular glaucoma in both eyes, associated with cosmetic iris implants. intervention procedures: Humphrey 24-2 visual field testing, optic nerve coherence tomography, and fundus imaging were performed. After bilateral intravitreal bevacizumab and panretinal photocoagulation, Ahmed glaucoma drainage devices were implanted in both eyes. main outcome measures: IOP, anterior chamber inflammation, neovascularization.
Results
Despite aggressive treatment, severe permanent bilateral vision loss ensued.
Conclusion
We strongly advise against the use of anterior chamber iris implants for cosmetic indications. Close monitoring of implanted individuals is necessary. Explantation should be considered at the earliest sign of adverse reaction.
The insertion of iris diaphragm silicone implants (NewColorIris; Kahn Medical Devices Corporation, Panama City, Panama) in the anterior chamber to change the appearance of the iris color has been recently offered as a permanent solution to cosmetic contact lenses. Internet advertisement states that over 700 procedures have been performed since 2002 with an incidence of chronic inflammation of 1.5% and raised intraocular pressures (IOP) that can be adequately controlled with eye drops (personal communication from NewColorIris). However, since 2008, there have been 4 reports of complications as a result of these implants that include increased IOP with or without glaucomatous changes, iritis with keratic precipitates, corneal edema, and hyphema, leading to decreased visual acuity. The severity of vision loss in these cases has been variable and mostly reversible. We report herein a case of devastating irreversible bilateral vision loss from neovascular glaucoma secondary to bilateral central retinal vein occlusion as a result of simultaneous implantation of these cosmetic iris diaphragms.
Case Report
A 25-year-old Hispanic woman traveled to Panama and underwent simultaneous bilateral eye surgery to change the color of her irides with non-FDA-approved anterior chamber cosmetic iris diaphragm implants (NewColorIris) ( Figure , Top row). Since the week following the surgery she complained of bilateral blurry vision, redness, tearing, and light sensitivity. Topical steroids for chronic iritis and IOP-lowering drops were prescribed by her surgeon during numerous postoperative visits back to Panama. Three months later, she consulted an ophthalmologist in the United States who recommended immediate explantation of the iris implants, but she did not follow this advice.
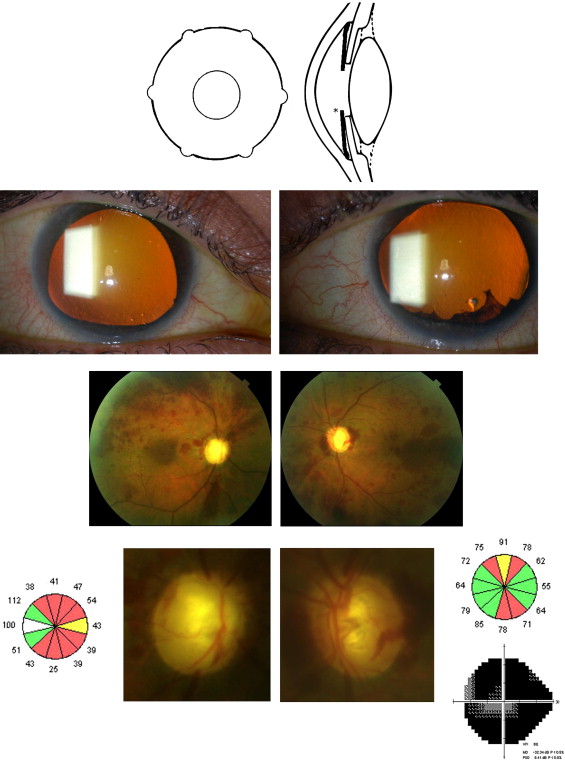
About 16 months after the implants were placed, the patient noticed a rapid decline of vision in both eyes and returned to Panama, where she was diagnosed with glaucoma and underwent removal of the implants by the original surgeon. A month later her best-corrected visual acuity (BCVA) had decreased to hand motion (HM) in the right and 20/400 in the left eye. IOP was 22 mm Hg in the right eye and 30 mm Hg in the left eye on latanoprost ophthalmic solution once at night (Xalatan 0.005%; Pfizer Inc, New York, New York, USA), brinzolamide ophthalmic suspension twice per day (Azopt 1%; Alcon Laboratories, Fort Worth, Texas, USA), and brimonidine ophthalmic solution twice per day (Alphagan P 0.1%; Allergan Inc, Irvine, California, USA) in both eyes. There was bilateral low-grade iritis, surgical aniridia ( Figure , Second row), and 1+ nuclear sclerosis. Gonioscopy revealed peripheral anterior synechiae and neovascularization of the angle and an inferior retracted hyphema. Fundoscopic examination showed minimal vitreous hemorrhage, advanced to end-stage glaucomatous optic neuropathy (right eye vertical cup-to-disc ratio 0.95, left eye 0.85), engorged retinal veins, macular edema, and numerous intraretinal hemorrhages throughout the fundus ( Figure , third row). She was diagnosed with bilateral central retinal vein occlusion and neovascular glaucoma at the referring practice and treated with intravitreal bevacizumab (Avastin; Genentech, San Francisco, California, USA) followed by panretinal photocoagulation (PRP). She was started on oral acetazolamide 500 mg twice a day for 5 days and referred to our glaucoma service when her IOP increased to 48 mm Hg in the right eye and 40 mm Hg in the left eye. There was mild corneal stromal edema with central corneal thicknesses of 602 μm in the right eye and 686 μm in the left eye, respectively. Endothelial counts by specular microscopy were 557 in the right eye and unobtainable in the left eye. Extensive thinning of the peripapillary retinal nerve fiber layer was confirmed by optical coherence tomography ( Figure , Bottom row) using Stratus OCT (Carl Zeiss Meditec, Dublin, California, USA). After informed consent, an Ahmed glaucoma drainage implant (New World Medical Inc, Rancho Cucamonga, California, USA) was urgently placed in the left eye, followed by the same procedure in the right eye within 1 week. Difluprednate ophthalmic suspension 4 times per day (Durezol 0.05%; Sirion Therapeutics, Tampa, Florida, USA) and brinzolamide ophthalmic suspension 3 times per day (Azopt 1%; Alcon Laboratories) were needed for three months after glaucoma drainage device implantation. Further PRP was added in both eyes to control neovascularization. After resolution of macular edema, her BCVA was hand motion in the right and 20/150 in the left eye with IOP in the mid teens bilaterally. Visual field analysis (HFA II model 750 operating system 12.6; Carl Zeiss Meditec, Jena, Germany) was unobtainable in the right eye and showed a small paracentral island in the left eye ( Figure , Bottom row).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


