TABLE 1.1 FDA-Approved Indications for Excimer Laser Refractive Surgery | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
and palpebral fissure height are adequate to accommodate a flap making apparatus. If the aperture is small or tight or if the eye is deep set, photorefractive keratectomy (PRK) may be a more preferable option.
the cause is not prior herpes simplex keratitis. Herpes viral infections can be reactivated by the ultraviolet radiation of the excimer laser. The presence of epithelial basement membrane dystrophy may indicate a possible defect in epithelial adhesion. Patients with this dystrophy are more likely to experience epithelial sloughing, possibly with diffuse lamellar keratitis or epithelial ingrowth. The risk of epithelial sloughing has been substantially reduced with the femtosecond laser. Patients with confluent guttae may be at risk for poor flap adhesion postoperatively, if the endothelial pump functions poorly. An abnormally thick cornea, especially in the early morning, may be a sign of abnormal endothelial pump function.
color vision, brightness comparison, and visual field. Obviously, some of this evaluation will already have been done before the retinal examination. Highly myopic patients often have tilted discs with peripapillary atrophy. The surgeon should rely on his or her own experience to determine if the appearance of the disc is inconsistent with the patient’s refractive error.
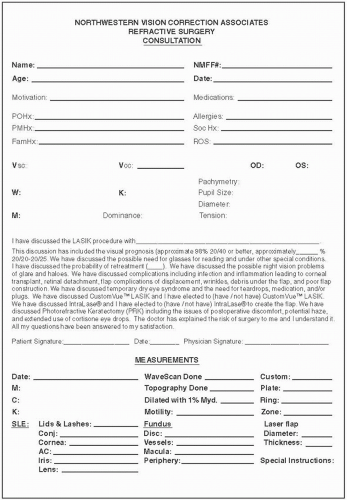
the refraction to stabilize. The wave scan will determine the degree and type of higher order aberrations. It also determines the refractive error in an objective way that can aid the surgeon when performing refraction. wave scan technology can be used postoperatively to assess the degree of higher order aberrations that may be induced by refractive surgery. The nuances of wave scan interpretation and custom LASIK as performed with several commonly used systems will be discussed later in the text.
appropriate and should raise a red flag about the candidacy of the particular patient. At this point it is helpful to remind the patient that LASIK reduces the dependence on glasses and contact lenses, but that glasses may be needed for reading when one reaches the mid-40s. “Correcting the dominant eye for distance and the nondominant eye for near, can reduce the need for reading glasses. This is called monovision.” This discussion is appropriate for patients of presbyopic age. “Glasses may also be needed for some distance activities, such as driving at night or in the rain, but it is rare for patients to require distance glasses full time.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree