Bacterial Conjunctivitis
Scott D. Barnes
C. Stephen Foster
Bacterial conjunctivitis affects all ages and is seen in all geographic locations, and it is the most common bacterial infection of the eye (1). Conjunctivitis may occur as a consequence of infection by viruses, bacteria, parasites, or fungi, and it may also occur as a consequence of trauma, malignancy, autoimmunity, allergy, and nonimmunologic skin conditions, such as acne rosacea. But the clinical characteristics of bacterial conjunctivitis are so typical of bacterial infections that one is rarely faced with some puzzling diagnostic dilemma when confronted by a patient with bacterial conjunctivitis. The one exception to this generalization occurs when the patient has chlamydial conjunctivitis, which is often chronic and which usually lacks the most tell-tale characteristic of most other bacterial infections of the outer eye, purulent discharge.
HISTORY
Purulent or catarrhal conjunctivitis has been recognized and written about by all developed societies, with clear descriptions in Chinese, Indian, Greek, and Egyptian writings extending back over the past 3500 years. The first written documentation of the recognition that it could be contagious probably dates from the early 18th century, and in the latter part of that century, Neisser, Koch, and Weekes identified the causative bacterial agents in patients with ophthalmia neonatorum and in patients with Egyptian ophthalmia.
EPIDEMIOLOGY
Precise data on the prevalence of bacterial conjunctivitis are difficult to obtain, but it is clear that it is more frequent in the young than in the elderly, and that it has seasonal peaks, with the winter and spring being the times of the year of highest reporting. The annual incidence among naval recruits in the 1980s was reported as 0.0025% of the population (2).
RISKS AND TRANSMISSION
As might be expected, the predominant risk for increased susceptibility to bacterial conjunctivitis includes systemic immunocompromise, local (ocular) immunocompromise (e.g., chronic use of topical steroid), and general debilitation (malnutrition, alcoholism). Transmission is most commonly from hand to eye, but can be from genitals to eye or from contiguous spread from nasolacrimal system or eyelid infection. Probably an underappreciated source of infestation is through the use of eye makeup harboring steadily increasing numbers of bacteria. And, finally, transfer of secretions from one person to another by flies or other insects, as in the case of transmission of trachoma in endemic areas, is a clear source of microbial transmission.
It is for this reason that this entity is the first to be addressed in this chapter, before moving on to the more “classic” bacterial infections that can produce bacterial conjunctivitis.
CHLAMYDIAL CONJUNCTIVITIS
Chronic follicular conjunctivitis (inclusion conjunctivitis) can be caused by chlamydia. The same serotypes (there are several, identifiable by monoclonal antibodies) that cause conjunctivitis in the adult can lead to neonatal conjunctivitis if an infected mother transmits the pathogen to the newborn during vaginal delivery. Repeated infections with Chlamydia trachomatis serotypes A, B, Ba, and C can cause trachoma, a chronic follicular keratoconjunctivitis that remains the most common cause of preventable blindness in the world. In addition, several cases of Parinaud’s oculoglandular syndrome have been reported with lymphogranuloma venereum, a sexually transmitted disease characterized by painful inguinal lymphadenopathy and caused by C. trachomatis serotypes L1 through L3.
Adult Inclusion Conjunctivitis
C. trachomatis can cause a chronic follicular conjunctivitis in adults and neonates. The adult form is usually sexually transmitted, with conjunctivitis developing in an estimated 1 in 300 patients with genital chlamydia (1), but it can occur with orogenital or hand-to-eye transmission of secretions (3). The
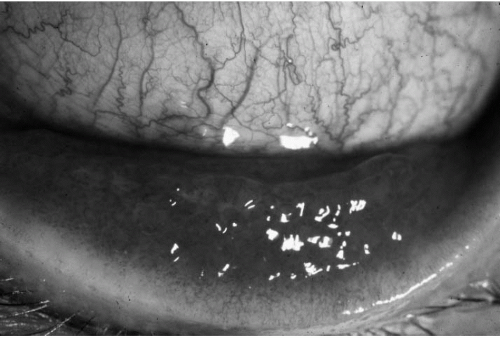
most common presentation is that of unilateral red eye (although it can be bilateral), preauricular adenopathy, papillary hypertrophy, marked hyperemia, mucopurulent discharge, and a follicular reaction (Fig. 13.2-1). Men often have a concomitant urethritis; women may have asymptomatic chronic cervicitis. Corneal involvement may quickly follow the conjunctivitis, resulting in punctate keratitis, epidemic keratoconjunctivitis-like infiltrates, and superior limbal pannus (neovascularization). Corneal scarring and neovascularization are less common with inclusion conjunctivitis than with trachoma, and the upper and lower palpebral conjunctiva are often equally involved as opposed to the preferentially affected upper conjunctiva in trachoma. However, severe inclusion conjunctivitis may be associated with a chronic, relapsing course leading to characteristics usually seen in trachoma.
most common presentation is that of unilateral red eye (although it can be bilateral), preauricular adenopathy, papillary hypertrophy, marked hyperemia, mucopurulent discharge, and a follicular reaction (Fig. 13.2-1). Men often have a concomitant urethritis; women may have asymptomatic chronic cervicitis. Corneal involvement may quickly follow the conjunctivitis, resulting in punctate keratitis, epidemic keratoconjunctivitis-like infiltrates, and superior limbal pannus (neovascularization). Corneal scarring and neovascularization are less common with inclusion conjunctivitis than with trachoma, and the upper and lower palpebral conjunctiva are often equally involved as opposed to the preferentially affected upper conjunctiva in trachoma. However, severe inclusion conjunctivitis may be associated with a chronic, relapsing course leading to characteristics usually seen in trachoma.
Treatment of Adult Inclusion Conjunctivitis
Because of the prominent mode of sexual transmission of this form of conjunctivitis, it is important simultaneously to treat all known partners. Failure to do so often results in more serious sequelae associated with reinfections. Topical antibiotics are relatively ineffective; systemic therapy is the mainstay of treatment. Tetracycline, doxycycline, azithromycin, ofloxacin or erythromycin are given for 3 weeks, with caution to avoid tetracycline in young children and pregnant or lactating women.
Trachoma
C. trachomatis serotypes A through C are responsible for trachoma. The severely blinding condition is endemic in many developing countries, especially in areas of close overcrowding and poor sanitation. Trachoma is usually the result of multiple untreated infections rather than a one-time event. The initial follicular conjunctivitis begins in the upper palpebral conjunctiva, followed by limbal follicles. Papillary hypertrophy, mucopurulent discharge, superior corneal pannus (neovascularization), and epithelial keratitis are early features of the disease. Later stages are marked by cicatrization of the conjunctiva, cornea, and eyelids.
Sequelae of Trachoma
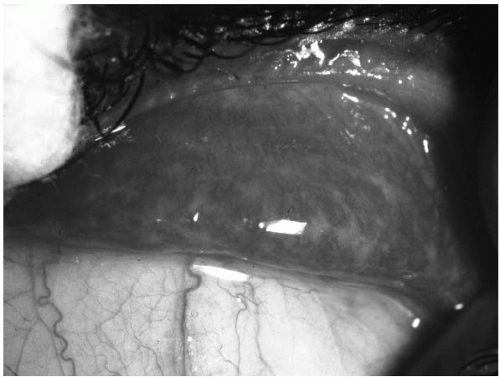
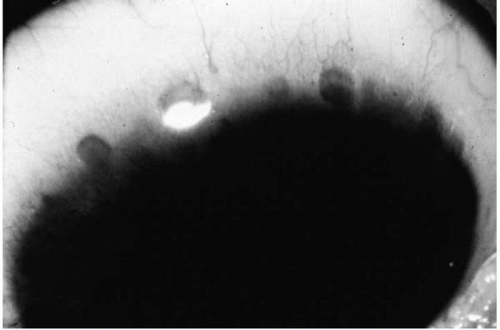
The blinding complications of trachoma are the result of the corneal exposure and ulceration due to the conjunctival scarring and lid deformities (4) (Fig. 13.2-2). Two classic findings are Arlt’s line and Hebert’s pits. Arlt’s line is the horizontal line of conjunctival scarring found along the superior palpebral conjunctiva (Fig. 13.2-3). Hebert’s pits are the sharply demarcated erosions near the limbus now filled with epithelium after the cicatrization of the limbal
follicles (Fig. 13.2-4). Once the regression of the superior pannus occurs, a diffuse corneal haze may be seen. Eyelid deformities are the result of the conjunctival scarring. Lids can be turned inward (entropion) or outward (ectropion) and lashes can be directed against the cornea (trichiasis), all of which contribute to an irregular ocular surface. Such irregularities can cause corneal scars, ulcers, neovascularization, and even perforation.
follicles (Fig. 13.2-4). Once the regression of the superior pannus occurs, a diffuse corneal haze may be seen. Eyelid deformities are the result of the conjunctival scarring. Lids can be turned inward (entropion) or outward (ectropion) and lashes can be directed against the cornea (trichiasis), all of which contribute to an irregular ocular surface. Such irregularities can cause corneal scars, ulcers, neovascularization, and even perforation.
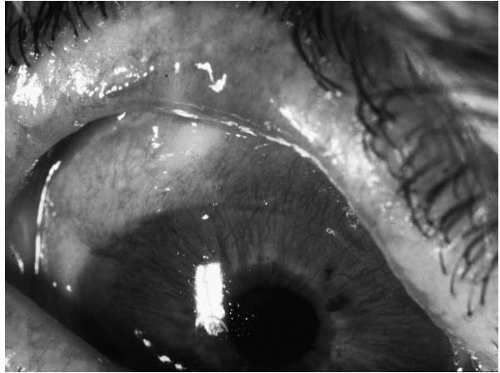 FIGURE 13.2-2. Cicatrizing conjunctivitis involving especially the tarsal conjunctiva in a patient with trachoma. |
Treatment of Trachoma
Systemic tetracycline or erythromycin is given for 3 weeks. The clinical response can often take several months; topical tetracycline or erythromycin is often used in endemic areas twice daily for 5 days each month for 6 months (5). This repeated topical treatment is especially useful in situations where repeat infection is likely. Loosely based on the smallpox eradication efforts, widespread prophylactic systemic antibiotics have been tried in endemic areas in an attempt to eliminate the disease. A single dose of azithromycin was proposed as a good choice for the eradication theory (6).
Lymphogranuloma Venereum
Certain serotypes of C. trachomatis (L1, L2, L3) have been associated with systemic lymphogranuloma venereum. The associated conjunctivitis is often mild and unilateral, producing a scant watery discharge. Although the conjunctivitis appears mild, there is rather impressive edema in the upper and lower eyelids. In addition to the usual preauricular lymphadenopathy, the nodes in the parotid and submaxillary region are also involved. There is a report of lymphogranuloma venereum conjunctivitis causing a keratitis leading to a corneal perforation in a patient with acquired immunodeficiency syndrome (7). Treatment is similar to that for inclusion conjunctivitis.
THE MORE CLASSIC CAUSES OF BACTERIAL CONJUNCTIVITIS
Patients with bacterial conjunctivitis usually present with a history of a rapid onset of unilateral lid edema, conjunctival hyperemia, and mucopurulent discharge. The opposite eye very often becomes involved with the same problem within 48 hours of the onset of the disorder. Staphylococcus and Corynebacterium species are the most common organisms to colonize the lids and conjunctiva and consequently are the most common causes of infectious conjunctivitis (8). Although almost any bacterial organism can cause conjunctivitis, the most common etiologies are Staphylococcus species, Streptococcus pneumoniae, Haemophilus species,
Moraxella, Corynebacterium diphtheriae, Neisseria species, and enteric gram-negative rods (9).
Moraxella, Corynebacterium diphtheriae, Neisseria species, and enteric gram-negative rods (9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree